Supplier-induced demand
In economics, supplier induced demand (SID) may occur when asymmetry of information exists between supplier and consumer. The supplier can use superior information to encourage an individual to demand a greater quantity of the good or service they supply than the Pareto efficient level, should asymmetric information not exist. The result of this is a welfare loss.
Health economics
The doctor-patient relationship is key to the practice of healthcare and is central to the delivery of high quality efficient care while maintaining costs. Controversy surrounds the extent and existence of supplier induced demand (SID). Some believe it is ideological rather than evidence-based. Validity of results from different models is reported to lack consensus, making policy difficult to develop and implement.[1] Normative definitions cast negative aspersions on physicians indicating they act as imperfect agents for their own self-interests. A positive perspective of SID focuses on a physician's ability to shift a patient's demand curve to the right.[2] Demand inducement refers to a "physician's alleged ability to shift patients' demand for medical care at a given price, that is, to convince patients to increase their use of medical care without lowering the price charged."[3] Economists have explored how this additional care will affect patient welfare.[4]
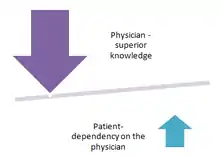
In health economics, supplier induced demand (SID) can be defined as the amount of demand that exists beyond what would have occurred in a market in which patients are fully informed.[5] In healthcare, a physician acts as an agent on behalf of the patient (the principal) guiding them to make the best possible treatment decisions. This agency relationship is influenced by information asymmetry between a physician and a patient, where it is assumed that the physician has more knowledge about diagnostic and treatment options than the patient. Asymmetry of information can also be influenced by the physician's own clinical experiences, expertise, and professional judgment as sometimes a patient will request their physician's personal opinion to aid them in making a healthcare decision.[6] A physician who is a "perfect agent" is one who would make recommendations for a patient that the patient would make for themselves if they had the same information.[7] SID can occur because of a breakdown in this agency relationship and happens when a physician recommends or encourages a patient to consume more care than is required for their medical problem, for example, ordering tests that the physician knows are not needed to make a diagnosis or ordering treatments that the physician knows will have minimal benefit.

Explanatory theories
Target income hypothesis
The target income hypothesis suggests that a physician is motivated to maintain a certain level of desired income (the target) and if their actual income falls below this level, they will then modify their behavior to restore their income back up to the target.[8] Behavior modifications may include alterations in the physician's recommendations to patients as to the extent or appropriateness of diagnostic and treatment modalities in order to produce additional income to meet the target. Obstetricians who recommend C-sections as a standard of care for delivering babies may be using their power and authority over pregnant women and their partners as a revenue generator to reach or maintain their target income.[9][10] Jonathan Gruber and Maria Owings looked at the relationship between physician financial incentives and cesarean section delivery by examining declining fertility rates in the United States.[11] The fee-for-service (FFS) physician incentive structure makes it easier for SID to occur since it rewards the physician for increasing the quantity of services delivered rather than for the actual quality of the services; this could induce the physician to offer a higher number of services than would be the optimal amount for the patient in order to increase revenue. Some of the proposed healthcare models in the Patient Protection and Affordable Care Act (PPACA) could modify how a physician is reimbursed for delivering care that would reward quality over quantity thereby reducing SID. One of these models, the Accountable care organization (ACO), reimburses a physician through a gain-sharing model that encourages them to collaborate with other providers to deliver care thus removing some of the individual incentives to induce demand.[12] Pay for performance may also provide a strategy to discourage overuse of unnecessary, low-value interventions by reimbursing for quality of care delivered.[13]
Professional uncertainty hypothesis
