Dexamethasone
Dexamethasone is a corticosteroid medication[6] used to treat rheumatic problems, a number of skin diseases, severe allergies, asthma, chronic obstructive lung disease, croup, brain swelling, eye pain following eye surgery, and along with antibiotics in tuberculosis.[6] In adrenocortical insufficiency, it may be used in combination with a mineralocorticoid medication such as fludrocortisone.[6] In preterm labor, it may be used to improve outcomes in the baby.[6] It may be given by mouth, as an injection into a muscle, as an injection into a vein, as a topical cream or ointment for the skin or as a topical ophthalmic solution to the eye.[6] The effects of dexamethasone are frequently seen within a day and last for about three days.[6]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Dextenza, Ozurdex, Neofordex, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682792 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous therapy (IV), intramuscular injection (IM), subcutaneous injection (SC), intraosseous (IO), eye drop |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 80–90% |
| Protein binding | 77% |
| Metabolism | Liver |
| Elimination half-life | biological half-life: 36 to 54 hours; plasma half-life: 4 to 5 hours[4][5] |
| Excretion | Urine (65%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.004 |
| Chemical and physical data | |
| Formula | C22H29FO5 |
| Molar mass | 392.467 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 262 °C (504 °F) |
| |
| |
| | |
The long-term use of dexamethasone may result in thrush, bone loss, cataracts, easy bruising, or muscle weakness.[6] It is in pregnancy category C in the United States, meaning that it should only be used when the benefits are predicted to be greater than the risks.[1] In Australia, the oral use is category A, meaning it has been frequently used in pregnancy and not been found to cause problems to the baby.[7] It should not be taken when breastfeeding.[6] Dexamethasone has anti-inflammatory and immunosuppressant effects.[6]
Dexamethasone was first made in 1957 by Philip Showalter Hench and was approved for medical use in 1961.[8][9][10] It is on the World Health Organization's List of Essential Medicines.[11] In 2017, it was the 321st most commonly prescribed medication in the United States, with more than one million prescriptions.[12]
Medical uses

Anti-inflammatory
Dexamethasone is used to treat many inflammatory and autoimmune disorders, such as rheumatoid arthritis and bronchospasm.[13] Idiopathic thrombocytopenic purpura, a decrease in numbers of platelets due to an immune problem, responds to 40 mg daily for four days; it may be administered in 14-day cycles. It is unclear whether dexamethasone in this condition is significantly better than other glucocorticoids.[14]
It is also given in small amounts[15] before and/or after some forms of dental surgery, such as the extraction of the wisdom teeth, an operation which often causes puffy, swollen cheeks.
Dexamethasone is commonly given as a treatment for croup in children, as a single dose can reduce the swelling of the airway to improve breathing and reduce discomfort.[16]
It is injected into the heel when treating plantar fasciitis, sometimes in conjunction with triamcinolone acetonide.
It is useful to counteract allergic anaphylactic shock, if given in high doses.
It is present in certain eye drops – particularly after eye surgery – and as a nasal spray, and certain ear drops (can be combined with an antibiotic and an antifungal). Dexamethasone intravitreal steroid implants have been approved by the FDA to treat ocular conditions such as diabetic macular edema, central retinal vein occlusion, and uveitis.[17] Dexamethasone has also been used with antibiotics to treat acute endophthalmitis.[18]
Dexamethasone is used in transvenous screw-in cardiac pacing leads to minimize the inflammatory response of the myocardium. The steroid is released into the myocardium as soon as the screw is extended and can play a significant role in minimizing the acute pacing threshold due to the reduction of inflammatory response. The typical quantity present in a lead tip is less than 1.0 mg.
