Black maternal mortality in the United States
The World Health Organization (WHO) defines maternal mortality as death that occurs during pregnancy and giving birth, or soon after. Black maternal mortality in the United States refers to the incidence of maternal mortality in the U.S. specifically for those identifying as black or African American. The usual causes of maternal mortality are conditions that occur or are exacerbated during a pregnancy. Therefore, most instances of maternal mortality are preventable deaths.[1] In the U.S., the CDC reported that black women experience maternal mortality at a rate two to three times higher than that of white women.[2] Researchers have identified several reasons for the black–white maternal mortality disparity in the U.S., including historical reasons, access to care, socioeconomic status, incidence of preexisting conditions, medical racism, and abortion access.
Maternal mortality rates
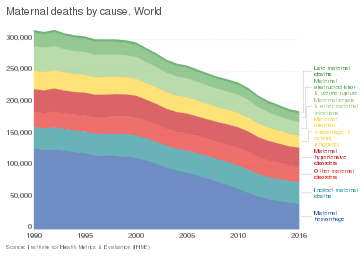
While maternal mortality rates in the United States remain relatively high compared to other developed countries, certain racial groups suffer maternal mortality at greater rates than others. In 2010, Black women had a maternal mortality rate that was three times higher than that of white women.[3] The estimated national maternal mortality rate in the United States is about 17 per 100,000–but is about 43 per 100,000 live births for Black women.[4] Furthermore, the authors cited data from the CDC Pregnancy Surveillance Study that showed these higher rates of Black maternal mortality are due to higher fatality rates, not a higher number, or incidence, of cases. This indicates that the higher maternal mortality rates among Black women is not due to a higher number of high-risk cases, but because Black women are more likely to die during or after giving birth. This same study found that the gap between Black and white maternal mortality has only increased over the past few decades.[3] A 2019 New York Times article reported that between 2000 and 2015, the national maternal mortality rate fell, but the Black maternal mortality rate increased.[5]
Causes
Historical context
An article in the American Journal of Public Health identified the effects of slavery on current maternal mortality. The authors describe that laws making enslavement an inheritable status increased the scrutiny of Black women and forced them into bearing children for the economic gain of their enslavers. In addition, many medical and surgical techniques were developed by exploiting the bodies of enslaved Black women. This legacy has persisted to modern times, and has made Black women less likely to trust the medical community.[6]
The practice of redlining, in which governments identified neighborhoods deemed to be risky investments, effectively blocked Black neighborhoods from accessing federal and bank loans. Due to this designation, only lower-quality hospitals persisted in these redlined neighborhoods, affecting the access of Black women to quality care to this day.[7] Although legal segregation ended in the 1960s, hospitals for Black people are still generally lower-quality than those targeted to higher-income, white people.[7]
The historical context of institutionalized racism in the US has also had the effect of making the Black community less likely to trust medical institutions and professionals.[7]
Access to prenatal and postnatal care
The purpose of prenatal care is to support pregnant women at an early stage, and monitor potential risk factors in order to make pregnancy and delivery as safe and healthy as possible. The literature shows that increasing access to prenatal care through public health departments caused a subsequent decrease in Black maternal mortality rates.[8] Furthermore, having fewer than 5 prenatal care visits, not attending prenatal care appointments, and accessing prenatal care later in a pregnancy are associated with maternal mortality. As Black women are more likely to begin prenatal care after their first trimester, this is a contributing factor to adverse maternal outcomes.[8]
The Center for American Progress published a report in 2019 that described "maternal care deserts", or areas where ob/gyn care is not available. The authors point out that women in rural areas and low-income areas have lower access to high-quality maternal health care, and lower access to hospitals in general, which necessarily decreases access to prenatal care.[9] Other obstacles such as lack of providers accepting public insurance such as Medicaid and transportation requirements to get to prenatal appointments affect Black women more than white women in the United States.[8]
In terms of postpartum care, Black women are about 5% less likely to seek out postpartum mental health care, and are additionally less likely than white women to follow up with continued care. These results occurred after controlling for income.[10]
Intersection of race and socioeconomic status
Income has been well studied as a social determinant of health, and it has been found that worse health outcomes at all-time points surrounding pregnancy are associated with lower socioeconomic status and income levels. Lack of insurance or using Medicaid, and experiencing homelessness are associated with severe morbidity rates, and are all more likely to apply to Black women and increase their risk of maternal death.[8]
Systemic racism contributes to the greater likelihood of Black women to belong to lower socioeconomic classes. A study from the Nature Public Health Collection journal pointed out that the COVID-19 pandemic increases the vulnerability of Black women who are more likely to work at jobs that carry greater exposure risks to COVID-19, and more likely to lose income due to unemployment. This is in addition to the pandemic making accessing perinatal care more challenging, and making income disparities even more stark. The researchers who authored this study recommend that the interlocking factors affecting Black mothers during the COVID-19 pandemic be specifically addressed in order to see tangible improvements in maternal health outcomes.[11]