The professional uncertainty hypothesis suggests that due to autonomy and individual practice patterns, physicians differ in their opinions regarding the effectiveness, appropriateness, and success rates of various treatment options for a particular condition. This leads to a level of uncertainty which may result in a lack of uniformly acceptable standards of care that can be followed by all physicians. This uncertainty may lead to different levels of recommended consumption (demand) to patients for healthcare services.[14] The use of evidence-based guidelines based on scientific evidence of improved outcomes for the diagnosis and treatment of a particular condition may reduce some physician autonomy but have a greater impact in reducing the professional uncertainty that may lead to SID.[15]
Variations in care and SID
It is unclear the extent to which SID explains geographic variations in care. It is a complicated topic. It is difficult to know how much is done explicitly to raise a physician's income and how much is practice style or professional uncertainty. Physicians who are more entrepreneurial may be interested in maximizing income. Surgeons may have more opportunity to manipulate demand. They may be more enthusiastic about certain procedures they perform because they generate more revenue or because they value the surgical treatment.[16]
Overutilization
The simple adage, "if you build it they will come," applies to SID and the medical profession. It appears when resources are available, overutilization occurs even when improved quality and outcomes are uncertain. This occurs daily in hospital intensive care units, at primary care physician offices and with overutilization of expensive radiologic technology and laboratory testing.[17] "Research suggests that those who invest in imaging equipment order more CT and MRI tests than doctors who haven't made the investment."[18] Analysts report that physicians reflexively respond to receiving positive test results by ordering more tests. Variation in medical practices can result in SID without producing increased quality outcomes. When standardized treatment pathways are unavailable to agents and principals a degree of uncertainty exists resulting in increased requests for unwarranted services. As a result, overutilization of supplies and services may occur without evidence of improved quality.[19]
Due to the number of contributing factors for the consumption of healthcare resources, it is difficult to isolate instances of supplier induced demand. However, there are many reasons for SID in healthcare that are important to understand including reimbursement rates, competition,[20] physician incentives and practices.[21] Increased levels and costs of technology, as well as changing practices[22] and the lack of evidence-based medicine or defined standards of care[23] allow more room for supplier induced demand. To further elaborate, take the example of PSA (prostate specific antigen) testing and early stage prostate cancer. Published guidelines have varied over the past few decades enough to cause doubt in a true standard of care.[24] With a number of treatment options including minimal to no healthcare interventions (watchful waiting, active surveillance, surgery, radiation therapy, etc.), patients may be influenced by providers to consume more healthcare than they would have otherwise given the asymmetry of information and marketing of treatment options from hospitals, physicians and industry. Externalities which influence supplier induced demand include direct to consumer marketing[25][26] and patient susceptibility to marketing to the extent that demand induced supply[27] is now being documented in health economics.
New technology and overutilization
Physicians are by nature and duty patient advocates, guiding the patient through joint decision making. This in part stems from a large knowledge differential between the two, a term known as asymmetric information, and evidenced by the differential between patients and physicians' interpretation of medical terms, underscoring the need for physicians to cross examine patients to verify whether they understand the terminology used in the clinical encounter.[28] While the physician bears the brunt of the knowledge differential, the patient is also responsible for sharing their entire medical history, concerns, barriers to and preferences for treatment in order for the physician to be an effective advocate for their health .[29] In effect, the patient provides all relevant information to the physician and relies on the physician to make the clinical decisions for them. This relationship requires a great deal of trust on the part of the patient, assuming that the clinical decisions made solely focus on patient health.
However, a physician's behavior may also be influenced by their desired income level. The current system is oriented towards fee for service, punishing lower utilization and rewarding overutilization through increased revenue. Physicians may use their knowledge differential and influence over patients to increase utilization of imaging or screening services, given the potential financial rewards.