Dexamethasone may be administered before antibiotics in cases of bacterial meningitis. It acts to reduce the inflammatory response of the body to the bacteria killed by the antibiotics (bacterial death releases proinflammatory mediators that can cause a response which is harmful), thus reducing hearing loss and neurological damage.[19]
Cancer
People with cancer undergoing chemotherapy are often given dexamethasone to counteract certain side effects of their antitumor treatments. Dexamethasone can increase the antiemetic effect of 5-HT3 receptor antagonists, such as ondansetron.[20] The exact mechanism of this interaction is not well-defined, but it has been theorized that this effect may be due to, among many other causes, inhibition of prostaglandin synthesis, anti-inflammatory effects, immunosuppressive effects, decreased release of endogenous opioids, or a combination of the aforementioned.[21]
In brain tumors (primary or metastatic), dexamethasone is used to counteract the development of edema, which could eventually compress other brain structures. It is also given in cord compression, where a tumor is compressing the spinal cord.
Dexamethasone is also used as a direct chemotherapeutic agent in certain hematological malignancies, especially in the treatment of multiple myeloma, in which dexamethasone is given alone or in combination with other chemotherapeutic drugs, including most commonly with thalidomide (Thal-dex), lenalidomide, bortezomib (Velcade, Vel-dex),[22] or a combination of doxorubicin (Adriamycin) and vincristine or bortezomib/lenalidomide/dexamethasone.
COVID‑19
Dexamethasone is recommended by the National Health Service in the UK and the National Institutes of Health (NIH) in the US for patients with COVID-19 who need either mechanical ventilation or supplemental oxygen (without ventilation).[23][24] Dexamethasone is otherwise not recommended.[23][24][25]
The Infectious Diseases Society of America (IDSA) guideline panel suggests the use of glucocorticoids for patients with severe COVID-19, defined as patients with SpO2 ≤94% on room air, and those who require supplemental oxygen, mechanical ventilation, or extracorporeal membrane oxygenation (ECMO).[26] The IDSA recommends against the use of glucocorticoids for those with COVID‑19 without hypoxemia requiring supplemental oxygen.[26]
The World Health Organization (WHO) recommends systemic corticosteroids rather than no systemic corticosteroids for the treatment of people with severe and critical COVID-19 (strong recommendation, based on moderate certainty evidence).[25] The WHO suggests not to use corticosteroids in the treatment of people with non-severe COVID-19 (conditional recommendation, based on low certainty evidence).[25]
A meta-analysis of seven clinical trials of critically ill COVID-19 patients, each treated with one of three different corticosteroids found a statistically significant reduction in death.[27] The largest reduction was obtained with dexamethasone (36% compared to placebo).[27][28]
In September 2020, the European Medicines Agency (EMA) endorsed the use of dexamethasone in adults and adolescents (from twelve years of age and weighing at least 40 kg) who require supplemental oxygen therapy.[29] Dexamethasone can be taken by mouth or given as an injection or infusion (drip) into a vein.[29]
Endocrine
Dexamethasone is the treatment for the very rare disorder of glucocorticoid resistance.[30][31]
In adrenal insufficiency and Addison's disease, dexamethasone is prescribed when the patient does not respond well to prednisone or methylprednisolone.
