Atenolol
Atenolol is a beta blocker medication primarily used to treat high blood pressure and heart-associated chest pain.[1] Atenolol, however, does not seem to improve mortality in those with high blood pressure.[2][3] Other uses include the prevention of migraines and treatment of certain irregular heart beats.[1][4] It is taken by mouth or by injection into a vein.[1][4] It can also be used with other blood pressure medications.[4]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tenormin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684031 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth, Intravenous (IV) |
| Drug class | Selective β1 receptor antagonist |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 40–50% |
| Protein binding | 6–16% |
| Metabolism | Liver <10% |
| Elimination half-life | 6–7 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.044.941 |
| Chemical and physical data | |
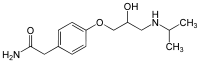
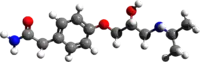
| Formula | C14H22N2O3 |
| Molar mass | 266.341 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Common side effects include feeling tired, heart failure, dizziness, depression, and shortness of breath.[1] Other serious side effects include bronchospasm.[1] Use is not recommended during pregnancy[1] and alternative drugs are preferred when breastfeeding.[5] It works by blocking β1-adrenergic receptors in the heart, thus decreasing the heart rate and workload.[1]
Atenolol was patented in 1969 and approved for medical use in 1975.[6] It is available as a generic medication.[1] In 2017, it was the 36th most commonly prescribed medication in the United States, with more than 20 million prescriptions.[7][8]
Medical uses
Atenolol is used for a number of conditions including hypertension, angina, long QT syndrome, acute myocardial infarction, supraventricular tachycardia, ventricular tachycardia, and the symptoms of alcohol withdrawal.[9]
The role for β-blockers in general in hypertension was downgraded in June 2006 in the United Kingdom, and later in the United States, as they are less appropriate than other agents such as ACE inhibitors, calcium channel blockers, thiazide diuretics and angiotensin receptor blockers, particularly in the elderly.[10][11][12]
Side effects
Atenolol was the main β-blocker identified as carrying a higher risk of provoking type 2 diabetes, leading to its downgrading in the United Kingdom in June 2006 to fourth-line agent in the management of hypertension.[11]
Antihypertensive therapy with atenolol provides weaker protective action against cardiovascular complications (e.g. myocardial infarction and stroke) compared to other antihypertensive medications. In some cases, diuretics are superior.[13]
Overdose
Symptoms of overdose are due to excessive pharmacodynamic actions on β1 and also β2-receptors. These include bradycardia (slow heartbeat), severe hypotension with shock, acute heart failure, hypoglycemia and bronchospastic reactions. Treatment is largely symptomatic. Hospitalization and intensive monitoring is indicated. Activated charcoal is useful to absorb the drug. Atropine will counteract bradycardia, glucagon helps with hypoglycemia, dobutamine can be given against hypotension and the inhalation of a β2-mimetic as hexoprenalin or salbutamol will terminate bronchospasms. Blood or plasma atenolol concentrations may be measured to confirm a diagnosis of poisoning in hospitalized patients or to assist in a medicolegal death investigation. Plasma levels are usually less than 3 mg/L during therapeutic administration, but can range from 3–30 mg/L in overdose victims.[14][15]
Society and culture
Atenolol has been given as an example of how slow healthcare providers are to change their prescribing practices in the face of medical evidence that indicates that a drug is not as effective as others in treating some conditions.[16] In 2012, 33.8 million prescriptions were written to American patients for this drug.[16] In 2014, it was in the top (most common) 1% of drugs prescribed to Medicare patients.[16] Although the number of prescriptions has been declining steadily since limited evidence articles contesting its efficacy was published, it has been estimated that it would take 20 years for doctors to stop prescribing it for hypertension.[16] Despite its diminished efficacy when compared to newer antihypertensive drugs, atenolol and other beta blockers still a relevant clinical choice for treating some conditions, since beta blockers are a diverse group of medicines with different properties that still requires further research.[10] As consequence, reasons for the popularity of beta blockers cannot be fully attributed to a slow healthcare system – patient compliance factor, such as treatment cost and duration, also affect adherence and popularity of therapy.[17]
References
- "Atenolol Monograph for Professionals". Drugs.com. AHFS. Retrieved 23 December 2018.