The behaviors seen in supplier induced demand in healthcare have contributed to our current overuse of imaging and diagnostic tests, which has resulted in an upward spiraling of medical costs projected to equal 20% of our GDP by 2015.[30] The advent of newer technology has not only led to improvements in care, but also to potentially unnecessary screening and diagnostic testing possibly influenced by financial incentives to referring physicians, practice behavior of referring physicians, US health system, comparative effectiveness research, appropriateness criteria, and quality gaps in evidence-based care.[31] It has been suggested that fragmented care processes, imperfect patient memory, and lack of electronic medical records also contribute to the overutilization of imaging services.[32] As a result, imaging services and physicians' reliance on these technologies have increased at a dramatically higher rate than other technologies.[33][34] Advancements in imaging have broadened their application, increasing uptake. For instance, positron-emission technology (PET) is now used in oncology and degenerative diseases of the central nervous system.[35] Similarly, overutilization is evidenced in the promotion of CT scans for private offices.[36]
As physician owned surgical centers and specialty hospitals increasingly use imaging services, insurers question the cost benefit ratio of the technology. Data also suggests that physicians tend to refer well insured patients to physician owned facilities, while referring Medicaid patients to hospital outpatient clinics,[37] thus financial incentives to self-refer to physician owned facilities may affect the referral patterns of less financially beneficial patients. As pointed out in one case, it is difficult to identify this type of overutilization "fraud". In the high-profile case of Dr. Mark Midei, he inserted cardiac stents in over 500 patients whose artery occlusion rates did not warrant surgical intervention according to standards of care. The hospital Dr. Midei practiced at agreed to pay $22 million fine to settle charges.[38][39]
Another cardiologist in Louisiana was sentenced to 10 years in prison, convicted on 51 counts of billing private and government health insurers for unnecessarily implanting cardiac stents, and the hospital he practiced at was forced to pay a $3.8 million settlement to the Department of Justice and $7.4 million class action lawsuit.
Another contributing factor to overutilization is a lack of real time cost available to both the physician and the patient. Physicians are unable to ascertain the true cost of a screening, imaging, or lab test thereby making it difficult for them to determine how much they are charging the system.[40][41] Effects of overutilization on patients can include unnecessary radiation exposure and false positive results.[42] Initiatives are underway to curtail excessive screenings that have been deemed unnecessary, such as limiting prostate cancer screening as the United States Preventive Services Task Force recently found inadequate evidence to determine whether treatment for prostate cancer detected by screening actually improves health outcomes.[43] Studies in geographic variation have shown no difference in patient outcomes between physicians who practice in high cost areas and those who practice in low cost areas.[44]
A 2009 American Board of Radiology Foundation summit to address overutilization also identified defensive medicine and patients as contributory factors to the issue. Defensive medicine is an order for imaging as a result of potential malpractice, rather than benefit to the patient.[45] It has been estimated to account for 5-25% of all imaging costs. Patient demand often stems from little financial responsibility for costs associated with imaging, as well as information from other individuals, radio, the media, and the Internet with disproportionate understanding of the implications of imaging (further testing, exposure to radiation). Patients are being targeted to "self-present" to imaging facilities for uncovered imaging services that claim to offer screen for undetected coronary artery disease and cancer in the lungs and other organs.[46] However, the false positives observed for CT screening of coronary artery disease are similar to the levels of other noninvasive tests for ischemic heart disease[47] and some data indicate these services do not yield more precise results.[48] For instance, data from electron-beam CT did not outperform the Framingham Risk Index for predicting coronary events.8 Researchers suggest that the use of CT scanning for cancer screening cannot offer patients complete "peace of mind" as there are still issues of sensitivity and specificity, raising concerns over the implications of false negatives.