It can be used in congenital adrenal hyperplasia in older adolescents and adults to suppress ACTH production. It is typically given at night.[32]
Pregnancy
Dexamethasone may be given to women at risk of delivering prematurely to promote maturation of the fetus' lungs. This administration, given from day to one week before delivery, has been associated with low birth weight, although not with increased rates of neonatal death.[33]
Dexamethasone has also been used during pregnancy as an off-label prenatal treatment for the symptoms of congenital adrenal hyperplasia (CAH) in female babies. CAH causes a variety of physical abnormalities, notably ambiguous genitalia. Early prenatal CAH treatment has been shown to reduce some CAH symptoms, but it does not treat the underlying congenital disorder. This use is controversial: it is inadequately studied, only around one in ten of the fetuses of women treated are at risk of the condition, and serious adverse events have been documented.[34] Experimental use of dexamethasone in pregnancy for fetal CAH treatment was discontinued in Sweden when one in five cases suffered adverse events.[35]
A small clinical trial found long-term effects on verbal working memory among the small group of children treated prenatally, but the small number of test subjects means the study cannot be considered definitive.[36][37]
High-altitude illnesses
Dexamethasone is used in the treatment of high-altitude cerebral edema (HACE), as well as high-altitude pulmonary edema (HAPE). It is commonly carried on mountain-climbing expeditions to help climbers deal with complications of altitude sickness.[38][39]
Nausea and vomiting
Intravenous dexamethasone is effective for prevention of nausea and vomiting in people who had surgery and whose post-operative pain was treated with long-acting spinal or epidural spinal opioids.[40]
The combination of dexamethasone and a 5-HT3 receptor antagonist such as ondansetron is more effective than a 5-HT3 receptor antagonist alone in preventing postoperative nausea and vomiting.[41]
Sore throat
A single dose of dexamethasone or another steroid speeds improvement of a sore throat.[42]
Contraindications
Contraindications of dexamethasone include,[43][44] but are not limited to:
- Uncontrolled infections
- Known hypersensitivity to dexamethasone
- Cerebral malaria
- Systemic fungal infection
- Concurrent treatment with live virus vaccines (including smallpox vaccine)
Adverse effects
The exact incidence of the adverse effects of dexamethasone are not available, hence estimates have been made as to the incidence of the adverse effects below based on the adverse effects of related corticosteroids and on available documentation on dexamethasone.[44][45][46][47][48]
Common
- Acne
- Insomnia
- Vertigo
- Increased appetite
- Weight gain
- Impaired skin healing
- Depression
- Euphoria
- Hypertension
- Increased risk of infection
- Raised intraocular pressure
- Vomiting
- Dyspepsia
- Confusion
- Amnesia
- Irritability
- Nausea
- Malaise
- Headaches
- Cataract (in cases of long-term treatment it occurs in about 10% of patients)
Unknown frequency
- Papilledema
- Adrenal suppression
- Growth stunting (in children)
- Cushing's syndrome
- Peptic ulcer
- Osteoporosis
- Myopathy
- Diabetes mellitus type 2
- Hyperglycaemia
- Pancreatitis (inflammation of the pancreas)
- Sodium and water retention
- Mania
- Psychosis
- Glaucoma
- Cardiomyopathy
- Abdominal distension
- Corneal or scleral thinning
- Candidiasis
- Skin atrophy
- Bruising
- Telangiectasia
- Striae
- Leukocytosis
- Thromboembolism
- Psychological dependence
- Vertebral collapse
- Oesophageal ulcer
- Seizures
- Hypertriglyceridaemia
- Intracranial hypertension (long-term treatment)
- Facial plethora
- Hypokalaemia
- Hypocalcaemia
- Muscular atrophy
- Nitrogen depletion due to protein catabolism
- Allergic reactions including anaphylaxis
Withdrawal
Sudden withdrawal after long-term treatment with corticosteroids can lead to:[44]
- Adrenal insufficiency
- Hypotension
- Fever
- Myalgia
- Arthralgia
- Rhinitis
- Conjunctivitis
- Painful itchy skin nodules
- Weight loss
- Death
Interactions
Known drug interactions include:[44]
- Inducers of hepatic microsomal enzymes such as barbiturates, phenytoin, and rifampicin can reduce the half-life of dexamethasone.
- Cotreatment with oral contraceptives can increase its volume of distribution.
