Digital health
Digital health, which includes digital care programs, is the convergence of digital technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery[1][2] and make medicine more personalized and precise.[3] The discipline involves the use of information and communication technologies to help address the health problems and challenges faced by people under treatment.[3] These technologies include both hardware and software solutions and services, including telemedicine, wearable devices, augmented reality, and virtual reality.[4][5] Generally, digital health is concerned about the development of interconnected health systems to improve the use of computational technologies, smart devices, computational analysis techniques, and communication media to aid healthcare professionals and their patients manage illnesses and health risks, as well as promote health and wellbeing.[3][5] Although digital health platforms hold a number of possible benefits, critics warn against potential privacy violations of personal health data and the role digital health could play in increasing the health and digital divide between social majority and minority groups. Worldwide adoption of electronic medical records has been on the rise since 1990 and is closely correlated with the existence of universal health care.[6] Digital health is a multi-disciplinary domain involving many stakeholders, including clinicians, researchers and scientists with a wide range of expertise in healthcare, engineering, social sciences, public health, health economics and data management.[7]
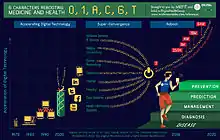
Elements
As an outgrowth of the Digital Revolution characterized by "the mass production and widespread use of digital logic circuits, and its derived technologies, including the computer, digital cellular phone, and the Internet,"[8] key elements of digital health include wireless devices, hardware sensors and software sensing technologies, microprocessors and integrated circuits, the Internet, social networking, mobile/cellular networks and body area networks, health information technology, genomics, and personal genetic information.[3][5][7][9][10]
Technologies
Digital health technologies come in many different forms and extend into various parts of healthcare. As new technologies develop, digital health, as a field, respectively transforms. The three most popular domains of digital health technologies include telemedicine, wearable technologies, and augmented and virtual reality. Telemedicine is how physicians treat patients remotely and the different technologies needed to make the process more efficient and faster.[11] The other main side of digital health is data collection and how to provide on-demand medical information for patients, which gave rise to wearables. Wearable technologies hold the promise of bringing personalized data and health-related tracking to all users.[12] In terms of digitized treatment, augmented and virtual reality can create personalized regimens for patients that can be repeated and tailored to treat many conditions.[13]
In fact some of these technologies are being propelled by the startup space, which has been followed via Internet or online media sources such as podcasts on digital health entrepreneurs.
Telemedicine
Telemedicine is one the broadest areas of digital health. It encompasses the digitization of medical records, remote care, appointment booking, self-symptom checkers, patient outcome reporting, and many others.[11] Digital and remote clinics are commonly used to provide quick, nonurgent consultations that save both the patients and doctors time.[11] Especially with the COVID-19 pandemic, this type of treatment has become the primary way doctors are seeing their patients and has proven to be very successful.[14] This type of digital treatment keeps both parties safe and is a reliable method that physicians plan to use for routine checks even after the pandemic ends.[14]
Telemedicine also covers online health records, where both patients and doctors have access to the relevant information at all times.[11] All this digital information means that patient data is accessible to healthcare professions and can be analyzed to create better and smarter treatment plans.[11] This paves the path for a more personalized healthcare system, which can help patients better understand their conditions and could result in more positive outcomes.[11]
Wearable technology
Wearable technology comes in many forms, including smartwatches and on-body sensors. Smartwatches were one of the first wearable devices that promoted self-monitoring and were typically associated with fitness tracking.[15] Many record health-related data, such as "body mass index, calories burnt, heart rate, physical activity patterns".[15] Beyond smartwatches, researchers are developing smart-related bodywear, like patches, clothes, and accessories, to administer "on-demand drug release".[12] This technology can expand into smart implants for both severe and non-severe medical cases, where doctors will be able to create better, dynamic treatment protocols that would not have been possible without such mobile technology.[12]