Concerns over overutilization of diagnostic tests have prompted the definition of "high value care" as the health benefits of an intervention justifies its harms and costs.[49] Some examples of low value care include a repeat ultrasonography for abdominal aortic aneurysm following a negative study or screening low risk individuals for hepatitis B virus infection.[50] Routine low back pain imaging is another area of overutilized imaging.[51] To curb future costs, it has also been proposed to include stewardship of resources (avoiding the overuse and misuse of diagnostic tests) as a general competency of the Accreditation Council for Graduate Medical Education/American Board of Medical Specialties for residency training and evaluation.12 Value based insurance design and personalized medicine are other methods being touted as solutions to bending the cost curve and reducing overutilization.[52][53]
Physician-owned facilities
In one report that identified the influence of the location of care delivery on SID, it was found that physicians were more likely to treat the low-severity patients at their physician-owned facility rather than to increase the overall number of procedures that were done in the population in order to increase revenue.[54]
Geography
Variation may also exist from regional or local community practice, and utilization of healthcare services can vary widely. McAllen, Texas, is one of the most expensive healthcare markets in the U.S., where in 2006 Medicare spent $15,000 per enrollee here, which was almost twice the national average.[55]
Direct-to-consumer advertising Three out of four patients who ask a physician about a particular medication have that medication prescribed to them because they saw advertising for it.[56] This results in a change in prescribing habits such that a physician will prescribe the more expensive requested medication rather than a lower price generic alternative.[57] Advertising for cosmetic surgery services can influence patients and physicians, extending even into the area of cosmetic gynecology where outcomes are unproven.[58]
Ethical concerns
The growing trend of "boutique" or "concierge" primary care physicians who advertise "more personal care" can be viewed as an example of SID. Concierge medicine is based on an annual fee paid by the consumer. Proponents believe this model will increase the quality of care delivered to those individuals who subscribe to it. Opponents argue it creates a two tier system, with better care for those who can afford it.[59][60][61]
SID can be associated with Medicare fraud and can be a prosecutable offense for reasons that include conducting and billing for unnecessary medical procedures in patients who have little or no disease.[62][63] Another ethical concern is the rise in healthcare spending that can be caused by SID.[64] SID may also be influenced by moral hazard where consumption of healthcare services may be increased when an individual's responsibility for the cost of a treatment is low.[65]
Economics of healthcare reform
The number of physicians entering primary care practice decreases, while the number of specialists increases. Thus, despite the growing number of patients who are demanding access to healthcare, there continues to be a greater supply of specialists, and fewer primary care physicians. This phenomenon leads to greater costs and strain in the system in terms of unnecessary procedures, less access and consumer apathy on cost of care within an already fragmented healthcare system. Additionally, many economists question whether or not doctors use their relationship with the patient for their own financial advantage by recommending and providing health services that the patient would have refused if well informed.[66] This concept is referred to as supplier induced demand.
Access to care challenges are exacerbated by the introduction of the baby boomers into the healthcare system. The aging boomer population is just now reaching the age of 65 and becoming eligible for Medicare. At the same time, fee for service reimbursement from the public payers, followed by the private payers is declining. Not only is the number of primary care physicians dwindling, but this decline in reimbursement causes many of these physicians to reduce the number of appointment slots for Medicare patients. This growing barrier to primary care physicians and the preventive care they provide means that more patients are being seen in less appropriate and less efficient venues of care (such as emergency rooms).[67]
However, the passage of the Patient Protection and Affordable Care Act (PPACA) and the recent SCOTUS affirmation of the individual mandate attempt to solve some of the challenges behind the current supplier induced demand. This includes Section 3021 of the Act, which calls for the development of a Center of Medicare and Medicaid Services Innovation Center (CMMI). This new Center fosters health care transformation by finding new ways to pay for and deliver care that improves quality and health while lowering costs.[68] These innovative models of payment and care service delivery include care for Medicare, Medicaid and CHIP beneficiaries using an open, transparent, and competitive process. Other provisions of PPACA include the establishment of additional methods designed to move the current system from volume (fee for service) to value (outcomes based payment), such as the Medicare Shared Savings Program. Standard economic theory makes no allowance at all for the possibility that the supplier would influence the position of the demand curve.
The patient's role in supplier induced demand has not gone ignored by public or private stakeholders. There are numerous efforts underway to understand how to involve the consumer in shared decision making and taking responsibility for health that may contribute to supplier induced demand.[69] The development of the Patient Centered Outcomes Research Institute (PCORI) was created to conduct research to provide information about the best available evidence to help patients and their health care providers make more informed decisions. PCORI's research is intended to give patients a better understanding of the prevention, treatment and care options available, and the science that supports those options. PCORI was established by Congress through the 2010 Patient Protection and Affordable Care Act but is by law an independent, non-profit organization.[70]
Lastly, reimbursement for providers is mostly on a fee for service basis and services rendered are paid for on an individual basis. There is no limit to the number of services rendered, or expectation that payment is based on any particular outcome. In recent years however, attention has been paid to entities in the industry (payer or payer/provider collaborations) who have innovated on different ways to pay for services rendered which depend entirely on outcomes. These methods hold all parties accountable for the outcomes of the services rendered.
