Platelet-rich plasma
Platelet-rich plasma (PRP), also known as autologous conditioned plasma, is a concentrate of platelet-rich plasma protein derived from whole blood, centrifuged to remove red blood cells. Though promoted to treat an array of medical problems, evidence for benefit is mixed as of 2020, with some evidence for use in certain conditions and against use in other conditions.[1][2][3] The cost per injection is generally US$500 to $2,000 as of 2019.[4]
| Platelet-rich plasma | |
|---|---|
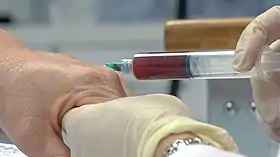 Platelet-rich plasma injection into the hand | |
| MeSH | D053657 |
Medical use
Evidence for benefit of PRP is mixed, with some evidence for use in certain conditions and against use in other conditions.[5][6][3] It has been investigated for chronic tendinitis,[7] osteoarthritis,[8] in oral surgery,[9] and in plastic surgery.[10]
A 2019 review found it not to be useful in rotator cuff disease.[3] While an older review found that it may be useful.[11] Tentative evidence supports its use in osteoarthritis (OA) of the knee.[12][13] A 2019 meta-analysis found that PRP might be more effective in reducing pain and improving function than hyaluronic acid in knee OA.[14]
A 2009 review found few randomized controlled trials that adequately evaluated the safety and efficacy of PRP treatments and concluded that PRP was "a promising, but not proven, treatment option for joint, tendon, ligament, and muscle injuries".[15] As compared to other conservative treatments for non-surgical orthopedic illnesses (e.g. steroid injection for plantar fasciitis), evidence does no support the use of PRP as a conservative treatment.[16] A 2018 review found that evidence was lacking for Achilles tendinopathy.[17] A 2019 meta-analysis found that, for most outcomes in Achilles tendinopathy, PRP treatment did not differ from placebo treatment.[18]
A 2010 Cochrane review of use in sinus lifts during dental implant placement found no evidence of benefit.[9] A 2013 review stated more evidence was needed to determine effectiveness for hair regrowth.[19]
A 2014 Cochrane review of PRP in musculoskeletal injuries found very weak evidence for a decrease in pain in the short term, and no difference in function in the short, medium or long term. There was weak evidence that suggested that harm occurred at comparable, low rates in treated and untreated people.[20] Similarly, another 2017 review for treating pain on skin graft donor sites found the evidence for benefit was poor.[21]
It has not been shown to be useful for bone healing.[22] A 2016 review of PRP use to augment bone graft found only one study reporting a difference in bone augmentation, while four studies found no difference.[23]
Besides the use in clinical practice PRP has been utilized for various tissue engineering applications in the context of bone, cartilage, skin, and soft tissue repair. It has been reviewed to serve as a source for the "delivery of growth factors and/or cells within tissue-engineered constructs, often in combination with biomaterials". [24]
Adverse effects
Adverse effects have been poorly studied. The single systematic review of the literature did not report of the types and number of adverse events.[25] In 2019, Health Canada stated that most autologous cell therapies have little evidence showing they work and can pose risks, such as cross-contamination between people if equipment is not sterilized properly or potentially dangerous immune reactions.[26] Health Canada stopped Canadian clinics from offering these types of services with a donor-patient model.[27] Health Canada later clarified that PRP treatments harvested from, and given back to, the same person (in a single procedure) was not covered by its initial guidance as the procedure falls under health care provider regulatory bodies (rather than Health Canada).[28]
Composition

There are four general categories of preparation of PRP based on its leukocyte and fibrin content: leukocyte-rich PRP (L-PRP), leukocyte reduced PRP (P-PRP; leukocyte reduced or pure PRP), leukocyte platelet-rich fibrin and pure platelet-rich fibrin.[29][30]
The efficacy of certain growth factors in healing various injuries and the concentrations of these growth factors found within PRP are the theoretical basis for the use of PRP in tissue repair.[31] The platelets collected in PRP are activated by the addition of thrombin and calcium chloride, which induces the release of the mentioned factors from alpha granules. The growth factors and other cytokines present in PRP include:[31][32]
Manufacturing