These technologies are used to gather data on patients at all times during the day.[12] Since doctors no longer need to have their patients come into the office to collect the necessary data, the data can lead to better treatment plans and patient monitoring.[12] Doctors will have better knowledge into how well a certain medication is performing.[12] They will also be able to continuously learn from this data and improve upon their original treatment plans to intervene when needed.[12]
Augmented and virtual reality
In digital health, augmented reality technology enhances real-world experiences with computerized sensory information and is used to build smart devices for healthcare professionals.[16] Since the majority of patient-related information now comes from hand-held devices, smart glasses provide a new, hands-free augmented way for a doctor to view their patient's medical history.[16] The applications of this technology can extend into data-driven diagnosis, augmented patient documentation, or even enhanced treatment plans, all by wearing a pair of smart glasses when treating a patient.[16]
Another similar technology space is virtual reality, which creates interactive simulations that mimic real-life scenarios and can be tailored for personalized treatments.[13] Many stroke victims lose range of motion and under standard treatment protocols; 55% to 75% of patients have long-term upper muscular dysfunction, as the lower body is primarily targeted during therapy.[13] Repeated actions and the length of therapy are the two main factors that show positive progress towards recovery.[13] Virtual reality technologies can create various 3D environments that are difficult to replace in real-life but are necessary to help patients retrain their motor movements.[13] These simulations can not only target specific body parts, but can also increase in intensity as the patient improves and requires more challenging tasks.[13]
Others
Some other technologies include Assistive technologies, rehabilitation robotics, and unobtrusive monitoring sensors that can help people with disabilities perform their daily tasks independently. Computational simulations, modeling, and machine learning (e.g. FG-AI4H) approaches can model health-related outcomes.[17] These advanced simulations are able to be repeated, replicated, and tailored to any research area.[17] In medical imaging, the applications for this technology helps healthcare professionals visualize genes, brain structures, and many other components of human anatomy.[17] The flexibility in this technology also allows for more positive and accurate results.[17] Mobile health (or mhealth) is the practice of medicine and public health supported by mobile devices.[18]
Health systems engineering is another subset of digital health that leverages other engineering industries to improve upon applications include knowledge discovery, decision making, optimization, human factors engineering, quality engineering, and information technology and communication. Speech and hearing systems for natural language processing, speech recognition techniques, and medical devices can aid in speech and hearing (e.g. cochlear implants).[19] Digital hearing aids use various algorithms to reduce background noises and improve perceptual performance, which is a significant improvement from regular hearing implants.[19]
Implementation
National electronic health record (EHR) systems National digital programs exist to support healthcare, form meaningful indicators, and facilitate population-based studies by providing clinically procured data in an open-source and standardized digital format. These can inform public health decisions, which are especially crucial in low-resource settings.[20] The World Health Organization's Global Observatory for eHealth (GOe) conducts and reports a worldwide survey of its 194 member nations on their progress towards EHR implementation as well as universal healthcare coverage. In their latest issue in 2015, 73 Members (58%) responded with having some eHealth strategy in place, a count that has increased since 1990.[6] Within this cohort, high-income countries are overrepresented, as well as the majority are countries with universal health care (UHC).
National digital programs exist to support healthcare, such as those of Canada Health Infoway built on core systems of patient and provider registries, clinical and diagnostic imaging systems, clinical reports and immunizations.[21] By 2014, 75% of Canadian physicians were using electronic medical records.[22]
In Uganda and Mozambique, partnerships between patients with cell phones, local and regional governments, technologists, non-governmental organizations, academia, and industry have enabled mHealth solutions.[23]
In the United Kingdom, the National Health Service (NHS) has commissioned a report on how to integrate digital healthcare technologies into the next generation of medicine.[24] The "Topol Review" recommended an expansion of education for both patients and providers of next-generation technologies such as Whole Genome Sequencing, and has also created Digital Fellowships for health professionals.[25]
On the other hand, the implementation of these innovations has also brought to light societal risks and regulatory needs, which are certainly challenging the current governance structures in the health sector.