See also
References
- LaBelle, R.; Stoddart, G.; Rice, T. (1994). "A re-examination of the meaning and importance of supplier-induced demand". Journal of Health Economics. 13 (3): 347–368. doi:10.1016/0167-6296(94)90036-1. PMID 10138860.
- Richardson, Jeff; Peacock, Stuart (July 1999). "Supplier Induced Demand Reconsidered" (PDF). Centre for Health Evaluation Working Paper 81.
- "Supplier Induced Demand".
- LaBelle, R.; Stoddart, G.; Rice, T. (1994). "A re-examination of the meaning and importance of supplier-induced demand". Journal of Health Economics. 13 (3): 347–368. doi:10.1016/0167-6296(94)90036-1. PMID 10138860.
- Donaldson, C. & Gerard, K. (1993). Economics of health care financing: the visible hand (pp.116-117). New York, NY: St. Martin's Press.
- Richardson, J.; Peacock, S. (2006). "Supplier-induced demand: Reconsidering the theories and new Australian evidence". Applied Health Economics and Health Policy. 5 (2): 87–98. doi:10.2165/00148365-200605020-00003. PMID 16872250.
- Folland, S., Goodman, A., &Stano, M. (2012). The economics of health and health care (7thed.) (pp. 305-308). Boston, MA: Pearson.
- Folland, S., Goodman, A., &Stano, M. (2012). The economics of health and health care (7thed.) (pp. 305-308). Boston, MA: Pearson.
- Folland, S., Goodman, A.C., & Stano, M. (2013). The Physician's Practice in The Economics of Health and Health Care. Boston: Pearson. pp. Chp 15.CS1 maint: multiple names: authors list (link)
- Sakala, Carol (1993). "Medically unnecessary cesarean section births:Introduction to a symposium". Social Science & Medicine. 37 (10): 1177–1198. doi:10.1016/0277-9536(93)90331-W. PMID 8272898.
- Gruber, J; Owings, M. (1996). "Physician Financial Incentives and Cesarean Section Delivery" (PDF). The RAND Journal of Economics. Spring. 27 (1): 99–123. doi:10.2307/2555794. JSTOR 2555794. PMID 10160536.
- Shafrin, J. (January 26, 2010). "What are Accountable Care Organizations?". Check date values in:
|year= / |date= mismatch(help) - Enthoven, A (2009). "Integrated delivery systems: the cure for fragmentation". The American Journal of Managed Care. 15: S284–S290. PMID 20088632.
- Wennberg, J.; Barnes, B.; Zubkoff, M. (1982). "Professional uncertainty and the problem of supplier-induced demand". Social Science and Medicine. 16 (7): 811–824. doi:10.1016/0277-9536(82)90234-9. PMID 7100999.
- Reinertsen, J. (2003). "Zen and the art of physician autonomy maintenance". Annals of Internal Medicine. 138 (12): 992–995. doi:10.7326/0003-4819-138-12-200306170-00011. PMID 12809456.
- "The Incidental Economist Blog".
- Mulley, A.G. (2009). "Inconvenient truths about supplier induced demand and unwarrented variation in medical practice". BMJ. 339: b4073. doi:10.1136/bmj.b4073. PMID 19843566.
- "Consumer Reports". June 2012.
- Mulley, A.G. (2009). "Inconvenient truths about supplier induced demand and unwarrented variation in medical practice". BMJ. 339 (339): b4073. doi:10.1136/bmj.b4073. PMID 19843566.
- Richardson, JR; Peacock, SJ (2006). "Supplier-induced demand: reconsidering the theories and new Australian evidence". Appl Health Econ Health Policy. 5 (2): 87–98. doi:10.2165/00148365-200605020-00003. PMID 16872250.
- Heaton, P. "Does treatment respond to reimbursement rates? Evidence from trauma care" (PDF). Retrieved 2008. Check date values in:
|access-date=(help) - Steinberg, M.L.; Konski, A. (2009). "Proton beam therapy and the convoluted pathway to incorporating emerging technology into routine medical care in the United States". The Cancer Journal. 15 (4): 333–338. doi:10.1097/ppo.0b013e3181af5b5c. PMID 19672151.
