Acute limb ischaemia
Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb.[1]
| Acute limb ischaemia | |
|---|---|
| Other names | Acute limb ischemia |
 | |
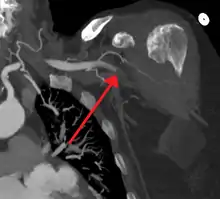
| Acute embolism to the right femoral artery resulting in ischemia | |
| Symptoms | Cold, painful, pulseless limb that cannot move |
| Causes | Embolism, thrombosis |
| Treatment | Thrombectomy, embolectomy, thrombolysis |
| Medication | Thrombolytic drugs |
Acute limb ischaemia is caused by embolism or thrombosis, or rarely by dissection or trauma.[2] Thrombosis is usually caused by peripheral vascular disease (atherosclerotic disease that leads to blood vessel blockage), while an embolism is usually of cardiac origin.[3] In the United States, ALI is estimated to occur in 14 out of every 100,000 people per year.[4] With proper surgical care, acute limb ischaemia is a highly treatable condition; however, delayed treatment (beyond 6 to 12 hours) can result in permanent disability, amputation, and/or death.
In contrast to acute limb ischemia, chronic limb threatening ischemia results from peripheral artery disease that develops over time. While limbs in both acute and chronic limb ischemia may be pulseless, a chronically ischemic limb is typically warm and pink due to a well-developed collateral artery network and does not need emergency intervention to avoid limb loss.[5]
The New Latin term ischaemia as written, is a British version of the word ischemia, and stems from the Greek terms ischein 'to hold'; and haima 'blood'.[6] In this sense, ischaemia refers to the inhibition of blood flow to/through the limb.
Signs and symptoms
Acute limb ischaemia can occur in patients through all age groups. People who smoke tobacco cigarettes and have diabetes mellitus are at a higher risk of developing acute limb ischaemia. Most cases involve people with atherosclerosis problems.[7]
Symptoms of acute limb ischaemia include:
- Pain
- Pallor (pale appearance of the limb)
- Paresthesias (abnormal sensations in the limb)
- Perishingly cold
- Pulselessness
- Paralysis
These symptoms are called "the six P's'";[8][9][10] they are commonly mis-attributed to compartment syndrome. One more symptom would be the development of gangrene. Immediate medical attention should be sought with any of the symptoms.[1]
In late stages, paresthesia is replaced by anesthesia (numbness) due to death of nerve cells.
In some cases, gangrene can occur within six hours of ischaemia.
Related conditions
When a limb is ischaemic in the non-acute (chronic) setting, the condition is alternatively called peripheral artery disease or critical limb ischaemia, rather than ALI. In addition to limb ischaemia, other organs can become ischaemic, causing:
- Renal ischemia (nephric ischaemia)
- Mesenteric ischaemia
- Cerebral ischaemia
- Cardiac ischaemia
Diagnosis
In order to treat acute limb ischaemia there are a series of things that can be done to determine where the occlusion is located, the severity, and what the cause was. To find out where the occlusion is located one of the things that can be done is simply a pulse examination to see where the heart rate can be detected and where it stops being sensed. Also there is a lower body temperature below the occlusion as well as paleness. A Doppler evaluation is used to show the extent and severity of the ischaemia by showing flow in smaller arteries. Other diagnostical tools are duplex ultrasonography, computed tomography angiography (CTA), and magnetic resonance angiography (MRA). The CTA and MRA are used most often because the duplex ultrasonography although non-invasive is not precise in planning revascularization. CTA uses radiation and may not pick up on vessels for revascularization that are distal to the occlusion, but it is much quicker than MRA.[1] In treating acute limb ischaemia time is everything.
In the worst cases acute limb ischaemia progresses to critical limb ischaemia, and results in death or limb loss. Early detection and steps towards fixing the problem with limb-sparing techniques can salvage the limb. Compartment syndrome can occur because of acute limb ischaemia because of the biotoxins that accumulate distal to the occlusion resulting in edema.[1]
Treatment
Surgery
The primary intervention in acute limb ischaemia is emergency embolectomy using a Fogarty Catheter, providing the limb is still viable within the 4-6h timeframe.[11] Other options include a vascular bypass to route blood flow around the clot.[12]

Medications
Those unsuitable for surgery may receive thrombolytics. In the past, streptokinase was the main thrombolytic chemical. More recently, drugs such as tissue plasminogen activator, urokinase, and anisterplase have been used in its place. Mechanical methods of injecting the thrombolytic compounds have improved with the introduction of pulsed spray catheters—which allow for a greater opportunity for patients to avoid surgery.[13][14] Pharmacological thrombolysis requires a catheter to be inserted into the affected area, attached to the catheter is often a wire with holes to allow for a wider dispersal area of the thrombolytic agent. These agents lyse the ischemia-causing thrombus quickly and effectively.[15] However, the efficacy of thrombolytic treatment is limited by hemorrhagic complications. Plasma fibrinogen level has been proposed as a predictor of these hemorrhagic complications. However, based on a systematic review of the available literature until January 2016, the predictive value of plasma is unproven.[16]
Mechanical thrombolysis
Another type of thrombolysis disrupts the clot mechanically using either saline jets or, more recently, ultrasound waves. Saline jets dislodge the clot using the Bernoulli effect. Ultrasound waves, emitted at low frequency, create a physical fragmentation of the thrombus.[17]
Considerations in treatment
The best course of treatment varies from case to case. The physician must take into account the details in the case before deciding on the appropriate treatment. No treatment is effective for every patient.