Innovation cycle
The innovation process for digital health is an iterative cycle for technological solutions that can be classified into five main activity processes from the identification of the healthcare problem, research, digital solution, and evaluating the solution, to implementation in working clinical practices.[3][4] Digital health may incorporate methods and tools adopted by software engineering, such as design thinking and agile software development.[26][27] These commonly follow a user-centered approach to design, which are evaluated by subject-matter experts in their daily life using real-world data.[27]
U.S. Food and Drug Administration
In 2019, the FDA published a Digital Health Innovation Action Plan that would reduce inefficiencies for physicians in an effort to cut overhead costs, improve access, increase quality of service, and make medicine more easily adapted for each person.[5] Topics within the innovation plan are wireless devices, telemedicine, software, and cybersecurity, among others.[5] According to FDA guidelines, if you release an app designed to help someone with a medical condition then that is considered a medical device. The FDA cannot regulate all healthcare apps, so they use "enforcement discretion", and up until 2020, have chosen not to regulate all digital care programs and apps. However, programs that use the word treatment, seek to diagnose or treat a condition, or are deemed unsafe, are and will be regulated by the FDA.[28] During the COVID-19 pandemic, regulations and enforcement of digital psychiatry apps were relaxed to facilitate use and reduce in-person contact.[29]
International Standards
At an intergovernmental level, the World Health Organization is the United Nations Specialized Agency for health, and the International Telecommunication Union is the UN Specialized Agency for ICTs, the Agencies collaborate in their work on digital health, such as the H.870 standard on safe listening, as well as the ITU-WHO Focus Group on Artificial Intelligence for Health, a subsidiary of the ITU-T Study Group 16.
Criticisms
Digital healthcare has been a major focus of American healthcare policy after the passage of the Affordable Care Act and HITECH Act.[30] This has resulted in an explosion in the number of physicians who interface with digital healthcare tools known as Electronic Medical Records (EMRs).[31] However, physicians are highly critical of the utility of EMRs for patient care, and point to their rising use as a significant component in physician burnout.[32][33][31]
The ownership of health data issue
At a global level, the implementation of digital health solutions depends on large data sets, ranging from simple statistics that record every birth and death to more sophisticated metrics that track diseases, outbreaks, and chronic conditions. These systems record data such as patient records, blood test results, EKGs, MRIs, billing records, drug prescriptions, and other private medical information. Medical professionals can use this data to make more data-driven decisions about patient care and consumers themselves can utilize it to make informed choices about their own health.[34] Given the personal nature of the data being collected, a crucial debate has arisen amongst stake-holders about one of the challenges induced by digital health solutions: the ownership of health data.[35] In most cases, governments and big data and technology companies are storing citizens' medical information, leaving many concerned with how their data is being used and/or who has access to it.[35] This is further compounded by the fact that the details that answer these questions is oftentimes hidden in complex terms & conditions that are rarely read.[35] A notable example of a data privacy breach in the digital health space took place in 2016.[36] Google faced a major lawsuit over a data-sharing agreement that gave its artificial intelligence arm, DeepMind, access to the personal health data of 1.6 million British patients.[36] Google failed to secure patient consent and guarantee the anonymity of the patients.[36] Another concept is that data is considered as a form of public good. Researchers from Stanford University proposed the use of such a framework, to think about data and the development of AI; they were thinking about radiology data specifically. [37] They concluded that clinical data should be a form of public good, used for the benefit of future patients and that the data should be widely available for the development of knowledge and tools to benefit future patients. From this, they drew three main conclusions. Firstly, if the clinical data is really not owned by anyone, those who interact with it then have an obligation to ensure that the data is used for the benefit of future patients in societies. Secondly, this data should be widely shared for research and development, and all the individuals and entities with access to that data, then essentially become stewards of that data and become responsible to carefully safeguard the privacy and to ensure that the data is used for developing knowledge and tools for the good. Thirdly, patient consent wouldn’t necessarily be required before the data is used for secondary purposes, such as AI development and training and testing, as long as there are mechanisms in place to ensure that ethical standards are being followed. According to this proposed framework, the authors propose that it would be unethical to sell data to the third parties by granting exclusive access in exchange for monetary or any kind of payments that exceed costs.