Pharmacology
As a glucocorticoid, dexamethasone is an agonist of the glucocorticoid receptor (GR). It has minimal mineralocorticoid activity.[49][50][51]
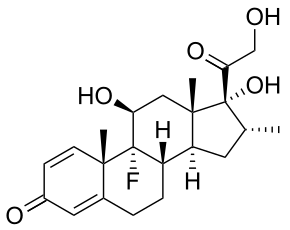
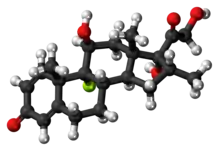
Chemistry
Dexamethasone is a synthetic pregnane corticosteroid and derivative of cortisol (hydrocortisone) and is also known as 1-dehydro-9α-fluoro-16α-methylhydrocortisone or as 9α-fluoro-11β,17α,21-trihydroxy-16α-methylpregna-1,4-diene-3,20-dione.[52][53] The molecular and crystal structure of dexamethasone has been determined by X-ray crystallography.[54] It is a stereoisomer of betamethasone, the two compounds differing only in the spatial configuration of the methyl group at position 16 (see steroid nomenclature).[55]
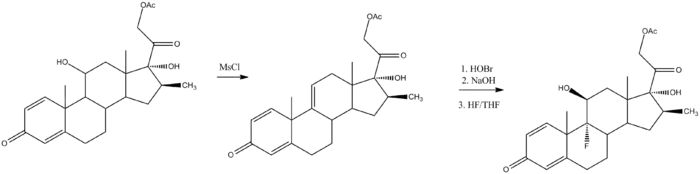
Synthesis
To synthesize dexamethasone, 16β-methylprednisolone acetate is dehydrated to the 9,11-dehydro derivative.[56][57] This is then reacted with a source of hypobromite, such as basic N-bromosuccinimide, to form the 9α-bromo-11β-hydrin derivative, which is then ring-closed to an epoxide. A ring-opening reaction with hydrogen fluoride in tetrahydrofuran gives dexamethasone.
History
Dexamethasone was first synthesized by Philip Showalter Hench in 1957.[8][9] It was introduced for medical use in 1958.[50]
On 16 June 2020, the RECOVERY Trial announced preliminary results stating that dexamethasone improves survival rates of hospitalized patients with COVID‑19 receiving oxygen or on a ventilator. Benefits were only observed in patients requiring respiratory support; those who did not require breathing support saw a worse survival rate than the control group, although the difference may have been due to chance.[58] A preprint containing the full dataset was published on 22 June 2020 and demand for dexamethasone surged after publication of the preprint.[59] The preliminary report was published in The New England Journal of Medicine on 18 July 2020.[60]
The World Health Organization (WHO) states that dexamethasone should be reserved for seriously ill and critical patients receiving COVID‑19 treatment in a hospital setting,[61] and the WHO Director-General stated that "WHO emphasizes that dexamethasone should only be used for patients with severe or critical disease, under close clinical supervision. There is no evidence this drug works for patients with mild disease or as a preventative measure, and it could cause harm."[62] In July 2020, the WHO stated they are in the process of updating treatment guidelines to include dexamethasone or other steroids.[63] In September 2020, the WHO released updated guidance on using corticosteroids for COVID‑19.[25]
In July 2020, the European Medicines Agency (EMA) started reviewing results from the RECOVERY study arm that involved the use of dexamethasone in the treatment of patients with COVID‑19 admitted to the hospital to provide an opinion on the results and in particular the potential use of dexamethasone for the treatment of adults with COVID-19.[64][65] In September 2020, the EMA received an application for marketing authorization of dexamethasone for COVID‑19.[66]
Society and culture
Price
Dexamethasone is inexpensive.[67] In the United States a month of medication is typically priced less than US$25.[6] In India, a course of treatment for preterm labor is about US$0.50.[67] The drug is available in most areas of the world.[67]
Nonmedical use
Dexamethasone is given in legal Bangladesh brothels to prostitutes not yet of legal age, causing weight gain aimed at making them appear older and healthier to customers and police.[68]
Dexamethasone and most glucocorticoids are banned by sporting bodies including the World Anti-Doping Agency.[69]
Veterinary use
Combined with marbofloxacin and clotrimazole, dexamethasone is available under the name Aurizon, CAS number 115550-35-1, and used to treat difficult ear infections, especially in dogs. It can also be combined with trichlormethiazide to treat horses with swelling of distal limbs and general bruising.[70]
See also
References
- "Dexamethasone Use During Pregnancy". Drugs.com. Archived from the original on 17 May 2016. Retrieved 9 June 2016.
Dexamethasone is only recommended for use during pregnancy when there are no alternatives and benefit outweighs risk.
- "Ozurdex EPAR". European Medicines Agency (EMA). Retrieved 24 October 2020.
- "Neofordex EPAR". European Medicines Agency (EMA). Retrieved 24 October 2020.