PRP is prepared by taking blood from the person, and then putting it through two stages of centrifugation designed to separate PRP from platelet-poor plasma and red blood cells. This is usually done by the clinic offering the treatment, using commercially available kits and equipment.[33] The resulting substance varies from person to person and from facility to facility, making it difficult to understand how safe and effective any specific use is.[33][34]
 Blood drawn from patient
Blood drawn from patient Removal of PRP after double centrifugation
Removal of PRP after double centrifugation PRP is Injected into area of injury via ultrasound guidance
PRP is Injected into area of injury via ultrasound guidance
Society and culture
The cost of a PRP treatment in the U.S. has been quoted as $1000 out-of-pocket expenses, as it is usually not covered by health insurance.[35] PRP has received attention in the popular media as a result of its use by athletes.[36][37][38][35] Use in an office setting is not approved by the FDA.[39]
In the 2010s, contentious cosmetic procedures marketed under the name of "vampire facials" grew in popularity, fueled by celebrity endorsement. These "vampire facials" generally center on PRP treatment, and usually (but not always) involve microneedling.[40][41]
PRP has also been injected into the vagina, in a procedure called "O-shot" or "orgasm shot" with claims that this will improve orgasms.[42] There is no evidence, however, to support these claims.[42][43]
Doping
Some concern exists as to whether PRP treatments violate anti-doping rules.[31] As of 2010 it was not clear if local injections of PRP could have a systemic impact on circulating cytokine levels, affecting doping tests and whether PRP treatments have systemic anabolic effects or affect performance.[31] In January 2011, the World Anti-Doping Agency removed intramuscular injections of PRP from its prohibitions after determining that there is a "lack of any current evidence concerning the use of these methods for purposes of performance enhancement".[44]
See also
References
- Xu, Q; Chen, J; Cheng, L (July 2019). "Comparison of platelet rich plasma and corticosteroids in the management of lateral epicondylitis: A meta-analysis of randomized controlled trials". International Journal of Surgery (London, England). 67: 37–46. doi:10.1016/j.ijsu.2019.05.003. PMID 31128316.
- Belk, JW; Kraeutler, MJ; Houck, DA; Goodrich, JA; Dragoo, JL; McCarty, EC (17 April 2020). "Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-analysis of Randomized Controlled Trials". The American Journal of Sports Medicine: 363546520909397. doi:10.1177/0363546520909397. PMID 32302218.
- Hurley, ET; Hannon, CP; Pauzenberger, L; Fat, DL; Moran, CJ; Mullett, H (May 2019). "Nonoperative Treatment of Rotator Cuff Disease With Platelet-Rich Plasma: A Systematic Review of Randomized Controlled Trials". Arthroscopy: The Journal of Arthroscopic & Related Surgery. 35 (5): 1584–1591. doi:10.1016/j.arthro.2018.10.115. PMID 31000394.
- "Platelet-Rich Plasma is Profitable, But How Well Does It Work?". American Council on Science and Health. 12 February 2019. Retrieved 30 September 2019.
- Mohammed, W; Farah, S; Nassiri, M; McKenna, J (2020). "Therapeutic efficacy of platelet-rich plasma injection compared to corticosteroid injection in plantar fasciitis: A systematic review and meta-analysis". Journal of Orthopaedics. 22: 124–134. doi:10.1016/j.jor.2020.03.053. PMC 7177161. PMID 32336895.
- Lin, MT; Wei, KC; Wu, CH (28 March 2020). "Effectiveness of Platelet-Rich Plasma Injection in Rotator Cuff Tendinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Diagnostics. 10 (4): 189. doi:10.3390/diagnostics10040189. PMC 7235747. PMID 32231127.
- Mishra A, Woodall J, Vieira A (January 2009). "Treatment of tendon and muscle using platelet-rich plasma". Clinics in Sports Medicine. 28 (1): 113–25. doi:10.1016/j.csm.2008.08.007. PMID 19064169.
- Andia I, Sánchez M, Maffulli N (January 2012). "Joint pathology and platelet-rich plasma therapies". Expert Opinion on Biological Therapy. 12 (1): 7–22. doi:10.1517/14712598.2012.632765. PMID 22171664. S2CID 39322743.
- Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, Worthington H, Coulthard P (Spring 2010). "Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review". European Journal of Oral Implantology. 3 (1): 7–26. PMID 20467595.
- Por YC, Shi L, Samuel M, Song C, Yeow VK (May 2009). "Use of tissue sealants in face-lifts: a metaanalysis". Aesthetic Plastic Surgery. 33 (3): 336–9. doi:10.1007/s00266-008-9280-1. PMID 19089492. S2CID 26761928.