Misinterpretation of data
Although the data and information provided by personalized health platforms may give reassurance to users, they might simultaneously induce increased anxiety and obsessive behavior.[38] As seen with platforms like WebMD, the misinterpretation of data can further contribute to patient hysteria: having increased access to information on oneself is not always positive.[38] In an extreme scenario, patients might feel a misplaced sense of security knowing that they have this access, meaning that they won't seek medical advice or help from professionals, even if it may be needed.[39]
Institutional ageism
Ageism is defined as the process of systemic discrimination against the elderly.[40] As digital health becomes more prevalent in our society, those who lack strong digital skills and the technical know-how needed to navigate these platforms will be put at a disadvantage.[41] This doesn't just apply to current seniors.[41] New digital technologies become popularized every year rendering older technology obsolete.[41] This means that this digital divide will always be present, unless health companies actively work to try to minimize this gap.[41] Not to mention, seniors are more prone to chronic health issues, meaning that they are one of the groups that has the greatest need for a digital health platform.[42] They represent an untapped user group.[42]
Digital divide
19 million people in the US do not have reliable connectivity access.[43] Worldwide, the UN estimates that 3.8 billion people are offline.[44] Those in rural communities and with lower levels of education lack significant barriers, like lack of reliable broadband and lack of basic digital literacy, required to use many digital health platforms.[38] As a result, the already existing health gap between low-income and high-income populations may become further exacerbated by up and coming health technologies.[38] To be effective, digital health solutions must foster the development of health literacy skills amongst platform users to make sure that the technology is used as intended[45]
Bio-surveillance risks
In the age of the COVID-19 pandemic, the use of digital health platforms as a means to contain the spread of the disease has been accelerated worldwide.[46] In South Korea for instance, the government strictly tracks the smartphone location of those who have been infected to make sure they obey quarantine guidelines.[47] Programs like this are being implemented across the world in countries such as Italy,[46] China,[47] Poland, and more.[46] Although beneficial in combating spread, critics worry about the potential loss of civil liberties associated with individuals handing over their private health data to government entities, and whether these "reduced regulations" will stay in place in a post-pandemic world.[47]
Lack of existing regulation
The COVID-19 Pandemic has brought to light the lack of existing regulation that exists in the digital health space.[48] When looking at Electronic Health Record platforms (EHR), the Health Insurance Portability and Accountability Act(HIPPA) of 1996 was the first comprehensive framework that aimed to protect the personal data of patients.[48] It was recently amended in 2009 with the Health Information Technology for Economic and Clinical Health (HITECH) Act which seeks to examine personal health data privacy laws through the lens of the private sector and increase enforcement of HIPPA.[48] Critics of these acts claim that they don't go far enough as there are still around 600,000 types of businesses that can access patient data without explicit consent.[48] Not to mention, there are extensive reports proving that HIPPA regulations are constantly violated, making some wonder whether the government even has the capacity to enforce the laws that they put in place.[49] With major companies like Facebook and Apple moving into digital health, critics question whether existing regulations are comprehensive enough.[50]
References
- O’Donoghue, John; Majeed, Azeem; Carroll, Christopher; Gallagher, Joseph; Wark, Petra A.; O’Connor, Siobhan; Akinlua, James Tosin; Fadahunsi, Kayode Philip (1 March 2019). "Protocol for a systematic review and qualitative synthesis of information quality frameworks in eHealth". BMJ Open. 9 (3): e024722. doi:10.1136/bmjopen-2018-024722. ISSN 2044-6055. PMC 6429947. PMID 30842114.