- Dogra P, Vijayashankar NP (14 September 2020). "Dexamethasone Suppression Test". StatPearls (September 14, 2020). PMID 31194457.
- Jobe AH, Milad MA, Peppard T, Jusko WJ (March 2020). "Pharmacokinetics and Pharmacodynamics of Intramuscular and Oral Betamethasone and Dexamethasone in Reproductive Age Women in India". Clinical and Translational Science. 13 (2): 391–99. doi:10.1111/cts.12724. PMC 7070803. PMID 31808984.
- "Dexamethasone". The American Society of Health-System Pharmacists. Archived from the original on 31 August 2017. Retrieved 29 July 2015.
- "Prescribing medicines in pregnancy database". Australian Government. 3 March 2014. Archived from the original on 8 April 2014. Retrieved 22 April 2014.
Drugs which have been taken by a large number of pregnant women and women of childbearing age without any proven increase in the frequency of malformations or other direct or indirect harmful effects on the fetus having been observed.
- "Dexamethasone". 17 June 2020.
- Rankovic Z, Hargreaves R, Bingham M (2012). Drug discovery and medicinal chemistry for psychiatric disorders. Cambridge: Royal Society of Chemistry. p. 286. ISBN 9781849733656. Archived from the original on 5 March 2016.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 485. ISBN 9783527607495.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "Dexamethasone – Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- Till J. "Paramedic Clinical Training Aid". Archived from the original on 31 March 2012. Retrieved 30 August 2011.
- Provan D, Stasi R, Newland AC, Blanchette VS, Bolton-Maggs P, Bussel JB, et al. (January 2010). "International consensus report on the investigation and management of primary immune thrombocytopenia". Blood. 115 (2): 168–86. doi:10.1182/blood-2009-06-225565. PMID 19846889.
- Schmelzeisen R, Frölich JC (1993). "Prevention of postoperative swelling and pain by dexamethasone after operative removal of impacted third molar teeth". European Journal of Clinical Pharmacology. 44 (3): 275–77. doi:10.1007/BF00271371. PMID 8491244. S2CID 12528750.
- "Croup – Diagnosis & Treatment". Mayo Clinic. Retrieved 13 October 2017.
Dexamethasone is usually recommended because of its long-lasting effects (up to 72 hours).
- Brady CJ, Villanti AC, Law HA, Rahimy E, Reddy R, Sieving PC, et al. (February 2016). "Corticosteroid implants for chronic non-infectious uveitis". Cochrane Database of Systematic Reviews. 2: CD010469. doi:10.1002/14651858.CD010469.pub2. PMC 5038923. PMID 26866343.
- Kim CH, Chen MF, Coleman AL (February 2017). "Adjunctive steroid therapy versus antibiotics alone for acute endophthalmitis after intraocular procedure". Cochrane Database of Systematic Reviews. 2: CD012131. doi:10.1002/14651858.CD012131.pub2. PMC 5419424. PMID 28225198.
- Brouwer MC, McIntyre P, Prasad K, van de Beek D (September 2015). "Corticosteroids for acute bacterial meningitis". Cochrane Database of Systematic Reviews (9): CD004405. doi:10.1002/14651858.CD004405.pub5. PMC 6491272. PMID 26362566.
- Roila F, Ballatori E, Ruggeri B, DeAngelis V (May 2000). "Dexamethasone alone or in combination with ondansetron for the prevention of delayed nausea and vomiting induced by chemotherapy". The New England Journal of Medicine. 342 (21): 1554–59. doi:10.1056/NEJM200005253422102. PMID 10824073.
- Holte K, Kehlet H (November 2002). "Perioperative single-dose glucocorticoid administration: pathophysiologic effects and clinical implications". Journal of the American College of Surgeons. 195 (5): 694–712. doi:10.1016/s1072-7515(02)01491-6. PMID 12437261.
