Oncolytic herpes virus
Many variants of herpes simplex virus have been considered for viral therapy of cancer; the early development of these was thoroughly reviewed in the journal Cancer Gene Therapy in 2002.[1] This page describes (in the order of development) the most notable variants—those tested in clinical trials: G207, HSV1716, NV1020 and Talimogene laherparepvec (previously Oncovex-GMCSF). These attenuated versions are constructed by deleting viral genes required for infecting or replicating inside normal cells but not cancer cells, such as ICP34.5, ICP6/UL39, and ICP47.
| Oncolytic herpes virus | |
|---|---|
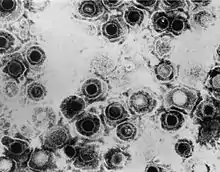 | |
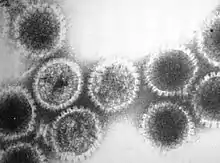
| TEM micrograph of a herpes simplex virus. | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Duplodnaviria |
| Kingdom: | Heunggongvirae |
| Phylum: | Peploviricota |
| Class: | Herviviricetes |
| Order: | Herpesvirales |
| Family: | Herpesviridae |
| Genus: | Simplexvirus |
| Species: | Human alphaherpesvirus 1 |
HSV1716
HSV1716 is a first generation oncolytic virus developed by The Institute of Virology, Glasgow, UK, and subsequently by Virttu Biologics (formerly Crusade Laboratories, a spin-out from The Institute of Virology), to selectively destroy cancer cells. The virus has the trade name SEPREHVIR. It is based on the herpes simplex virus (HSV-1). The HSV1716 strain has a deletion of the gene ICP34.5. ICP34.5 is a neurovirulence gene (enabling the virus to replicate in neurons of the brain and spinal cord). Deletion of this gene provides the property of tumor-selective replication to the virus (i.e. largely prevents replication in normal cells, while still allowing replication in tumor cells), although it also reduces replication in tumor cells as compared to wild type HSV.[2][3]
A vital part of the normal mechanism of HSV-1, the ICP34.5 protein has been proposed to condition post-mitotic cells for viral replication. With no ICP34.5 gene, the HSV-1716 variant is unable to overcome normal defences of healthy differentiated cells (mediated by PKR) to replicate efficiently. However, tumour cells have much weaker PKR-linked defences, which may be the reason why HSV1716 effectively kills a wide range of tumour cell lines in tissue culture.
An HSV1716 variant, HSV1716NTR is an oncolytic virus generated by inserting the enzyme NTR into the virus HSV1716 as a GDEPT strategy.[4] In-vivo, administration of the prodrug CB1954 to athymic mice bearing either A431 or A2780 tumour xenografts, 48 hours after intra-tumoral injection of HSV1790, resulted in a marked reduction in tumour volumes and significantly improved survival compared to administration of virus alone. A similar approach has been taken with a variant of HSV1716 that expresses the noradrenaline transporter to deliver radioactive iodine into individual infected cancer cells, by tagging a protein that cancer cells transport. The nor-adrenaline transporter specifically transports a compound containing radioactive iodine across the cell membrane, using genes from the virus. The only cells in the body that receive a significant radiation dose are those infected and their immediate neighbours.[5]
Clinical trials
- High grade glioma: Three phase I trials have been completed and two phase II trials are in preparation.[6][7]
- Squamous cell carcinoma of head and neck: A phase I trial has been completed.[8]
- Malignant melanoma: A phase I trial has been completed.[9]
- Hepatocellular carcinoma: A phase I/II trial is in preparation.
