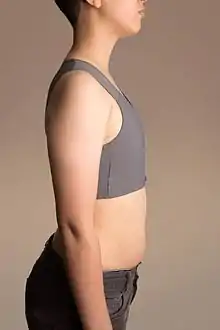
Breast binding
Breast binding is the act of flattening breasts by the use of constrictive materials. The term also refers to the material used in this act. Common binding materials include cloth strips, purpose-built undergarments (often using spandex or other synthetic fibre) and shirts layered from tight to loose. The act of breast binding is common for trans men, but is also done by androgynous and non-binary people, as well as crossdressers, cosplayers, and performers. In a general sense, women may also use binders as alternatives to bras or as a practice of propriety.[1]
Breast binding by use of cloth strip or tape may result in bodily damage such as permanent deformation of the breast if it causes injury/trauma and scarring. Fibrosis of the anterior chest wall can lead to restriction of the lung's ability to expand.
Motivation
There are many reasons people would bind their breasts:
- For accelerated recovery by reducing movement after an injury or surgery.
- For transgender people
- For cosplay, crossplay, and other forms of costuming.
- For concealment of breasts or breast development.
- For beauty and aesthetics.
- For less-feminine appearance or to assist with passing as male.
- For suppression of gender dysphoria.
- For athletics.
- Lactation suppression.[2]
Some adolescent girls bind their breasts as they enter puberty. This is done usually for reasons of modesty (they do not want others to see them), embarrassment (they do not want others to know they have started developing), or desire to be as they previously were (they do not want to have breasts yet). This has potential risks, as the developing tissue may conform to the restricted shape, resulting in permanent deformity. Breast binding in adolescent girls may be a symptom of body dysmorphic disorder.[3]
Transgender men, or people with gender dysphoria, as well as women who have developed larger breasts from hormone replacement therapy or breast augmentation surgery, may have motivation to bind their breasts. Transgender men and people with other gender identities (typically male presenting) may bind their breasts as an alternative to or while waiting for a "top surgery" (mastectomy) in order to be recognized as masculine presenting. Men may also find cause to bind if afflicted with gynecomastia as a means to control appearance in place of surgery or during the wait before surgery.
Methods
Purpose-built undergarments known as binders or binding bras exist (often using spandex or other synthetic fibre), and are commonly used for breast binding. These can be more expensive than other options and are not widely stocked, but are generally considered less dangerous than alternatives.
Other common binding materials include cloth strips, elastic or non-elastic bandages, and shirts layered from tight to loose. Duct tape has been used as well, but is dangerous and should be avoided. Elastic bandages such as ace bandages are also unsafe to use. It is safest to use a binder from a reputable company or a high impact sports bra.
Complications
To minimise complications, it is often advised that a binding device/method should always be as loose as is practicable and should not be worn for longer than 8 hours.[4] Binding for extended periods of time can lead to rashes or yeast infections under the breasts,[5][6] back or chest pain, shortness of breath, overheating, or fractured ribs.[4] Additionally, some unconventional binding materials, such as duct tape or athletic bandages, are known to increase an individual's risk for negative health outcomes such as shortness of breath, musculoskeletal damage, and skin damage.[7]
Unsafe binding may lead to permanent deformation of the breasts,[8] scarring, and lung constriction[9] and long-term binding may adversely affect the outcome of a future mastectomy.[10]
In one study, 97.2% of those surveyed had some sort of health problem caused by binding. Despite this, many are unwilling to seek medical attention due to a perceived lack of knowledge from healthcare professionals, and continue binding anyway since they believe the benefits out-weigh the risks.[4] In case of health concerns, binding wearers tend to seek help from healthcare professionals they perceive as trans-friendly and who will not stigmatize their binding practice.[11]
History
Breast binding has been used in many historical contexts. Wearing a corset was one way that the size of breasts could be reduced.[12] Different time periods of history have had differing viewpoints on the female form, including widespread use of corsets throughout western European history up to the Victorian era. The Japanese kimono can be considered a very elaborate form of binding, although the obi (belt) goes around the lower torso, while the chest is bound by the sarashi. In the 1920s, flappers bound their chests to achieve a less traditional look.[13]
See also
References
- Countryman, Betty Ann. "Breast care in the early puerperium." Journal of Obstetric, Gynecologic, & Neonatal Nursing 2.5 (1973): 36–40
- Swift, Kathy; Janke, Jill (May 2003). "Breast Binding . . . Is It All That It's Wrapped Up To Be?". J. Obstet. Gynecol. Neonatal Nurs. 32 (3): 332–339. doi:10.1177/0884217503253531. ISSN 0884-2175. PMID 12774875.
- Horowitz K, Gorfinkle K, Lewis O, Phillips KA (December 2002). "Body dysmorphic disorder in an adolescent girl". J Am Acad Child Adolesc Psychiatry. 41 (12): 1503–9. doi:10.1097/00004583-200212000-00023. PMC 1613829. PMID 12447038.
- Tsjeng, Zing (28 September 2016). "Inside the Landmark, Long Overdue Study on Chest Binding". Broadly. Retrieved 4 January 2019.
- Feldman, JL; Goldberg, J (2006). "Transgender primary medical care: Suggested guidelines for clinicians in British Columbia". Vancouver Coastal Health. Retrieved 15 June 2014.
- Erickson-Schroth, Laura (2014). Trans Bodies, Trans Selves: A Resource for the Transgender Community. Oxford University Press. p. 134. ISBN 9780199325351.
- "Chest Binding: A Physician's Guide". PRIDEinPractice. 6 April 2019. Retrieved 1 October 2020.
- "Binding FAQ" (PDF). University of Michigan Health System. Archived from the original (PDF) on 6 September 2012.
- Dutton, Lauren; Koenig, Karel; Fennie, Kristopher (2008-08-01). "Gynecologic care of the female-to-male transgender man". Journal of Midwifery & Women's Health. 53 (4): 331–337. doi:10.1016/j.jmwh.2008.02.003. ISSN 1542-2011. PMC 4902153. PMID 18586186.
- Makadon, Harvey J.; Mayer, Kenneth H.; Potter, Jennifer; Goldhammer, Hilary (2015). The Fenway Guide to Lesbian, Gay, Bisexual and Transgender Health. ACP Press. p. 409. ISBN 9781934465783.
- Jarrett, Brooke A.; Corbet, Alexandra L.; Gardner, Ivy H.; Peitzmeier, Sarah M. (14 Dec 2018). "Chest Binding and Care Seeking Among Transmasculine Adults: A Cross-Sectional Study". Transgender Health. Mary Ann Liebert, Inc., publishers. 3 (1): 170–178. doi:10.1089/trgh.2018.0017. PMC 6298447. PMID 30564633. Archived from the original on 2019-01-28.
- Smith, Merril (2014). Cultural encyclopedia of the breast. Lanham: Rowman & Littlefield. p. 46. ISBN 9780759123311.
- Farrell-Beck & Gau, J. & C. (2002). Uplift: The bra in America. Philadelphia: Philadelphia: University of Pennsylvania Press.