- Chen, Connie E.; Harrington, Robert A.; Desai, Sumbul A.; Mahaffey, Kenneth W.; Turakhia, Mintu P. (1 June 2019). "Characteristics of Digital Health Studies Registered in ClinicalTrials.gov". JAMA Internal Medicine. 179 (6): 838–840. doi:10.1001/jamainternmed.2018.7235. ISSN 2168-6106. PMC 6547144. PMID 30801617.
- Bhavnani, Sanjeev P.; Narula, Jagat; Sengupta, Partho P. (7 May 2016). "Mobile technology and the digitization of healthcare". European Heart Journal. 37 (18): 1428–38. doi:10.1093/eurheartj/ehv770. PMC 4914890. PMID 26873093.
- Widmer, R. Jay; Collins, Nerissa M.; Collins, C. Scott; West, Colin P.; Lerman, Lilach O.; Lerman, Amir (April 2015). "Digital Health Interventions for the Prevention of Cardiovascular Disease: A Systematic Review and Meta-Analysis". Mayo Clinic Proceedings. 90 (4): 469–80. doi:10.1016/j.mayocp.2014.12.026. PMC 4551455. PMID 25841251.
- "Digital health". US Food and Drug Administration. 19 July 2019. Retrieved 23 September 2019.
- "WHO | Global diffusion of eHealth: Making universal health coverage achievable". WHO. Retrieved 5 November 2020.
- O’Donoghue, John; Herbert, John (1 October 2012). "Data Management within mHealth Environments: Patient Sensors, Mobile Devices, and Databases". Journal of Data and Information Quality. 4 (1): 1–20. doi:10.1145/2378016.2378021. S2CID 2318649.
- Rafael, Perez-Uribe; Carlos, Salcedo-Perez; David, Ocampo-Guzman (13 April 2018). Handbook of Research on Intrapreneurship and Organizational Sustainability in SMEs. IGI Global. ISBN 9781522535447.
- Topol, Eric J. (2012). The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care. Basic Books. ISBN 978-0-465-02550-3. OCLC 868260493 – via Internet Archive.
- Iyawa, G E; Herselman, M; Botha, A (2016), "Digital Health Innovation Ecosystems: From Systematic Literature Review to Conceptual Framework", Procedia Computer Science, 100: 244–252, doi:10.1016/j.procs.2016.09.149
- Miedany, Yasser El- (1 January 2017). "Telehealth and telemedicine: how the digital era is changing standard health care". Smart Homecare Technology and TeleHealth. 4: 43–52. doi:10.2147/SHTT.S116009.
- Amft, O. (January 2018). "How Wearable Computing Is Shaping Digital Health". IEEE Pervasive Computing. 17 (1): 92–98. doi:10.1109/MPRV.2018.011591067. ISSN 1558-2590. S2CID 3921043.
- Merians, Alma S.; Jack, David; Boian, Rares; Tremaine, Marilyn; Burdea, Grigore C.; Adamovich, Sergei V.; Recce, Michael; Poizner, Howard (1 September 2002). "Virtual reality--augmented rehabilitation for patients following stroke. (Case Report)". Physical Therapy. 82 (9): 898–916. doi:10.1093/ptj/82.9.898.
- Monaghesh, Elham; Hajizadeh, Alireza (1 August 2020). "The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence". BMC Public Health. 20 (1): 1193. doi:10.1186/s12889-020-09301-4. ISSN 1471-2458. PMC 7395209. PMID 32738884.
- Rich, Emma; Miah, Andy (2 January 2017). "Mobile, wearable and ingestible health technologies: towards a critical research agenda". Health Sociology Review. 26 (1): 84–97. doi:10.1080/14461242.2016.1211486. ISSN 1446-1242. S2CID 151558809.