- Malignant pleural mesothelioma: A phase I/II trial is in progress.[10]
- Non-CNS pediatric cancer: A phase I trial is in progress.[11]
G207
G207 was constructed as a second-generation vector from HSV-1 laboratory strain F, with ICP34.5 deleted and the ICP6 gene inactivated by insertion of the E. coli LacZ gene.[12]
Two phase I clinical trials in glioma were completed.[13][14][15] The results of the first trial were published simultaneously with the first trial of HSV1716 in 2000, with commentators praising the demonstration of safety of these viruses when injected into brain tumours but also expressing disappointment that viral replication could not be demonstrated due to the difficulty of taking biopsies from brain tumours.[16]
NV1020
NV1020 is an oncolytic herpes virus initially developed by Medigene Inc. and licensed for development by Catherex Inc. in 2010.[17] NV1020 has a deletion of just one copy of the ICP34.5 gene and ICP6 is intact.[18] A direct comparison of NV1020 and G207 in a mouse model of peritoneal cancer showed that NV1020 is more effective at lower doses.[19]
Clinical trials
A Phase I/II study completed in 2008 evaluating NV1020 for treatment of metastatic colorectal cancer in the liver.[20] The study assessed tumour response by CT scan and FDG-PET scans, showing 67% of patients had an initial increase in tumour size then followed by a decrease in 64% of patients.[21][19]
Talimogene laherparepvec
Talimogene laherparepvec is the USAN name for the oncolytic virus also known as 'OncoVEX GM-CSF'. It was developed by BioVex Inc. (Woburn, MA, USA & Oxford, UK) until BioVex was purchased by Amgen in January 2011.[22]
It is a second-generation herpes simplex virus based on the JS1 strain and expressing the immune stimulatory factor GM-CSF.[23][24] Like other oncolytic versions of HSV it has a deletion of the gene encoding ICP34.5, which provides tumor selectivity.[25] It also has a deletion of the gene encoding ICP47, a protein that inhibits antigen presentation,[26] and an insertion of a gene encoding GM-CSF, an immune stimulatory cytokine.[2][3] Deletion of the gene encoding ICP47 also puts the US11 gene (a late gene) under control of the immediate early ICP47 promoter. The earlier and greater expression of US11 (also involved in overcoming PKR-mediated responses) largely overcomes the reduction in replication in tumor cells of ICP34.5-deleted HSV as compared to wild type virus, but without reducing tumor selectivity.
- Clinical trials
Including phase III : See Talimogene laherparepvec
References
- Varghese S, Rabkin SD (December 2002). "Oncolytic herpes simplex virus vectors for cancer virotherapy". Cancer Gene Therapy. 9 (12): 967–78. doi:10.1038/sj.cgt.7700537. PMID 12522436.
- Mohr I, Gluzman Y (September 1996). "A herpesvirus genetic element which affects translation in the absence of the viral GADD34 function". The EMBO Journal. 15 (17): 4759–66. doi:10.1002/j.1460-2075.1996.tb00853.x. PMC 452208. PMID 8887567.
- Liu BL, Robinson M, Han ZQ, Branston RH, English C, Reay P, et al. (February 2003). "ICP34.5 deleted herpes simplex virus with enhanced oncolytic, immune stimulating, and anti-tumour properties". Gene Therapy. 10 (4): 292–303. doi:10.1038/sj.gt.3301885. PMID 12595888.
- Braidwood L, Dunn PD, Hardy S, Evans TR, Brown SM (June 2009). "Antitumor activity of a selectively replication competent herpes simplex virus (HSV) with enzyme prodrug therapy". Anticancer Research. 29 (6): 2159–66. PMID 19528476.
- Sorensen A, Mairs RJ, Braidwood L, Joyce C, Conner J, Pimlott S, et al. (April 2012). "In vivo evaluation of a cancer therapy strategy combining HSV1716-mediated oncolysis with gene transfer and targeted radiotherapy". Journal of Nuclear Medicine. 53 (4): 647–54. doi:10.2967/jnumed.111.090886. PMID 22414636.
- Harrow S, Papanastassiou V, Harland J, Mabbs R, Petty R, Fraser M, et al. (November 2004). "HSV1716 injection into the brain adjacent to tumour following surgical resection of high-grade glioma: safety data and long-term survival". Gene Therapy. 11 (22): 1648–58. doi:10.1038/sj.gt.3302289. PMID 15334111.
- Papanastassiou V, Rampling R, Fraser M, Petty R, Hadley D, Nicoll J, et al. (March 2002). "The potential for efficacy of the modified (ICP 34.5(-)) herpes simplex virus HSV1716 following intratumoural injection into human malignant glioma: a proof of principle study". Gene Therapy. 9 (6): 398–406. doi:10.1038/sj.gt.3301664. PMID 11960316.
- Mace AT, Ganly I, Soutar DS, Brown SM (August 2008). "Potential for efficacy of the oncolytic Herpes simplex virus 1716 in patients with oral squamous cell carcinoma". Head & Neck. 30 (8): 1045–51. doi:10.1002/hed.20840. PMID 18615711.
- MacKie RM, Stewart B, Brown SM (February 2001). "Intralesional injection of herpes simplex virus 1716 in metastatic melanoma". Lancet. 357 (9255): 525–6. doi:10.1016/S0140-6736(00)04048-4. PMID 11229673. S2CID 34442464.
