East Kent Hospitals University NHS Foundation Trust
East Kent Hospitals University NHS Foundation Trust is one of the largest hospital trusts in England. It runs the Kent and Canterbury Hospital (Canterbury), William Harvey Hospital (Ashford), Queen Elizabeth The Queen Mother Hospital (Margate), Buckland Hospital (Dover), and the Royal Victoria Hospital (Folkestone) - and some outpatient facilities in the East Kent and Medway areas in England.
| East Kent Hospitals University NHS Foundation Trust | |
|---|---|
 | |
| Type | NHS foundation trust |
| Established | 1 March 2009 |
| Headquarters | Kent and Canterbury Hospital |
| Region served | Kent |
| Population | 695,000 |
| Hospitals | |
| Chair | Stephen Smith |
| Chief executive | Susan Acott |
| Staff | 8,045 |
| Website | www |
It serves a local population of around 759,000 people. It is a teaching trust involved in the education and training of doctors, nurses and other healthcare professionals, with King's College London and, since 2018, Kent and Medway Medical School.[1]
Development
The Trust, with Maidstone and Tunbridge Wells NHS Trust was jointly procuring an electronic patient record system in a contract worth £10m - £40m in December 2013.[2]
In April 2014 it was reported that the Trust was looking for a partner to develop a private hospital at the William Harvey Hospital site and enhance the returns from the Spencer private hospital on the Queen Elizabeth The Queen Mother Hospital site with a contract over the next 15 to 15 years.[3]
The Trust's proposal to centralise surgery on the Canterbury site in order to manage problems caused by "the increasing sub-specialisation of surgery, the lack of availability of surgeons with skills that are essential to managing high risk and emergency general surgery, and the difficulty recruiting both permanent and locum medical staff" in May 2014 aroused opposition among consultants.[4]
In May 2018 the trust announced plans to transfer 850 cleaning, catering, switchboard and portering staff who work for Serco and 250 NHS staff working on estates, procurement and facilities to a new limited company owned by the trust and described as a social enterprise.[5]
Performance
In 2010, it was named "Trust of the Year 2010" by the healthcare information organisation Dr Foster.[7]
The Trust was placed in special measures by Monitor (NHS) in September 2014 following an unfavourable report from the Care Quality Commission.[8]
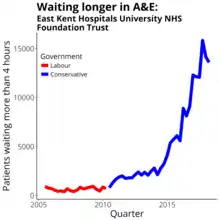
In 2015 the Trauma Audit & Research Network showed that the William Harvey Hospital in Ashford was the best performing hospital receiving trauma patients in England and Wales, out of 100 hospitals offering trauma facilities across the country, according to survival rates of patients.[9] The Care Quality Commission upgraded the Trust from "inadequate" to "requires improvement" and cited significant improvements. Two of the Trust’s five hospitals were rated as "Good". It was one of 26 responsible for half of the national growth in patients waiting more than four hours in accident and emergency over the 2014/5 winter.[10] It hit controversy when an RAF sergeant was asked to leave the waiting room in case his uniform upset other patients. It admitted breaching a patient's human rights when it placed a "do not resuscitate" (DNR) order on the patients notes because the patient had learning difficulties. The trust had not consulted the family about the decision.[11]
In 2016 the Trust saw improvements in its annual Patient-Led Assessment in Care Environments audits, which were introduced nationally in 2013. All hospitals, hospices and day treatment centres that give NHS-funded care are subject to a PLACE inspection. In April 2016 it admitted that it could not cope with the overwhelming demand on its ophthalmology department, which saw nearly 100,000 patients in 2015/6. 7000 were in need of follow-up and at risk of deteriorating eyesight.[12]
In October 2017 after months of very poor performance against the A&E four hour target it was clearly the worst performing trust in England on A&E in 2017-18, with around 30%t of patients waiting over four hours. The Chair of the trust, Nikki Cole, resigned and was replaced by Peter Carter.[13] In 2017-18 East Kent Hospitals saw 74.3% of A&E patients within four hours.[14]
In August 2018 it announced that planned orthopaedic operations would be moved from the William Harvey Hospital to the Kent and Canterbury Hospital in an attempt to avoid cancellations.[15]
