Extramedullary hematopoiesis
Extramedullary hematopoiesis (EMH or sometimes EH[1]) refers to hematopoiesis occurring outside of the medulla of the bone (bone marrow).[2] It can be physiologic or pathologic.
Physiologic EMH occurs during embryonic and fetal development; during this time the main site of fetal hematopoiesis are liver and the spleen.
Pathologic EMH can occur during adulthood when physiologic hematopoiesis can't work properly in the bone marrow and the hematopoietic stem cells (HSC) have to migrate to other tissues in order to continue with the formation of blood cellular components. Pathologic EMH can be caused by myelofibrosis,[3] thalassemias or disorders caused in the hematopoietic system.
Physiologic EMH
During fetal development, hematopoiesis occurs mainly in the fetal liver followed by localization to the bone marrow.[4] Hematopoiesis also takes place in many other tissues or organs such as the yolk sac, the aorta-gonad mesonephros (AGM) region, the spleen, and lymph nodes. During development, vertebrates go through a primitive and a definitive phase of hematopoiesis. The lungs also play a role in platelet production in adults.[5]
Primitive hematopoiesis
Primitive hematopoiesis occurs in the yolk sac during early embryonic development. It is characterized by the production of erythroid progenitors or nucleated erythrocytes, also known as erythroblasts or megaloblasts. The main objective of the production of these cells will be the facilitation of tissue oxygenation to support rapid embryonic growth. This primitive phase is transitory and the cells that are produced express embryonic globins, aren't pluripotent, and aren't capable of self-renewal.
Definitive hematopoiesis
Definitive hematopoiesis differs from the primitive phase through the production of hematopoietic stem cells. The formation of these cells occurs in the AGM later in development. Later, they migrate to the fetal liver where the majority of physiologic EMH takes place. Finally, once the bone marrow has developed, they migrate there. They can also migrate to the spleen and lymph nodes where hematopoiesis can occur, but to a lesser degree.
Pulmonary hematopoiesis
Pulmonary hematopoiesis also appears to play an important role in adults.[5] In comparison to the bone marrow, where trilineage hematopoiesis occurs, the lungs preferentially contribute to the production of platelets through a resident population of megakaryocytes. This is supported by studies showing that blood leaving the lungs has more platelets and fewer progenitor cells than blood entering the lungs. It has been seen that in cases of severe thrombocytopenia, pulmonary megakaryocytes migrate out of lungs into the bone marrow, where they help to replenish the depleted bone marrow population.
Pathologic EMH
In adults, the majority of hematopoiesis occurs in the bone marrow. Significant production in any other organ is usually the result of a pathological process. When red blood cell (RBC) numbers are low, the body induces a homeostatic mechanism aimed to increase the synthesis of RBCs, typically via the production of erythropoietin. If the loss of RBCs becomes severe, hematopoiesis will occur in the extramedullary spaces outside the bone.[6]
The cause of pathologic EMH can be one of many hematological diseases, such as myelofibrosis, or as a result of bone marrow irradiation. Thalassemia and its resultant hemolytic anemia is another important cause of pathologic EMH. EMH has been observed in numerous other benign hematological disorders such as sickle cell anemia, hereditary spherocytosis, congenital dyserythroblastic anemia and idiopathic thrombocytopenic purpura.[6] EMH can also be seen as part of the response to systemic inflammation or infection.
Sites of EMH
Sites of EMH can be widespread however, most common localizations are in the spleen, liver, and lymph nodes. Other manifestations occur in the thymus, heart, breast, prostate, broad ligaments, kidneys, adrenal glands, pleura, retroperitoneal tissue, skin, peripheral and cranial nerves, and the spinal canal.[6][7]
Spleen
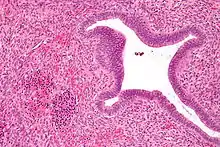
During the postnatal period, the spleen is becomes a frequent site of EMH whereas, during the embryonic stages of hematopoiesis, it is only a minor factor. Despite the hypoxic/acidic conditions of the splenic microenvironment, supplied with a legion of macrophages making it inhospitable for HSCs, EMH usually occurs within the red pulp. Among the various organs associated with EMH, the spleen offers a unique site for evaluation of hematopoietic stem cell (HSC)/niche interactions.[8][7]
Liver
It is normal for infants have hepatic EMH as they are developing up until roughly 5 weeks of age.[9] On the other hand, hepatic EMH in adults can indicate a pathological state. This includes transplantation, hepatic tumors, hepatic disorders, or sepsis. Hepatoblastoma, adenomas and hepatocellular carcinomas can also lead to EMH in adults.[10][11] Additionally, EMH is often observed within the hepatic sinusoids.