- Clinical trial number NCT01721018 for "Intrapleural Administration of HSV1716 to Treat Patients With Malignant Pleural Mesothelioma" at ClinicalTrials.gov
- Clinical trial number NCT00931931 for "HSV1716 in Patients With Non-Central Nervous System (Non-CNS) Solid Tumors" at ClinicalTrials.gov
- Mineta T, Rabkin SD, Yazaki T, Hunter WD, Martuza RL (September 1995). "Attenuated multi-mutated herpes simplex virus-1 for the treatment of malignant gliomas". Nature Medicine. 1 (9): 938–43. doi:10.1038/nm0995-938. PMID 7585221. S2CID 8712053.
- Markert JM, Medlock MD, Rabkin SD, Gillespie GY, Todo T, Hunter WD, et al. (May 2000). "Conditionally replicating herpes simplex virus mutant, G207 for the treatment of malignant glioma: results of a phase I trial". Gene Therapy. 7 (10): 867–74. doi:10.1038/sj.gt.3301205. PMID 10845725.
- Clinical trial number NCT00028158 for "Safety and Effectiveness Study of G207, a Tumor-Killing Virus, in Patients With Recurrent Brain Cancer" at ClinicalTrials.gov
- Clinical trial number NCT00157703 for "G207 Followed by Radiation Therapy in Malignant Glioma" at ClinicalTrials.gov
- Kirn DH (May 2000). "A tale of two trials: selectively replicating herpesviruses for brain tumors". Gene Therapy. 7 (10): 815–6. doi:10.1038/sj.gt.3301213. PMID 10845717.
- "MediGene AG divests Oncolytic Herpes Simplex Viruses (oHSV) program to Catherex, Inc" (Press release). MediGene AG. April 13, 2010. Archived from the original on October 29, 2013. Retrieved May 7, 2013.
- Varghese S, Rabkin SD (December 2002). "Oncolytic herpes simplex virus vectors for cancer virotherapy". Cancer Gene Therapy. 9 (12): 967–78. doi:10.1038/sj.cgt.7700537. PMID 12522436.
- Geevarghese SK, Geller DA, de Haan HA, Hörer M, Knoll AE, Mescheder A, et al. (September 2010). "Phase I/II study of oncolytic herpes simplex virus NV1020 in patients with extensively pretreated refractory colorectal cancer metastatic to the liver". Human Gene Therapy. 21 (9): 1119–28. doi:10.1089/hum.2010.020. PMC 3733135. PMID 20486770.
- Clinical trial number NCT00149396 for "Safety and Efficacy of a Genetically Engineered Herpes Simplex Virus NV1020 to Treat Colorectal Cancer Metastatic to Liver" at ClinicalTrials.gov
- Sze DY, Iagaru AH, Gambhir SS, De Haan HA, Reid TR (January 2012). "Response to intra-arterial oncolytic virotherapy with the herpes virus NV1020 evaluated by [18F]fluorodeoxyglucose positron emission tomography and computed tomography". Human Gene Therapy. 23 (1): 91–7. doi:10.1089/hum.2011.141. PMID 21895536.
- "Amgen, Form 8-K, Current Report, Filing Date Jan 26, 2012" (PDF). secdatabase.com. Retrieved Jan 8, 2013.
- "OncoVEXGM-CSF RAC Submission" (PDF). NIH Genetic Modification Clinical Research Information System (GeMCRIS®). Archived from the original (PDF) on 28 May 2010. Retrieved 1 April 2013.
- Hu JC, Coffin RS, Davis CJ, Graham NJ, Groves N, Guest PJ, et al. (November 2006). "A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor". Clinical Cancer Research. 12 (22): 6737–47. doi:10.1158/1078-0432.CCR-06-0759. PMID 17121894.
- Raafat N, Sadowski-Cron C, Mengus C, Heberer M, Spagnoli GC, Zajac P (September 2012). "Preventing vaccinia virus class-I epitopes presentation by HSV-ICP47 enhances the immunogenicity of a TAP-independent cancer vaccine epitope". International Journal of Cancer. 131 (5): E659-69. doi:10.1002/ijc.27362. PMID 22116674.
- Broughton SE, Dhagat U, Hercus TR, Nero TL, Grimbaldeston MA, Bonder CS, et al. (November 2012). "The GM-CSF/IL-3/IL-5 cytokine receptor family: from ligand recognition to initiation of signaling". Immunological Reviews. 250 (1): 277–302. doi:10.1111/j.1600-065X.2012.01164.x. PMID 23046136.