Autotransplantation
Autotransplantation is the transplantation of organs, tissues, or even particular proteins from one part of the body to another in the same person (auto- meaning "self" in Greek[1]).
| Autotransplantation | |
|---|---|
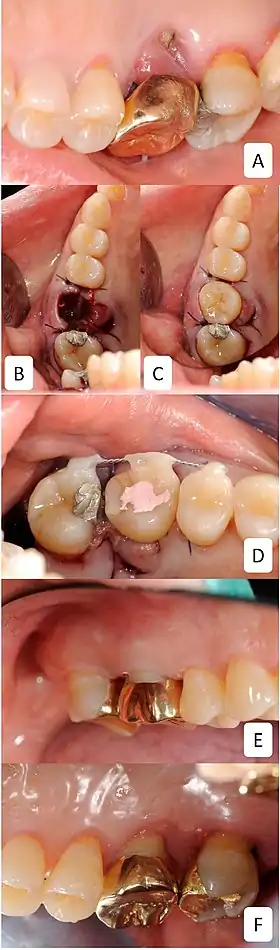 Autotransplantation of wisdom tooth | |
| MeSH | D014182 |
The autologous tissue (also called autogenous, autogeneic, or autogenic tissue) transplanted by such a procedure is called an autograft or autotransplant.[2]
It is contrasted with allotransplantation (from other individual of same species), Syngeneic transplantation (Grafts transplanted between two genetically identical individuals of the same species) and xenotransplantation (from other species).
A common example is the removal of a piece of bone (usually from the hip) and its being ground into a paste for the reconstruction of another portion of bone.
Autotransplantation, although most common with blood, bone, or skin, can be used for a wide variety of organs. One of these rare examples is autotransplantation of a kidney from one side of the body to the other. Kidney autotransplantation is used as a treatment for nutcracker syndrome.[3]
Autologous blood donation
In blood banking terminology, autologous blood donation refers to a blood donation marked for use by the donor, typically for a scheduled surgery. (Generally, the notion of "donation" does not refer to giving to oneself, though in this context it has become somewhat acceptably idiomatic.) They are commonly called "Autos" by blood bank personnel, and it is one major form of the more general concept of autotransfusion (the other being intraoperative blood salvage).
Some advantages of autologous blood donation are:
- Blood type will always match, even with a rare blood type or antibody type.
- If only autologous blood is used during surgery the risk of exposure to infectious disease such as hepatitis or HIV from blood is eliminated.
- The risk of allergic reactions is reduced.
The disadvantages are:
- Higher cost due to individualized processing, record-keeping, and management.
- In most cases, the blood is discarded if it is not used instead of being added to the general supply.
- Blood donation prior to colorectal cancer surgery seemed causative for a worse overall and colorectal cancer specific survival.[4]
Autologous blood is not routinely tested for infectious diseases markers such as HIV antibodies. In the United States, autologous blood is tested only if it is collected in one place and shipped to another.
There is also a risk that, in an emergency or if more blood is required than has been set aside in advance, the patient could still be exposed to donor blood instead of autologous blood. Autologous donation is also not suitable for patients who are medically unable to or advised not to give blood, such as cardiac patients or small children and infants.[5]
Bone autograft

In orthopaedic medicine, bone graft can be sourced from a patient's own bone in order to fill space and produce an osteogenic response in a bone defect. However, due to the donor-site morbidity associated with autograft, other methods such as bone allograft and bone morphogenetic proteins and synthetic graft materials are often used as alternatives. Autografts have long been considered the "Gold Standard" in Oral Surgery and Implant Dentistry because it offered the best regenerations results. Lately, the introduction of morphogen-enhanced bone graft substitutes have shown to show similar success rates and quality of regeneration; however, their price is still very high.
See also
- Autotransfusion – the process of returning to a patient their own blood that has been lost.
- Replantation – reattaching a severed limb or other part of the body.[6]
- Rotationplasty – attaching the foot with ankle joint (reversed) to the femur to replace the knee.[7]
- Spleen transplantation - Splenic autotransplantation is possible
References
- "Definition of auto- in Greek | Dictionary.com". www.dictionary.com. Retrieved 2019-06-25.
- Andreasen, J.; Paulsen, HU; Yu, Z.; Ahlquist, R (1990). A long‐term study of 370 autotransplanted premolars. Part I. Surgical procedures and standardized techniques for monitoring healing. Eur J Orthod. pp. 12: 3– 13.
- Boodman, Sandra D. (October 24, 2020). "Stomach pain was ruining her life. Then a scan provided a life-changing clue". Washington Post.
- Harlaar, JJ; Gosselink, MP; Hop, WC; Lange, JF; Busch, OR; Jeekel, H (November 2012). "Blood transfusions and prognosis in colorectal cancer: long-term results of a randomized controlled trial". Annals of Surgery. 256 (5): 681–7. doi:10.1097/SLA.0b013e318271cedf. PMID 23095610. S2CID 35798344.
- Regina Hwang; Peter Liou; Tomoaki Kato (November 2018). "Ex vivo liver resection and autotransplantation: An emerging option in selected indications". Journal of Hepatology. 69 (5): 1037–1046. doi:10.1016/j.jhep.2018.09.005. PMID 30243765 – via Plum xMetrics.
- Li J; Guo Z; Zhu Q (2008). "Fingertip replantation: determinants of survival". Plastic and Reconstructive Surgery. Plast Reconstr Surg. 122 (3): 122:833–839. doi:10.1097/PRS.0b013e318180ed61. PMID 18766047. S2CID 25442316.
- Christie MJ; DeBoer DK; McQueen DA; Cooke FW; Hahn DL (2003). Salvage procedure for failed total knee arthroplasty. J Bone Joint Surg. pp. 85:58–62.