- Klinker, Kai; Wiesche, Manuel; Krcmar, Helmut (25 June 2019). "Digital Transformation in Health Care: Augmented Reality for Hands-Free Service Innovation". Information Systems Frontiers. 22 (6): 1419–1431. doi:10.1007/s10796-019-09937-7. ISSN 1572-9419. S2CID 195330313.
- Chang, Victor (January 2018). "Computational Intelligence for Medical Imaging Simulations". Journal of Medical Systems. 42 (1): 10. doi:10.1007/s10916-017-0861-x. ISSN 0148-5598. PMID 29177790. S2CID 13049464.
- Silva, Bruno M. C.; Rodrigues, Joel J. P. C.; de la Torre Díez, Isabel; López-Coronado, Miguel; Saleem, Kashif (August 2015). "Mobile-health: A review of current state in 2015". Journal of Biomedical Informatics. 56: 265–272. doi:10.1016/j.jbi.2015.06.003. ISSN 1532-0480. PMID 26071682.
- Jiang, Tao; Liang, Ruiyu; Wang, Qinqyun; Bao, Yongqiang (March 2018). "Speech Noise Reduction Algorithm in Digital Hearing Aids Based on an Improved Sub-band SNR Estimation". Circuits, Systems, and Signal Processing. 37 (3): 1243–1267. doi:10.1007/s00034-017-0605-7. ISSN 0278-081X. S2CID 3484142.
- Fritz, Fleur; Tilahun, Binyam; Dugas, Martin (1 March 2015). "Success criteria for electronic medical record implementations in low-resource settings: a systematic review". Journal of the American Medical Informatics Association. 22 (2): 479–488. doi:10.1093/jamia/ocu038. ISSN 1067-5027. PMID 25769683.
- "Progress in Canada". Canada Health Infoway. 2016. Archived from the original on 12 November 2016. Retrieved 11 November 2016.
- Collier, Roger (6 January 2015). "National Physician Survey: EMR use at 75%". Canadian Medical Association Journal. 187 (1): E17-8. doi:10.1503/cmaj.109-4957. PMC 4284187. PMID 25487665.
- Källander, Karin; Tibenderana, James K.; Akpogheneta, Onome J.; Strachan, Daniel L.; Hill, Zelee; ten Asbroek, Augustinus H.A.; Conteh, Lesong; Kirkwood, Betty R.; Meek, Sylvia R. (25 January 2013). "Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: A review". Journal of Medical Internet Research. 15 (1): e17. doi:10.2196/jmir.2130. PMC 3636306. PMID 23353680.

- "Topol review". Health Education England. 21 February 2018. Retrieved 8 March 2020.
- "The Topol Review". The Topol Review – NHS Health Education England. Retrieved 8 March 2020.
- Plattner, Hasso; Schapranow, Matthieu-P., eds. (2013). High-Performance In-Memory Genome Data Analysis. Springer.
- Benjamin, Katherine; Potts, Henry WW (27 February 2018). "Digital transformation in government: Lessons for digital health?". Digital Health. 4: 205520761875916. doi:10.1177/2055207618759168. ISSN 2055-2076. PMC 6005404. PMID 29942624.
- FDA (26 September 2019). "Examples of Software Functions for Which the FDA Will Exercise Enforcement Discretion". U.S. Food and Drug Administration. Retrieved 8 June 2020.
- Health, Center for Devices and Radiological (16 April 2020). "Enforcement Policy for Digital Health Devices For Treating Psychiatric Disorders During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency". U.S. Food and Drug Administration. Retrieved 30 July 2020.
- Agrawal, Raag; Prabakaran, Sudhakaran (5 March 2020). "Big data in digital healthcare: lessons learnt and recommendations for general practice". Heredity. 124 (4): 525–534. doi:10.1038/s41437-020-0303-2. ISSN 0018-067X. PMC 7080757. PMID 32139886.