Pre-existing conditions
A study conducted by Amy Metcalfe, James Wick, and Paul Ronksley analyzing trends in maternal mortality from 1993 to 2012 showed that the percentage of Black women with pre-existing conditions increased from about 10% to about 17%, the highest out of all other racial and ethnic groups in the United States. On top of this, Black women are more likely to have unplanned pregnancies–and are thus more likely to lack prior monitoring and treatment of pre-existing conditions before, during, and after the pregnancy.[3]
A different study by Deirdre Owens and Sharla Fett points out that everyday and institutional racism against Black people can affect the health of Black women, and increase their risk of high blood pressure, which in turn increases the risk of eclampsia, a main cause of pregnancy-related death.[6]
Racism
The Metcalfe, et al study analyzing trends in maternal mortality in the US over time cited evidence of the effect of structural racism on increasing Black maternal mortality.[3] One manifestation of this is in the lower quality of hospitals that Black women tend to visit in comparison to white women, and the hospitals Black women frequent tend to report higher rates of maternal morbidity. In addition, Black and white patients are treated differently by healthcare professionals. Black women, in addition to other racial minorities, are less like to be treated with induced labor than white women.[3]
Another phenomenon contributing to Black maternal mortality is the dismissal of Black women's pain by medical professionals.[6] A Harvard School of Public Health publication discussed this phenomenon by collecting numerous examples of medical professionals being dismissive or providing delayed care to Black mothers expressing pain or problematic symptoms.[12] The publication tells the story of Shalon Irving, a Black woman who experienced symptoms such as high blood pressure, blurry vision, and hematoma after childbirth. However, her doctors advised her to not take further action, and Irving died soon after. According to the author, this was just one instance of medical caregivers being less likely to take Black women's concerns seriously, contributing to maternal death.[12]
Abortion access
Unsafe abortion is a major contributor to maternal mortality and morbidity and Black women, who are more likely to have unplanned pregnancies and be of lower socioeconomic status, are more likely to undergo unsafe abortions. Access to safe abortions can be more difficult for women lacking transportation, insurance, or who may be enduring social stigmatization.[13]
Prevention
A large proportion of maternal deaths are thought to be preventable, and thus research has been conducted to identify methods to decrease maternal mortality and reduce disparities.
Some researchers looking at hospital quality believe that improving quality of care can help address the maternal mortality disparity in the United States. The authors of one article from the Seminars in Perinatology journal suggest that higher quality hospitals have administrative and physician advocates, collect and use feedback, and have substantial goals they want to achieve. In addition, the capacity for hospitals to offer maternal health-related services, such as an intensive care unit, 24-hour anesthesia, and ob/gyn specialists contributes to maternal mortality rates by hospital. Prioritizing standardizing care in times of crisis and early risk factors may also directly address issues that lead to maternal mortality in Black women, such as hypertension, hemorrhage, and eclampsia.[14] Notably, a 2018 initiative in New York City attempting to address the strikingly high levels of Black maternal mortality had healthcare workers undergo implicit bias training, and included a public health component through community-based organizations.[6]
A 2018 Lancet study employed a health technology system called “Gabby” to assess health risks and pre-existing conditions in Black women before conception. The study found that the use of this system to target preconception health risks increased the number of risks that received the necessary attention and treatment.[15] Addressing conditions prior to conception and prenatal care could be an important part of reducing Black maternal mortality, as Black women are more likely to have unaddressed pre-existing conditions that endanger their health or their child’s health. These conditions can impact the health of the parent or child even before conception occurs, so the use of this kind of system could be beneficial in reducing adverse outcomes.

In addition, experts in medicine, sociology, and law have said that deliberately addressing racism, both within and outside of the medical field, is necessary. Some have argued against the conventional classification of race as a risk factor in health, instead calling for the recognition of racism and poverty as the underlying factors contributing to Black maternal mortality and other poor health outcomes for Black people.[6]
Reproductive and sexual health and rights
Some of the barriers that impact access to prenatal and postnatal care also affect access to reproductive and sexual healthcare. Testing and treatment for sexually transmitted illnesses, HIV, contraception, cancer, and other health concerns impacting women is harder to access for those in low-resource settings or without health insurance. Furthermore, Black women have suffered a long history of forced sterilizations and non-consented hysterectomies.[16] Studies show that Black women have lower rates of contraception use than white women, which contributes to higher rates of unplanned pregnancies which are typically higher risk. Family planning is less accessible for low-income Black women, and beyond that, some Black women are distrustful of medical professionals and contraceptives.[17]
References
- "Maternal mortality". who.int. Retrieved 2020-10-22.