In 2018 it had 214 estates and facilities related incidents. It runs more than 100 buildings, some of which date back to the 1930s, and appealed for £34 million in emergency capital funding in January 2019.[16]
The trust commissioned 28 beds from a residential home, Ami Lodge in Deal, Kent, to support patients medically fit to leave hospital but not able to return to their own home. It was forced to abandon the scheme when the Care Quality Commission rated the home "inadequate" in November 2018.[17]
In 2020 the BBC found 7 cases of babies either stillborn or who died shortly after birth since 2016, these cases should have been prevented with better care. The Royal College of Obstetricians and Gynaecologists found in 2015, consultants, failing to do labour ward rounds, failing to review women, make care plans or attend out of hours when asked, consultants, rarely did CTG training, and reportedly were, "doing their own thing rather than follow guidelines" Staff alleged at the review, the board did not consider maternity services a priority and no action would be taken over concerns raised. In 2014 the trust was put into special measures after Care Quality Commission rated its care, including maternity care inadequate. Since then the CQC rated it as requiring improvement.[18]
From 2016 to 2019 the trust had to close one of its two maternity units, which are nearly 40 miles apart, to new births 111 times. At least 120 women in labour were diverted. Although it is not unusual for maternity units close or divert for short periods these closures were unusually frequent.[19] In October 2020 the trust was prosecuted by the Care Quality Commission for failing to provide safe care and treatment exposing Harry Richford and his mother Sarah. Harry died a week after his birth at Queen Elizabeth The Queen Mother Hospital in 2017. This is the first such prosecution of an acute trust.[20]
References
- "Annual Report, Quality Report and Accounts 2018/19". East Kent Hospitals University NHS Foundation Trust. 2 September 2019. p. 15. Retrieved 28 September 2019.
- "Kent trusts issue £40m EPR tender". E Health Insider. 24 December 2013. Retrieved 12 January 2014.
- "East Kent FT seeks partner to 'reinvigorate' private offering". Health Service Journal. 11 April 2014. Retrieved 14 April 2014.
- "Surgery centralisation plans on hold following clinician concerns". Health Service Journal. 3 June 2014. Retrieved 18 June 2014.
- "Over 1,000 staff to transfer to trust subsidiary company". Health Service Journal. 9 May 2018. Retrieved 13 August 2018.
- "A&E Attendances and Emergency Admissions". NHS England. Retrieved 12 April 2018.
- East Kent Hospitals University NHS Foundation Trust named Trust of the Year in the 2010 Hospital Guide
- "East Kent Health Trust placed into special measures by Monitor following damning CQC report on sites in Canterbury, Ashford and Margate". Kent Online. 2 September 2014. Retrieved 28 September 2014.
- "William Harvey Hospital rated best performing hospital in country for trauma". East Kent Hospitals University NHS Foundation Trust. 2015. Retrieved 1 October 2018.
- "26 trusts responsible for half of national A&E target breach". Health Service Journal. 1 April 2015. Retrieved 3 May 2015.
- Dreaper, Jane (8 December 2015). "Apology over 'do not resuscitate' order". BBC News.
- "Hospital 'overwhelmed' by eye care demand". Health Service Journal. 14 April 2016. Retrieved 19 June 2016.
- "EAST KENT HOSPITALS UNIVERSITY NHS FOUNDATION TRUST Worst performing A&E trust appoints new interim chair". Health Service Journal. 3 October 2017. Retrieved 23 December 2017.
- The 10 worst A&Es for waits revealed BBC
- "Elective operations moved to new hospital ahead of winter". Health Service Journal. 21 August 2018. Retrieved 1 October 2018.
- "Trust seeks £34m in emergency capital". Health Service Journal. 28 January 2019. Retrieved 3 March 2019.
- "Trust spot purchasing beds after ending deal with 'inadequate' home". Health Service Journal. 19 February 2019. Retrieved 24 March 2019.
- East Kent hospitals: Baby deaths 'could have been prevented' BBC
- "Exclusive: Trust diverted at least 120 women in labour in four years". Health Service Journal. 30 April 2020. Retrieved 8 June 2020.
- "CQC to prosecute acute trust in groundbreaking case". Health Service Journal. 9 October 2020. Retrieved 25 November 2020.