- Wennbert, J.E.; Barnes, B. A.; Zubkoff, M. (1982). "Professional uncertainty and the problem of supplier-induced demand". Social Science & Medicine. 16 (7): 811–824. doi:10.1016/0277-9536(82)90234-9. PMID 7100999.
- 6. US. Preventive Services Task Force (2012). "Screening for Prostate Cancer: U.S. Preventive Services Task Force Recommendation Statement".
- "Frequently Asked Questions-Health Economics". National Conference of State Legislatures. 2006.
- "Prescription Drugs and Mass Media Advertising, 2000" (PDF). The National Institute for Health Care Management: Research and Educational Foundation. 2001.
- Shih, Y; Tai-Seale, M. (2012). "Physicians' perception of demand-induced supply in the information age: a latent class model solution". Health Economics. 21 (3): 252–269. doi:10.1002/hec.1710. PMID 21280137.
- Boyle, C (1970). "Difference between Patients' and Doctors' Interpretation of Some Common Medical Terms". British Medical Journal. 2 (5704): 286–289. doi:10.1136/bmj.2.5704.286. PMC 1700443. PMID 5420179.
- "A Doctor's Duty to Patient Advocacy Blog".
- "Congress of the United States. (2008). Budget options. Vol 1, Health care. Washington, DC: Congressional Budget Office". Missing or empty
|url=(help) - Hendee, W (2010). "Addressing overutilization in medical imaging". Radiology. 257 (1): 240–245. doi:10.1148/radiol.10100063. PMID 20736333.
- Fuchs, V (2001). "Physicians' view of the relative importance of thirty medical innovations". Health Affairs. 20 (5): 30–42. doi:10.1377/hlthaff.20.5.30. PMID 11558715.
- "Overutilization of imaging services: causes, costs, and opportunities".
- Igelhart, J (2006). "The new era of medical imaging-progress and pitfalls". NEJM. 354 (26): 2822–2828. doi:10.1056/nejmhpr061219. PMID 16807422.
- Juweid, M (2006). "Positron-emission tomography and assessment of cancer therapy". NEJM. 354 (5): 496–507. doi:10.1056/nejmra050276. PMID 16452561.
- "Advertisement to physicians encouraging overutilization - "Capitalize on imaging opportunities in urology".
- Gabel, J (2008). "Where do I send thee? Does physician ownership affect referral patterns to ambulatory surgery centers?". Health Affairs. 27 (3): 165–174. doi:10.1377/hlthaff.27.3.w165. PMID 18349040.
- "The Curious Case of Dr. Midei - Medical Over-Utilization or Fraud?".
- "White Paper: Overutilization, Abuse and Fraud within Cardiac Departments" (PDF).
- Brooke, R (2012). "Do physicians need a shopping cart for healthcare services?". JAMA. 307 (8): 791–792. doi:10.1001/jama.2012.204. PMID 22357829.
- Mitka, M (2011). "Price of healthcare services". JAMA. 306 (22): 2443. doi:10.1001/jama.2011.1764.
- "CT scans and x-rays draw patients into risk and overutilization". 2010-12-28.
- "Screening for prostate cancer".
- "The High Cost of Health Care". New York Times.
- Lee, T (2002). "Direct to consumer marketing of high-technology screening tests". NEJM. 346 (7): 529–531. doi:10.1056/nejm200202143460715. PMID 11844859.
- O'Rourke, R (2000). "American College of Cardiology/American Heart Association Expert Consensus document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease". Circulation. 102 (1): 126–140. doi:10.1161/01.cir.102.1.126. PMID 10880426.
- Detrano, R (1999). "Coronary calcium does not accurately predict near-term future coronary events in high-risk adults". Circulation. 99 (20): 2633–2638. doi:10.1161/01.cir.99.20.2633. PMID 10338455.
- Owens, D (2011). "High value cost conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions". Annals of Internal Medicine. 154 (3): 174–180. doi:10.7326/0003-4819-154-3-201102010-00007. PMID 21282697.