- Tomiyama H, Yamashina A (2014). "Beta-Blockers in the Management of Hypertension and/or Chronic Kidney Disease". International Journal of Hypertension. 2014: 919256. doi:10.1155/2014/919256. PMC 3941231. PMID 24672712.
- DiNicolantonio JJ, Fares H, Niazi AK, Chatterjee S, D'Ascenzo F, Cerrato E, Biondi-Zoccai G, Lavie CJ, Bell DS, O'Keefe JH (2015). "β-Blockers in hypertension, diabetes, heart failure and acute myocardial infarction: a review of the literature". Open Heart. 2 (1): e000230. doi:10.1136/openhrt-2014-000230. PMC 4371808. PMID 25821584.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 151–153. ISBN 9780857113382.
- "Atenolol use while Breastfeeding". Drugs.com. Retrieved 23 December 2018.
- Fischer, Janos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 461. ISBN 9783527607495.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Atenolol - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- "Atenolol". The American Society of Health-System Pharmacists. Retrieved 8 May 2018.
- Wiysonge, CS; Bradley, HA; Volmink, J; Mayosi, BM; Opie, LH (January 2017). "Beta-blockers for hypertension". Cochrane Database of Systematic Reviews. 1: 3. doi:10.1002/14651858.CD002003.pub5. PMC 5369873. PMID 28107561.
Further research should be of high quality and should explore whether there are differences between different subtypes of beta-blockers or whether beta-blockers have differential effects on younger and older people [...] Beta-blockers were not as good at preventing the number of deaths, strokes, and heart attacks as other classes of medicines such as diuretics, calcium-channel blockers, and renin-angiotensin system inhibitors. Most of these findings come from one type of beta-blocker called atenolol. However, beta-blockers are a diverse group of medicines with different properties, and we need more well-conducted research in this area." (p. 2-3)
- Sheetal Ladva (28 June 2006). "NICE and BHS launch updated hypertension guideline". National Institute for Health and Clinical Excellence. Archived from the original on 11 May 2008. Retrieved 19 August 2012.
- Cruickshank, JM (August 2007). "Are we misunderstanding beta-blockers". International Journal of Cardiology. 120 (1): 10–27. doi:10.1016/j.ijcard.2007.01.069. PMID 17433471.
- Carlberg B, Samuelsson O, Lindholm LH (2004). "Atenolol in hypertension: is it a wise choice?". The Lancet. 364 (9446): 1684–9. doi:10.1016/S0140-6736(04)17355-8. PMID 15530629.
- DeLima LG, Kharasch ED, Butler S (1995). "Successful pharmacologic treatment of massive atenolol overdose: sequential hemodynamics and plasma atenolol concentrations". Anesthesiology. 83 (1): 204–207. doi:10.1097/00000542-199507000-00025. PMID 7605000.
- R. Baselt (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, Calif.: Biomedical Publications. pp. 116–117.
- Epstein, David; ProPublica (22 July 2017). "When Evidence Says No, But Doctors Say Yes". The Atlantic. Retrieved 8 May 2018.
- Choi, Hyo Yoon; Oh, Im Jung; Lee, Jung Ah; Lim, Jisun; Kim, Young Sik; Jeon, Tae-Hee; Cheong, Yoo-Seock; Kim, Dae-Hyun; Kim, Moon-Chan; Lee, Sang Yeoup. "Factors Affecting Adherence to Antihypertensive Medication". Korean Journal of Family Medicine. 39 (6): 325–332. doi:10.4082/kjfm.17.0041. ISSN 2005-6443. PMC 6250947. PMID 30384549.
External links
- "Atenolol". Drug Information Portal. U.S. National Library of Medicine.