Treatment depends on many factors, including:
- Location of lesions
- Anatomy of lesions
- Individual risk factors
- Procedural risk
- Clinical presentation of symptoms
- Duration of symptoms
- etc.[13]
Epidemiology
The major cause of acute limb ischaemia is arterial embolism (80%), while arterial thrombosis is responsible for 20% of cases. In rare instances, arterial aneurysm of the popliteal artery has been found to create a blood clot or embolism resulting in ischaemia.[18]
References
- Walker T. Gregory (2009). "Acute Limb Ischemia". Techniques in Vascular and Interventional Radiology. 12 (2): 117–129. doi:10.1053/j.tvir.2009.08.005. PMID 19853229.
- Creager, Mark A.; Kaufman, John A.; Conte, Michael S. (2012). "Acute Limb Ischemia". New England Journal of Medicine. 366 (23): 2198–2206. doi:10.1056/NEJMcp1006054. PMID 22670905.
- Klonaris, C; Georgopoulos, S; Katsargyris, A; Tsekouras, N; Bakoyiannis, C; Giannopoulos, A; Bastounis, E (March 2007). "Changing patterns in the etiology of acute lower limb ischemia". International Angiology : A Journal of the International Union of Angiology. 26 (1): 49–52. PMID 17353888.
- Dormandy J, Heeck L, Vig S (June 1999). "Acute limb ischemia". Semin Vasc Surg. 12 (2): 148–53. PMID 10777242.
- Farber, A (12 July 2018). "Chronic Limb-Threatening Ischemia". The New England Journal of Medicine. 379 (2): 171–180. doi:10.1056/NEJMcp1709326. PMID 29996085.
- "Ischaemia." Merriam-Webster. Last modified 2012. http://www.merriam-webster.com/dictionary/ischemia?show=0&t=1334804041
- Brooks Marcus; Jenkins Michael P (2008). "Acute and chronic ischaemia of the limb". Surgery (Oxford). 26 (1): 17–20. doi:10.1016/j.mpsur.2007.10.012.
- Brearley, S (May 8, 2013). "Acute leg ischaemia". BMJ (Clinical Research Ed.). 346: f2681. doi:10.1136/bmj.f2681. PMID 23657181.
- "CKS is only available in the UK". NICE. Retrieved 2020-10-15.
- "Acute Limb Ischaemia - Clinical Features - Management". TeachMeSurgery. Retrieved 2020-10-15.
- Goldberg, Andrew (2012). Surgical Talk: Lecture Notes in Undergraduate Surgery. Imperial College Press. p. 234. ISBN 978-1-84816-6141.
- Bowley, Douglas, and Andrew Kingsnorth, eds. Fundamentals of Surgical Practice: A Preparation Guide for the Intercollegiate Mrcs Examination. 3rd ed. N.p.: Cambridge University Press, 2011. 506-11. Web. 20 Apr. 2012.
- Andaz S.; Shields D.A.; Scurr J.H.; Smith P.D. Coleridge (1993). "Thrombolysis in acute lower limb ischaemia". European Journal of Vascular Surgery. 7 (6): 595–603. doi:10.1016/S0950-821X(05)80702-9. PMID 8270059.
- ABC of Arterial and Venous Disease: Acute Limb Ischaemia Ken Callum and Andrew Bradbury BMJ: British Medical Journal, Vol. 320, No. 7237 (Mar. 18, 2000), pp. 764-767
- Wardlaw J.M.; Warlow C.P. (1992). "Thrombolysis in acute ischemic stroke: does it work?". Stroke. 23 (12): 1826–1839. doi:10.1161/01.str.23.12.1826.
- Poorthuis, Michiel H. F.; Brand, Eelco C.; Hazenberg, Constantijn E. V. B.; Schutgens, Roger E. G.; Westerink, Jan; Moll, Frans L.; de Borst, Gert J. (2017-03-05). "Plasma fibrinogen level as a potential predictor of hemorrhagic complications after catheter-directed thrombolysis for peripheral arterial occlusions". Journal of Vascular Surgery. 65 (5): 1519–1527.e26. doi:10.1016/j.jvs.2016.11.025. ISSN 1097-6809. PMID 28274749.
- Sean P. Lyden, Endovascular Treatment of Acute Limb Ischemia: Review of Current Plasminogen Activators and Mechanical Thrombectomy Devices PERSPECT VASC SURG ENDOVASC THER December 2010 22: 219-222, first published on March 16, 2011
- Mitchell ME, Carpenter JP. Overview of acute arterial occlusion of the extremities (acute limb ischemia). In: Post TW, ed. UpToDate. Waltham, MA: UpToDate. https://www.uptodate.com/contents/overview-of-acute-arterial-occlusion-of-the-extremities-acute-limb-ischemia?source=search_result&search=Classification%20of%20acute%20extremity%20ischemia&selectedTitle=1∼90#H506059593. Last updated May 31, 2016. Accessed December 13, 2016.