- Chen, Xiao; Jones, Ian A.; Park, Caron; Vangsness, C. Thomas (July 2018). "The Efficacy of Platelet-Rich Plasma on Tendon and Ligament Healing: A Systematic Review and Meta-analysis With Bias Assessment". The American Journal of Sports Medicine. 46 (8): 2020–2032. doi:10.1177/0363546517743746. ISSN 1552-3365. PMC 6339617. PMID 29268037.
- Dai WL, Zhou AG, Zhang H, Zhang J (March 2017). "Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Trials". Arthroscopy. 33 (3): 659–670.e1. doi:10.1016/j.arthro.2016.09.024. PMID 28012636.
- Shen L, Yuan T, Chen S, Xie X, Zhang C (January 2017). "The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials". Journal of Orthopaedic Surgery and Research. 12 (1): 16. doi:10.1186/s13018-017-0521-3. PMC 5260061. PMID 28115016.
- Han, Yanhong; Huang, Hetao; Pan, Jianke; Lin, Jiongtong; Zeng, Lingfeng; Liang, Guihong; Yang, Weiyi; Liu, Jun (July 1, 2019). "Meta-analysis Comparing Platelet-Rich Plasma vs Hyaluronic Acid Injection in Patients with Knee Osteoarthritis". Pain Medicine (Malden, Mass.). 20 (7): 1418–1429. doi:10.1093/pm/pnz011. ISSN 1526-4637. PMC 6611633. PMID 30849177.
- Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA (November 2009). "Platelet-rich plasma: from basic science to clinical applications". The American Journal of Sports Medicine. 37 (11): 2259–72. doi:10.1177/0363546509349921. PMID 19875361. S2CID 5914979.
- Franchini M, Cruciani M, Mengoli C, Marano G, Pupella S, Veropalumbo E, Masiello F, Pati I, Vaglio S, Liumbruno GM (November 2018). "Efficacy of platelet-rich plasma as conservative treatment in orthopaedics: a systematic review and meta-analysis". Blood Transfusion = Trasfusione del Sangue. 16 (6): 502–513. doi:10.2450/2018.0111-18. PMC 6214820. PMID 30201082.
- Zhang, YJ; Xu, SZ; Gu, PC; Du, JY; Cai, YZ; Zhang, C; Lin, XJ (August 2018). "Is Platelet-rich Plasma Injection Effective for Chronic Achilles Tendinopathy? A Meta-analysis". Clinical Orthopaedics and Related Research. 476 (8): 1633–1641. doi:10.1007/s11999.0000000000000258. PMC 6259774. PMID 29601383.
- Liu, Chun-jie; Yu, Kun-lun; Bai, Jiang-bo; Tian, De-hu; Liu, Guo-li (April 2019). "Platelet-rich plasma injection for the treatment of chronic Achilles tendinopathy: A meta-analysis". Medicine. 98 (16): e15278. doi:10.1097/MD.0000000000015278. ISSN 0025-7974. PMC 6494278. PMID 31008973.
- Valente Duarte de Sousa IC, Tosti A (May 2013). "New investigational drugs for androgenetic alopecia". Expert Opinion on Investigational Drugs. 22 (5): 573–89. doi:10.1517/13543784.2013.784743. PMID 23550739. S2CID 21653303.
- Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC (April 2014). "Platelet-rich therapies for musculoskeletal soft tissue injuries". The Cochrane Database of Systematic Reviews. 29 (4): CD010071. doi:10.1002/14651858.CD010071.pub3. PMC 6464921. PMID 24782334.
- Sinha S, Schreiner AJ, Biernaskie J, Nickerson D, Gabriel VA (November 2017). "Treating pain on skin graft donor sites: Review and clinical recommendations". The Journal of Trauma and Acute Care Surgery. 83 (5): 954–964. doi:10.1097/TA.0000000000001615. PMID 28598907. S2CID 44520644.
- Griffin XL, Smith CM, Costa ML (February 2009). "The clinical use of platelet-rich plasma in the promotion of bone healing: a systematic review". Injury. 40 (2): 158–62. doi:10.1016/j.injury.2008.06.025. PMID 19084836.
- Pocaterra A, Caruso S, Bernardi S, Scagnoli L, Continenza MA, Gatto R (August 2016). "Effectiveness of platelet-rich plasma as an adjunctive material to bone graft: a systematic review and meta-analysis of randomized controlled clinical trials". International Journal of Oral and Maxillofacial Surgery. 45 (8): 1027–34. doi:10.1016/j.ijom.2016.02.012. PMID 26987695.
