Cord lining
Cord lining, cord tissue, or umbilical cord lining membrane, is the outermost layer of the umbilical cord. As the umbilical cord itself is an extension of the placenta, the umbilical cord lining membrane is an extension of the amniotic membrane covering the placenta. The umbilical cord lining membrane comprises two layers: the amniotic (or epithelial) layer and the sub-amniotic (or mesenchymal) layer. The umbilical cord lining membrane is a rich source of two strains of stem cells (CLSCs): epithelial stem cells (from the amniotic layer) (CLECs) and mesenchymal stem cells (from the sub-amniotic layer) (CLMCs). Discovered by Singapore-based CellResearch Corporation in 2004, this is the best known source for harvesting human stem cells.
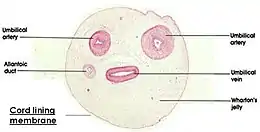
Cross-section of the umbilical cord

Source of mesenchymal stem cells
The sub-amniotic region of the umbilical cord lining has been reported to be a source of mesenchymal stem cells termed (CLMCs).[1][2] These cells express MSC specific markers such as NT5E (cluster of differentiation73), endoglin (CD105) as well as Oct 3/4 and NANOG. Furthermore, these CLMCs can also be differentiated in-vitro into osteogenic, chondrogenic and adipogenic lineages. MSC from the sub-epithelial region of the cord lining can be expanded in-vitro for more than 30 passages or 90 population doublings without losing their multi-lineage differentiation capability or going into senescence.[3]
MSC isolated from the cord lining membrane have been reported to be immune-privileged. Compared with MSC from the bone marrow, cord lining MSC showed more effective immune suppression presumably due to lower expression of HLA Class I on their surfaces and also higher expression of immune suppressive cytokines.[4] Compared with MSC from cord blood, placenta and Wharton’s Jelly, cord lining MSC showed the highest proliferation and migration potential. Furthermore, they expressed lower levels of HLA Class I and II, contributing to their lower immunogenicity.[5]
Pre-clinical studies performed on the cord lining MSC have revealed their potential in repairing heart muscle damage due to ischemia. A study performed in the rat model showed improved heart function and reduction of damaged myocardium when cord lining MSC combined with a fibrin gel carrier and a vascularized graft were introduced to the ischaemic area.[6] A similar study combining the cord lining MSC with carrier endothelial cells within a fibrin matrix in-vivo also revealed improvement in cardiac function, reduction in scar tissue formation and better vascularization.[7]
Source of epithelial stem cells
The amniotic layer of the umbilical cord lining has been shown to contain a large population of epithelial stem cells (EpSC). These cord lining EpSC exhibit classical pluripotent stem cell markers such as SSEA-4, Oct-4, SOX2 and Nanog.[8] They also express p63, a specific marker of epithelial progenitor cells.[9][10] In-vitro organotypic culture of cord lining EpSC using the air-liquid interface method resulted in stratified epithelium being formed with expression of various forms of cytokeratins.[8] Furthermore, due to their similarity in terms of phenotypic expression of keratins compared to normal human epidermal keratinocytes, cord lining EpSC have the potential to be an alternative source of cells for skin repair and regeneration.[11]
Animal studies on cord lining EpSC have shown that genetic modifications using the proinsulin gene allowed transplanted stem cells to lower blood glucose levels in diabetic animals.[12] These cells also express HLA-G in the transmembrane and soluble form, aiding in their immunosuppressive behavior. In vitro studies also indicated that cord lining EpSC can be differentiated biochemically to become hepatocyte-like cells (liver cells) as shown by the expression of hepatic-specific markers such as â-fetoprotein, albumin and hepatocyte-specific cytokeratins.[13]
Cord lining EpSC show similarities to limbal stem cells in terms of expression of ABCG2, HES1 and BMI1 in addition to p63.[10] When transplanted onto rabbit eyes with corneal defects on a human amniotic membrane scaffold, these stem cells could reconstitute the natural morphology of the corneal epithelium similar to that of a natural corneal surface.[14] The stem cells included a unique mucin-expressing cord lining epithelial stem cell (CLEC-muc) expressing (MUC1).[15] Such results were not seen when human amniotic membrane was used without the cells indicating the therapeutic value of the cord lining EpSC.
References
- Kita, K. (2008). Isolation and characterization of mesenchymal stem cells from the sub-amniotic human umbilical cord lining membrane. Stem Cells and Developments, 19(4), 491-502.
- Jeschke, M. (2011). Umbilical cord lining membrane and Wharton’s Jelly- derived mesenchymal stem cells: the similarities and differences. The Open Tissue Engineering and Regenerative Medicine Journal, 4, 21-27.
- Patel, A. N. (2013). Mesenchymal stem cell population isolated from the subepithelial layer of umbilical cord tissue. Cell Transplantation, 22, 513-519.
- Deuse, T. (2011). Immunogenicity and immunomodulatory properties of umbilical cord lining mesenchymal cells. Cell Transplantation, 20, 655-667.
- Stubbendorff, M. (2013). Immunological properties of extraembryonic human mesenchymal stromal cells derived from gestational tissue. Stem Cells and Development, 22(19), 1-9.
- Lilyanna, S. (2013). Cord lining-mesenchymal stem cells graft supplemented with an omental flap induces myocardial revascularization and ameliorates cardiac dysfunction in a rat model of chronic ischemic heart failure. Tissue Engineering Part A, 19(11-12), 1303-1315.
- Martinez, E. (2013). Grafts enriched with subamnion-cord-lining mesenchymal stem cell angiogenic spheroids induce post-ischemic myocardial revascularization and preserve cardiac function in failing rat hearts. Stem Cells and Developments, 22(23), 3087-3099.
- Huang, L. (2011). Stem cell-like properties of human umbilical cord lining epithelial cells and the potential for epidermal reconstitution. Cytotherapy, 13(2), 145-155.
- Pellegrini, G. (2001). p63 identifies keratinocyte stem cells. PNAS, 98(6), 3156-3161.
- Reza, H. M. (2011). Characterization of a novel umbilical cord lining cell with CD227 positivity and unique pattern of P63 expression and function. Stem Cells Reviews and Reports, 7(3), 624-638.
- Ruetze, M. (2008). Common features of umbilical cord epithelial cells and epidermal keratinocytes. Journal of Dermatological Science, 50(3), 227-231.
- Zhou, Y. (2011). Characterization of human umbilical cord lining-derived epithelial cells and transplantation potential. Cell transplantation, 20, 1827-1841.
- Cheong, H. H. (2013). Metabolically functional hepatocyte-like cells from human umbilical cord lining epithelial cells. Assay Drug Development and Technologies, 11(2), 130-138.
- Bains, KK; et al. (August 2019). "Recovering vision in corneal epithelial stem cell deficient eyes". Contact Lens & Anterior Eye: The Journal of the British Contact Lens Association. 42 (4): 350–358. doi:10.1016/j.clae.2019.04.006. PMC 6611221. PMID 31047800.
- Saleh, R; Reza, HM (10 October 2017). "Short review on human umbilical cord lining epithelial cells and their potential clinical applications". Stem Cell Research & Therapy. 8 (1): 222. doi:10.1186/s13287-017-0679-y. PMC 5634865. PMID 29017529.