- Harousseau JL, Attal M, Leleu X, Troncy J, Pegourie B, Stoppa AM, et al. (November 2006). "Bortezomib plus dexamethasone as induction treatment prior to autologous stem cell transplantation in patients with newly diagnosed multiple myeloma: results of an IFM phase II study". Haematologica. 91 (11): 1498–505. PMID 17043025.

- "Dexamethasone and COVID-19". SPS – Specialist Pharmacy Service. Retrieved 22 July 2020.
- "Corticosteroids". COVID-19 Treatment Guidelines. National Institutes of Health. Retrieved 12 July 2020.
- World Health Organization (2020). Corticosteroids for COVID-19: living guidance, 2 September 2020 (Report). World Health Organization. hdl:10665/334125. WHO/2019-nCoV/Corticosteroids/2020.1. Lay summary.
- "COVID-19 Guideline, Part 1: Treatment and Management". Infectious Diseases Society of America. Retrieved 22 July 2020.
Recommendation 4. Among hospitalized patients with severe* COVID-19, the IDSA guideline panel suggests glucocorticoids rather than no glucocorticoids. (Conditional recommendation, Moderate certainty of evidence)
Remark: Dexamethasone 6 mg IV or PO for 10 days (or until discharge if earlier) or equivalent glucocorticoid dose may be substituted if dexamethasone unavailable. Equivalent total daily doses of alternative glucocorticoids to dexamethasone 6 mg daily are methylprednisolone 32 mg and prednisone 40 mg.
Recommendation 5. Among hospitalized patients with COVID-19 without hypoxemia requiring supplemental oxygen, the IDSA guideline panel suggests against the use of glucocorticoids. (Conditional recommendation, Low certainty of evidence) - Sterne JA, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, et al. (The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group) (September 2020). "Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis". JAMA. 324 (13): 1330–1341. doi:10.1001/jama.2020.17023. PMC 7489434. PMID 32876694. S2CID 221467783.
- Prescott HC, Rice TW (September 2020). "Corticosteroids in COVID-19 ARDS: Evidence and Hope During the Pandemic". JAMA. 324 (13): 1292–1295. doi:10.1001/jama.2020.16747. PMID 32876693. S2CID 221468015.
- "EMA endorses use of dexamethasone in COVID-19 patients on oxygen or mechanical ventilation". European Medicines Agency (EMA) (Press release). 18 September 2020. Retrieved 21 September 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- Chrousos GP, Detera-Wadleigh SD, Karl M (December 1993). "Syndromes of glucocorticoid resistance" (PDF). Annals of Internal Medicine. 119 (11): 1113–24. doi:10.7326/0003-4819-119-11-199312010-00009. PMID 8239231. S2CID 26040431. Archived from the original (PDF) on 14 August 2017. Retrieved 4 July 2020.
- Charmandari E, Kino T, Ichijo T, Chrousos GP (May 2008). "Generalized glucocorticoid resistance: clinical aspects, molecular mechanisms, and implications of a rare genetic disorder". The Journal of Clinical Endocrinology and Metabolism. 93 (5): 1563–72. doi:10.1210/jc.2008-0040. PMC 2386273. PMID 18319312.
- Dan L. Longo, Anthony Fauci, Dennis Kasper, Stephen Hauser, J. Jerry Jameson and Joseph Loscalzo, Harrison's Principles of Internal Medicine, 18th edition, p. 3055
- Bloom SL, Sheffield JS, McIntire DD, Leveno KJ (April 2001). "Antenatal dexamethasone and decreased birth weight". Obstetrics and Gynecology. 97 (4): 485–90. doi:10.1016/S0029-7844(00)01206-0. PMID 11275014. S2CID 33601749.
- Elton C (18 June 2010). "A Prenatal Treatment Raises Questions of Medical Ethics". Archived from the original on 31 August 2016 – via content.time.com.
- Hirvikoski T, Nordenström A, Wedell A, Ritzén M, Lajic S (June 2012). "Prenatal dexamethasone treatment of children at risk for congenital adrenal hyperplasia: the Swedish experience and standpoint". The Journal of Clinical Endocrinology and Metabolism. 97 (6): 1881–83. doi:10.1210/jc.2012-1222. PMID 22466333.