- Journal of Clinical Pharmacy and Therapeutics. 42 (1). February 2017. doi:10.1111/jcpt.2017.42.issue-1. ISSN 0269-4727 //doi.org/10.1111%2Fjcpt.2017.42.issue-1. Missing or empty
|title=(help) - Daniel Essin, M. A. (6 February 2012). "Improve EHR Systems by Rethinking Medical Billing". Physicians Practice. Retrieved 8 March 2020.
- Gawande, Atul. "Why Doctors Hate Their Computers". The New Yorker. Retrieved 8 March 2020.
- Health, Center for Devices and Radiological (22 September 2020). "What is Digital Health?". FDA.
- Torous, John; Roberts, Laura Weiss (05 01, 2017). "Needed Innovation in Digital Health and Smartphone Applications for Mental Health: Transparency and Trust". JAMA Psychiatry. 74 (5): 437–438. doi:10.1001/jamapsychiatry.2017.0262. ISSN 2168-6238. PMID 28384700. Check date values in:
|date=(help) - Sharon, Tamar (1 July 2018). "When digital health meets digital capitalism, how many common goods are at stake?". Big Data & Society. 5 (2): 2053951718819032. doi:10.1177/2053951718819032. ISSN 2053-9517. S2CID 150255521.
- Template:Authors = Larson DB, Magnus DC, Lungren MP, Shah NH, Langlotz CP.
- Lupton, Deborah (2014). "Critical Perspectives on Digital Health Technologies". Sociology Compass. 8 (12): 1344–1359. doi:10.1111/soc4.12226. ISSN 1751-9020.
- Becker, Stefan; Miron-Shatz, Talya; Schumacher, Nikolaus; Krocza, Johann; Diamantidis, Clarissa; Albrecht, Urs-Vito (2014). "mHealth 2.0: Experiences, Possibilities, and Perspectives". JMIR mHealth and uHealth. 2 (2): e24. doi:10.2196/mhealth.3328. PMC 4114478. PMID 25099752.
- Lloyd-Sherlock, Peter G.; Ebrahim, Shah; McKee, Martin; Prince, Martin James (31 August 2016). "Institutional ageism in global health policy". BMJ. 354: i4514. doi:10.1136/bmj.i4514. ISSN 1756-1833. PMID 27582131. S2CID 41312322.
- "The Effect of Ageism on the Digital Divide Among Older Adults". heraldopenaccess.us. Retrieved 3 November 2020.
- Loader, Brian D. (13 January 2009). Digital Welfare for the Third Age. doi:10.4324/9780203886533. ISBN 9780203886533.
- "Eighth Broadband Progress Report". Federal Communications Commission. 21 August 2012. Retrieved 3 November 2020.
- "Press Release". www.itu.int. Retrieved 3 November 2020.
- Dunn, Patrick; Hazzard, Eric (10 15, 2019). "Technology approaches to digital health literacy". International Journal of Cardiology. 293: 294–296. doi:10.1016/j.ijcard.2019.06.039. ISSN 1874-1754. PMID 31350037. Check date values in:
|date=(help) - "The rise of the bio-surveillance state". www.newstatesman.com. Retrieved 3 November 2020.
- "Coronavirus bio-surveillance around the globe". Big Think. 27 March 2020. Retrieved 3 November 2020.
- Solove, Daniel J. (4 April 2013). "HIPAA Turns 10: Analyzing the Past, Present, and Future Impact". Rochester, NY. SSRN 2245022. Cite journal requires
|journal=(help) - Miron-Scahtz, Talya; Elwyn, Glyn (30 June 2011). "To serve and protect? Electronic health records pose challenges for privacy, autonomy and person-centered medicine". International Journal of Person Centered Medicine. 1 (2): 405–409. doi:10.5750/ijpcm.v1i2.84.
- Sharon, Tamar (18 July 2020). "Blind-sided by privacy? Digital contact tracing, the Apple/Google API and big tech's newfound role as global health policy makers". Ethics and Information Technology: 1–13. doi:10.1007/s10676-020-09547-x. ISSN 1388-1957. PMC 7368642. PMID 32837287.