- Qaseem, A (2012). "Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care". Annals of Internal Medicine. 156 (2): 147–149. doi:10.7326/0003-4819-156-2-201201170-00011. PMID 22250146.
- Chou, R (2011). "Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians". Annals of Internal Medicine. 154 (3): 181–189. CiteSeerX 10.1.1.690.1604. doi:10.7326/0003-4819-154-3-201102010-00008. PMID 21282698.
- Weinberger, S (2011). "Providing high value, cost conscious care: a critical seventh general competency for physicians". Annals of Internal Medicine. 155 (6): 386–388. CiteSeerX 10.1.1.672.8906. doi:10.7326/0003-4819-155-6-201109200-00007. PMID 21930856.
- Malis, N (2011). "Overhauling the reimbursement system for molecular diagnostics". Nature Biotechnology. 29 (5): 390–391. doi:10.1038/nbt.1869. PMID 21552233.
- Robinson, J (2011). "Applying value-based insurance design to high-cost health services" (PDF). Health Affairs. 29 (11): 2009–2016. doi:10.1377/hlthaff.2010.0469. PMID 21041740.
- Stensland, J.; Winter, A. (2006). "Do physician owned cardiac hospitals increase utilization?". Health Affairs. 25 (1): 119–129. doi:10.1377/hlthaff.25.1.119. PMID 16403751.
- Gawande, A. (June 1, 2009). "The cost conundrum: What a Texas town can teach us about health care". The New Yorker.
- Wosinska, M. (2002). "Just what the patient ordered? Direct-to-consumer advertising and the demand for pharmaceutical products | HBS Marketing Research Paper No. 02-04". Papers.ssrn.com. SSRN 347005. Missing or empty
|url=(help) - Bradford, W.D.; Kleit, A.N.; Nietert, P.J.; Steyer, T.; McIlwain, T.; Ornstein, S. (2006). "How direct-to-consumer television advertising for osteoarthritis drugs affects physicians' prescribing behavior". Health Affairs. 25 (5): 1371–1377. doi:10.1377/hlthaff.25.5.1371. PMID 16966735.
- Iglesias, C (2012). "Cosmetic gynecology and the elusive quest for the "perfect" vagina". Obstet. Gynecol. 119 (6): 1083–1084. doi:10.1097/aog.0b013e31825833f5. PMID 22617570.
- Folland, S., Goodman, A.C., & Stano, M. The Physician's Practice in The Economics of Health and Health Care. Boston: Pearson. pp. Chp 15.CS1 maint: multiple names: authors list (link)
- Zuger, Abigail (Oct 30, 2005). "For a Retainer, Lavish Care by "Boutique Doctors"". New York Times.
- Chen, Pauline W. (August 26, 2010). "Can Concierge Medicine for the Few Benefit the Many?". New York Times.
- O'Riordan, M. (June 26, 2009). "Cardiologist gets 10 years for performing unnecessary interventions". Theheart.org.
- "Louisiana cardiologist sentenced in federal court for performing unnecessary medical procedures" (PDF). United States Attorney's Office. June 4, 2009.
- Mulley, A. (2009). "Inconvenient truths about supplier induced demand and unwarranted variation in medical practice". BMJ. 339: 1007–1009. doi:10.1136/bmj.b4073. PMID 19843566.
- Van Dijk, C.; den Berg, B.; Verhei, R; Spreeuwenberg, P.; Groenewegen, P.; de Bakker, D. (2012). "Moral hazard and supplier-induced demand: Empirical evidence in general practice". Health Economics. 22 (3): 340–352. doi:10.1002/hec.2801. PMID 22344712.
- Gawande, A (June 1, 2009). "The cost conundrum".
- "Access to care. (n.d.)". Ama-assn.org.
- "Access to care. (n.d.)". Ama-assn.org.
- Pauly, M.; Sattherwaite, M. (1981). "The pricing of primary care physician's services: a test of the role of consumer information" (PDF). The Bell Journal of Economics. 12 (2): 488–506. doi:10.2307/3003568. JSTOR 3003568.
- "About us". Pcori.org. 2012.