- Lang, Siegmund; Loibl, Markus; Herrmann, Marietta (2018). "Platelet-Rich Plasma in Tissue Engineering: Hype and Hope". European Surgical Research. Europaische Chirurgische Forschung. Recherches Chirurgicales Europeennes. 59 (3–4): 265–275. doi:10.1159/000492415. ISSN 1421-9921. PMID 30244245.
- Frautschi RS, Hashem AM, Halasa B, Cakmakoglu C, Zins JE (March 2017). "Current Evidence for Clinical Efficacy of Platelet Rich Plasma in Aesthetic Surgery: A Systematic Review". Aesthetic Surgery Journal. 37 (3): 353–362. doi:10.1093/asj/sjw178. PMID 28207031.
- Canada, Health (2019-05-15). "Health Canada Policy Position Paper – Autologous Cell Therapy Products". aem. Retrieved 2019-07-09.
- "Health Canada orders halt to unproven stem cell-based injection treatments". Retrieved 2019-07-09.
- "Health Canada clarifies position on Platelet Rich Plasma treatments". Health Canada. Health Canada. 26 July 2019. Retrieved 7 January 2020.
- Pavlovic V, Ciric M, Jovanovic V, Stojanovic P (2016). "Platelet Rich Plasma: a short overview of certain bioactive components". Open Medicine. 11 (1): 242–247. doi:10.1515/med-2016-0048. PMC 5329835. PMID 28352802.
- Bielecki T, Dohan Ehrenfest DM, Everts PA, Wiczkowski A (June 2012). "The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: new perspectives". Current Pharmaceutical Biotechnology. 13 (7): 1153–62. doi:10.2174/138920112800624373. PMID 21740376.
- Borrione P, Gianfrancesco AD, Pereira MT, Pigozzi F (October 2010). "Platelet-rich plasma in muscle healing". American Journal of Physical Medicine & Rehabilitation. 89 (10): 854–61. doi:10.1097/PHM.0b013e3181f1c1c7. PMID 20855985.
- Yu W, Wang J, Yin J (April 2011). "Platelet-rich plasma: a promising product for treatment of peripheral nerve regeneration after nerve injury". The International Journal of Neuroscience. 121 (4): 176–80. doi:10.3109/00207454.2010.544432. PMID 21244302. S2CID 26837842.
- Dhurat R, Sukesh M (2014). "Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author's Perspective". Journal of Cutaneous and Aesthetic Surgery. 7 (4): 189–97. doi:10.4103/0974-2077.150734. PMC 4338460. PMID 25722595.
- Kanchanatawan W, Arirachakaran A, Chaijenkij K, Prasathaporn N, Boonard M, Piyapittayanun P, Kongtharvonskul J (May 2016). "Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee". Knee Surgery, Sports Traumatology, Arthroscopy. 24 (5): 1665–77. doi:10.1007/s00167-015-3784-4. PMID 26387122. S2CID 35221300.
- Kolata G (2010-01-12). "Popular Blood Therapy May Not Work". New York Times.
- Schwarz A (2009-02-16). "A Promising Treatment for Athletes, in Blood". New York Times. New York.
- Reynolds G (2011-01-26). "Phys Ed: Does Platelet-Rich Plasma Therapy Really Work?". New York Times.
- Storrs C (2009-12-18). "Is Platelet-Rich Plasma an Effective Healing Therapy?". Scientific American.
- Beitzel K, Allen D, Apostolakos J, Russell RP, McCarthy MB, Gallo GJ, Cote MP, Mazzocca AD (February 2015). "US definitions, current use, and FDA stance on use of platelet-rich plasma in sports medicine". The Journal of Knee Surgery. 28 (1): 29–34. doi:10.1055/s-0034-1390030. PMID 25268794.
- Georgiou, Aristos (14 September 2018). "What is a vampire facial?". Newsweek. Retrieved 29 March 2019.
- "What it's really like to get the infamous vampire facial". The Independent. 28 February 2018. Retrieved 29 March 2019.
- Osborne, Hannah (8 July 2016). "Injecting blood plasma into your clitoris for $2,500 won't give you with better orgasms". International Business Times UK. Retrieved 1 October 2018.
- Goodman, Michael P. (2016). Female Genital Plastic and Cosmetic Surgery. John Wiley & Sons. p. PT391. ISBN 9781118848487.
There is presently no information in peer reviewed literature.
- "World Anti-Doping Agency announces changes to Prohibited List". Irish Medical Times. 2011-01-10.