Lymph nodes
EMH in the lymph nodes is usually associated with underlying hematopoietic neoplasms. Myeloproliferative neoplasms (MPNs) tend to result in EMH.[12] If EMH is identified in the lymph nodes of an adult or infant, a hematologic evaluation, including blood cell counts, peripheral blood smear and potentially a bone marrow biopsy should be performed.[7]
Other sites
The following tissues may also be associated with EMH: thymus, heart, breast, prostate, fatty tissue, adrenal glands, kidney, periosteum, pleural cavity, para-vertebral regions, intra-spinal tissue, retroperitoneal tissue, skin, peripheral and cranial nerves, the spinal canal, pre-sacral region, nasopharyngeal region, para-nasal sinuses and numerous types of benign/malignant neoplasms. The most common sites of EMH associated with neoplastic disorder are the spleen, lymph nodes, skin, bone, small intestine, orbit, breast, cervix, nasal sinus, mediastinum and brain.[7][13][14][15]
Microenvironment of EMH
Of the various organs associated with EMH, the spleen offers a unique site for evaluating HSC/niche interactions as it is one of the most common sites of EMH, however it does not play a major role in embryonic/developmental hematopoiesis.[7] High expression levels of CXCL12 were found in the human spleens of EMH-positive patients compared to those who were EMH-negative. The high expression of CXCL12, a candidate marker of bone marrow niche-constituting in cells, indicates HSC/niche interactions in the spleen.[16] Studies have show that CXCL12 localizes in the sinus endothelial cells of the red pulp in EMH-positive spleens; whereas, CXCL12 was expressed throughout the vascular endothelial cells of the white pulp in spleens of EMH-negative and -positive cases.[16] The fact that EMH frequently occurs in the red pulp, is supported by current data that suggests that splenic sinus endothelial cells expressing CXCL12 may contribute to the attachment and recruitment of circulating hematopoietic precursor cells, forming bone marrow niche-like regions of EMH in the human spleen.[16]
References
- Kim CH (2010-03-23). "Homeostatic and pathogenic extramedullary hematopoiesis". Journal of Blood Medicine. 1: 13–9. doi:10.2147/jbm.s7224. PMC 3262334. PMID 22282679.
- Birbrair A, Frenette PS (April 2016). "Niche heterogeneity in the bone marrow". Annals of the New York Academy of Sciences. 1370 (1): 82–96. Bibcode:2016NYASA1370...82B. doi:10.1111/nyas.13016. PMC 4938003. PMID 27015419.
- Chunduri S, Gaitonde S, Ciurea SO, Hoffman R, Rondelli D (October 2008). "Pulmonary extramedullary hematopoiesis in patients with myelofibrosis undergoing allogeneic stem cell transplantation". Haematologica. 93 (10): 1593–5. doi:10.3324/haematol.13203. PMID 18641018.
- Jagannathan-Bogdan M, Zon LI (June 2013). "Hematopoiesis". Development. 140 (12): 2463–7. doi:10.1242/dev.083147. PMC 3666375. PMID 23715539.
- Lefrançais E, Ortiz-Muñoz G, Caudrillier A, Mallavia B, Liu F, Sayah DM, et al. (April 2017). "The lung is a site of platelet biogenesis and a reservoir for haematopoietic progenitors". Nature. 544 (7648): 105–109. Bibcode:2017Natur.544..105L. doi:10.1038/nature21706. PMC 5663284. PMID 28329764.
- Sohawon D, Lau KK, Lau T, Bowden DK (October 2012). "Extra-medullary haematopoiesis: a pictorial review of its typical and atypical locations". Journal of Medical Imaging and Radiation Oncology. 56 (5): 538–44. doi:10.1111/j.1754-9485.2012.02397.x. PMID 23043573.
- Yamamoto K, Miwa Y, Abe-Suzuki S, Abe S, Kirimura S, Onishi I, et al. (January 2016). "Extramedullary hematopoiesis: Elucidating the function of the hematopoietic stem cell niche (Review)". Molecular Medicine Reports. 13 (1): 587–91. doi:10.3892/mmr.2015.4621. PMID 26648325.
- Wolf BC, Neiman RS (1987). "Hypothesis: splenic filtration and the pathogenesis of extramedullary hematopoiesis in agnogenic myeloid metaplasia". Hematologic Pathology. 1 (1): 77–80. PMID 3332874.
- MacSween RM, Burt AD, Portmann BC, Ishak KG, Scheurer PJ, Anthony PP, Weisenberg E (2003). "Pathology of the liver, 4th edition". Diagnostic Cytopathology. 29 (1): 43. doi:10.1002/dc.10338. ISSN 1097-0339.
- Tsamandas AC, Jain AB, Raikow RB, Demetris AJ, Nalesnik MA, Randhawa PS (August 1995). "Extramedullary hematopoiesis in the allograft liver". Modern Pathology. 8 (6): 671–4. PMID 8532704.
- Schlitt HJ, Schäfers S, Deiwick A, Eckardt KU, Pietsch T, Ebell W, et al. (March 1995). "Extramedullary erythropoiesis in human liver grafts". Hepatology. 21 (3): 689–96. doi:10.1002/hep.1840210314. PMID 7533123.
- Craig CE, Quaglia A, Dhillon AP (November 2004). "Extramedullary haematopoiesis in massive hepatic necrosis". Histopathology. 45 (5): 518–25. doi:10.1111/j.1365-2559.2004.01970.x. PMID 15500656.
- Johns JL, Christopher MM (May 2012). "Extramedullary hematopoiesis: a new look at the underlying stem cell niche, theories of development, and occurrence in animals". Veterinary Pathology. 49 (3): 508–23. doi:10.1177/0300985811432344. PMID 22262354.
- Sohawon D, Lau KK, Lau T, Bowden DK (October 2012). "Extra-medullary haematopoiesis: a pictorial review of its typical and atypical locations". Journal of Medical Imaging and Radiation Oncology. 56 (5): 538–44. doi:10.1111/j.1754-9485.2012.02397.x. PMID 23043573.
- Palatnik A, Narayan R, Walters M (November 2012). "Extramedullary hematopoiesis involving uterus, fallopian tubes, and ovaries, mimicking bilateral tuboovarian abscesses". International Journal of Gynecological Pathology. 31 (6): 584–7. doi:10.1097/PGP.0b013e31825183ad. PMID 23018220.
- Miwa Y, Hayashi T, Suzuki S, Abe S, Onishi I, Kirimura S, et al. (June 2013). "Up-regulated expression of CXCL12 in human spleens with extramedullary haematopoiesis". Pathology. 45 (4): 408–16. doi:10.1097/pat.0b013e3283613dbf. PMID 23619587.