- "Racial and Ethnic Disparities Continue in Pregnancy-Related Deaths". CDC Online Newsroom. CDC. 2019-09-06. Retrieved 2020-10-22.
- Metcalfe, Amy; Wick, James; Ronksley, Paul (2018). "Racial disparities in comorbidity and severe maternal morbidity/mortality in the United States: an analysis of temporal trends". Acta Obstetricia et Gynecologica Scandinavica. 97 (1): 89–96. doi:10.1111/aogs.13245. ISSN 1600-0412. PMID 29030982. S2CID 207028740.
- "Racial Disparities Persist in Maternal Morbidity, Mortality and Infant Health". AJMC. Retrieved 2020-10-22.
- Rabin, Roni Caryn (2019-05-07). "Huge Racial Disparities Found in Deaths Linked to Pregnancy (Published 2019)". The New York Times. ISSN 0362-4331. Retrieved 2020-11-22.
- Owens, Deirdre Cooper; Fett, Sharla M. (2019-08-15). "Black Maternal and Infant Health: Historical Legacies of Slavery". American Journal of Public Health. 109 (10): 1342–1345. doi:10.2105/AJPH.2019.305243. ISSN 0090-0036. PMC 6727302. PMID 31415204.
- "The Impact of Institutional Racism on Maternal and Child Health". NICHQ - National Institute for Children's Health Quality. Retrieved 2020-10-22.
- Gadson, Alexis; Akpovi, Eloho; Mehta, Pooja K. (2017-08-01). "Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome". Seminars in Perinatology. Strategies to reduce Racial/Ethnic Disparities in Maternal Morbidity and Mortality. 41 (5): 308–317. doi:10.1053/j.semperi.2017.04.008. ISSN 0146-0005. PMID 28625554.
- Taylor, Jamila; Novoa, Cristina; Hamm, Katie; Phadke, Shilpa. "Eliminating Racial Disparities in Maternal and Infant Mortality". Center for American Progress. Retrieved 2020-10-09.
- Kozhimannil, Katy Backes; Trinacty, Connie Mah; Busch, Alisa B.; Huskamp, Haiden A.; Adams, Alyce S. (June 2011). "Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women". Psychiatric Services (Washington, D.C.). 62 (6): 619–625. doi:10.1176/appi.ps.62.6.619. ISSN 1075-2730. PMC 3733216. PMID 21632730.
- "PRIME PubMed | Syndemic Perspectives to Guide Black Maternal Health Research and Prevention During the COVID-19 Pandemic". www.unboundmedicine.com. Retrieved 2020-10-09.
- Boston, 677 Huntington Avenue; Ma 02115 +1495‑1000 (2018-12-18). "America is Failing its Black Mothers". Harvard Public Health Magazine. Retrieved 2020-10-22.
- Haddad, Lisa B; Nour, Nawal M (2009). "Unsafe Abortion: Unnecessary Maternal Mortality". Reviews in Obstetrics and Gynecology. 2 (2): 122–126. ISSN 1941-2797. PMC 2709326. PMID 19609407.
- Howell, Elizabeth A; Zeitlin, Jennifer (August 2017). "Improving Hospital Quality to Reduce Disparities in Severe Maternal Morbidity and Mortality". Seminars in Perinatology. 41 (5): 266–272. doi:10.1053/j.semperi.2017.04.002. ISSN 0146-0005. PMC 5592149. PMID 28735811.
- Jack, Brian W.; Bickmore, Timothy; Yinusa-Nyahkoon, Leanne; Reichert, Matthew; Julce, Clevanne; Sidduri, Nireesha; Martin-Howard, Jessica; Zhang, Zhe; Woodhams, Elisabeth; Fernandez, Juan; Loafman, Mark (2020-09-01). "Improving the health of young African American women in the preconception period using health information technology: a randomised controlled trial". The Lancet Digital Health. 2 (9): e475–e485. doi:10.1016/S2589-7500(20)30189-8. ISSN 2589-7500.
- Prather, Cynthia; Fuller, Taleria R.; Marshall, Khiya J.; Jeffries, William L. (July 2016). "The Impact of Racism on the Sexual and Reproductive Health of African American Women". Journal of Women's Health. 25 (7): 664–671. doi:10.1089/jwh.2015.5637. ISSN 1540-9996. PMC 4939479. PMID 27227533.
- Jackson, Andrea V.; Wang, Lin-Fan; Morse, Jessica (2017-08-01). "Racial and ethnic differences in contraception use and obstetric outcomes: A review". Seminars in Perinatology. Strategies to reduce Racial/Ethnic Disparities in Maternal Morbidity and Mortality. 41 (5): 273–277. doi:10.1053/j.semperi.2017.04.003. ISSN 0146-0005. PMID 28651792.