- Hirvikoski T, Nordenström A, Lindholm T, Lindblad F, Ritzén EM, Wedell A, Lajic S (February 2007). "Cognitive functions in children at risk for congenital adrenal hyperplasia treated prenatally with dexamethasone". The Journal of Clinical Endocrinology and Metabolism. 92 (2): 542–48. doi:10.1210/jc.2006-1340. PMID 17148562.
- Lajic S, Nordenström A, Hirvikoski T (2011). "Long-term outcome of prenatal dexamethasone treatment of 21-hydroxylase deficiency". Endocrine Development. 20: 96–105. doi:10.1159/000321228. ISBN 978-3-8055-9643-5. PMID 21164263.
- Cymerman A, Rock PB (1994). "Medical Problems in High Mountain Environments. A Handbook for Medical Officers" (PDF). USARIEM-TN94-2. US Army Research Inst. of Environmental Medicine Thermal and Mountain Medicine Division Technical Report. Archived from the original (PDF) on 17 June 2017. Retrieved 17 June 2020. Cite journal requires
|journal=(help) - Eledrisi MS (April 2007). "First-line therapy for hypertension". Annals of Internal Medicine. 146 (8): 615. doi:10.7326/0003-4819-146-8-200704170-00021. PMID 17438328.
- Grape S, Usmanova I, Kirkham KR, Albrecht E (April 2018). "Intravenous dexamethasone for prophylaxis of postoperative nausea and vomiting after administration of long-acting neuraxial opioids: a systematic review and meta-analysis". Anaesthesia. 73 (4): 480–89. doi:10.1111/anae.14166. PMID 29226971.
- Kovac AL (May 2006). "Meta-analysis of the use of rescue antiemetics following PONV prophylactic failure with 5-HT3 antagonist/dexamethasone versus single-agent therapies". The Annals of Pharmacotherapy. 40 (5): 873–87. doi:10.1345/aph.1G338. PMID 16670361. S2CID 32843029.
- Sadeghirad B, Siemieniuk RA, Brignardello-Petersen R, Papola D, Lytvyn L, Vandvik PO, et al. (September 2017). "Corticosteroids for treatment of sore throat: systematic review and meta-analysis of randomised trials". BMJ. 358: j3887. doi:10.1136/bmj.j3887. PMC 5605780. PMID 28931508.
- "Decadron, Dexamethasone Intensol (dexamethasone) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 12 December 2013. Retrieved 11 December 2013.
- "Product Information Dexamethsone (dexamethasone)" (PDF). TGA eBusiness Services. Aspen Pharmacare Australia Pty Ltd. 10 August 2010. Retrieved 11 December 2013. (Accept terms and conditions to open PDF, which doesn't work in archived version)
- "Product Information Dexmethsone Injection" (PDF). TGA eBusiness ServicesAspen Pharmacare Australia Pty Ltd. Aspen Pharmacare Australia Pty Ltd. 2 March 2011. Retrieved 11 December 2013. (Accept terms and conditions to open PDF, which doesn't work in archived version)
- "Dexamethasone tablet [ECR Pharmaceuticals]". DailyMed. ECR Pharmaceuticals. December 2010. Archived from the original on 13 December 2013. Retrieved 11 December 2013.
- "Dexamethasone Tablet BP 2.0 mg – Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Merck Sharp & Dohme Limited. 26 January 2018. Retrieved 17 June 2020.
- "Dexamethasone 4.0 mg/ml injection – Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Merck Sharp & Dohme Limited. 4 December 2013. Archived from the original on 8 May 2015. Retrieved 11 December 2013.
- De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Nicolaides NC, Pavlaki AN, Maria Alexandra MA, Chrousos GP (2000). "Glucocorticoid Therapy and Adrenal Suppression". PMID 25905379. Cite journal requires
|journal=(help) - Khan MO, Park KK, Lee HJ (2005). "Antedrugs: an approach to safer drugs". Current Medicinal Chemistry. 12 (19): 2227–39. doi:10.2174/0929867054864840. PMID 16178782.
- Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, Brown JP, Cohen A, Kim H (August 2013). "A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy". Allergy, Asthma, and Clinical Immunology. 9 (1): 30. doi:10.1186/1710-1492-9-30. PMC 3765115. PMID 23947590.
- Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 366–. ISBN 978-1-4757-2085-3. Archived from the original on 15 February 2017.
- Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 310–. ISBN 978-3-88763-075-1. Archived from the original on 24 August 2017.
- Raynor JW, Minor W, Chruszcz M (2007). "Dexamethasone at 119 K". Acta Crystallographica Section E. 63 (6): o2791–93. doi:10.1107/S1600536807020806.
- Antignac, Jean-Philippe; Le Bizec, Bruno; Monteau, Fabrice; Andre, François (2002). "Differentiation of betamethasone and dexamethasone using liquid chromatography/positive electrospray tandem mass spectrometry and multivariate statistical analysis". Journal of mass spectrometry: JMS. 37 (1): 69–75. doi:10.1002/jms.260. ISSN 1076-5174. PMID 11813313.
- Arth GE, Fried J, Johnston DBR, Hoff DR, Sarett HL, Silber RH, Stoerk HC, Winter CA (1958). "16-Methylated steroids. II. 16α-Methyl analogs of cortisone, a new group of anti-inflammatory steroids. 9α-Halo derivatives". Journal of the American Chemical Society. 80 (12): 3161–63. doi:10.1021/ja01545a063.
- Taub D, Hoffsommer RD, Slates HL, lWendler NL (1958). "16β-Methyl cortical steroids". Journal of the American Chemical Society. 80 (16): 4435. doi:10.1021/ja01549a095.
- "Dexamethasone in COVID-19" (PDF). www.gpni.co.uk. 16 June 2020. Retrieved 18 June 2020.
- Mahase E (June 2020). "Covid-19: Demand for dexamethasone surges as RECOVERY trial publishes preprint". BMJ. 369: m2512. doi:10.1136/bmj.m2512. PMID 32576548.
- Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. (July 2020). "Dexamethasone in Hospitalized Patients with Covid-19 – Preliminary Report". New England Journal of Medicine. doi:10.1056/NEJMoa2021436. PMC 7383595. PMID 32678530.
- "Important to use dexamethasone only for serious COVID cases – WHO". 17 June 2020. Retrieved 18 June 2020.
- "WHO Director-General's opening remarks at the media briefing on COVID-19". World Health Organization. 22 June 2020. Retrieved 26 June 2020.
- "Q&A: Dexamethasone and COVID-19". World Health Organization (WHO). Retrieved 12 July 2020.
- "EMA starts review of dexamethasone for treating adults with COVID-19 requiring respiratory support". European Medicines Agency (EMA) (Press release). 24 July 2020. Retrieved 27 July 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- "EMA to review results from study testing common steroid drug against COVID-19". Reuters. 24 July 2020. Retrieved 27 July 2020.
- "EMA receives application for marketing authorisation of Dexamethasone Taw COVID-19". European Medicines Agency (EMA). 2 September 2020. Retrieved 2 September 2020.
- "Dexamethasone for Accelerating Lung Maturation in Preterm Babies" (PDF). Archived (PDF) from the original on 22 December 2015. Retrieved 29 July 2015.
- Dummett M (30 May 2010). "Bangladesh's dark brothel steroid secret". BBC News Online. Archived from the original on 22 February 2012.
- "Prohibited In-Competition: Glucocorticoids". World Anti-Doping Agency.
- "Trichlormethiazide and Dexamethasone for veterinary use". Wedgewood Pharmacy. Archived from the original on 12 December 2007. Retrieved 23 January 2008.
External links
| Wikimedia Commons has media related to Dexamethasone. |
- "Dexamethasone". Drug Information Portal. U.S. National Library of Medicine.
- "Dexamethasone Ophthalmic". MedlinePlus.
- "Dexamethasone Injection". MedlinePlus.