Ethyl eicosapentaenoic acid
Ethyl eicosapentaenoic acid (E-EPA, icosapent ethyl) is a medication used to treat hypertriglyceridemia. It is used in combination with changes in diet in adults with hypertriglyceridemia ≥ 150 mg/dL.[2]
 | |
| Clinical data | |
|---|---|
| Trade names | Vascepa |
| Other names | Eicosapentaenoic acid ethyl ester; Ethyl eicosapentaenoate; Eicosapent; EPA ethyl ester; E-EPA, Icosapent ethyl (USAN US) |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a613024 |
| License data |
|
| Routes of administration | By mouth |
| Drug class | Antilipemic Agents |
| ATC code |
|
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C22H34O2 |
| Molar mass | 330.512 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
It is made from the omega-3 fatty acid eicosapentaenoic acid (EPA).[2] The US Food and Drug Administration (FDA) granted the approval of it (as Vascepa) in 2012, to Amarin Corporation, and it became the second fish oil-based medication after omega-3 acid ethyl esters, brand named Lovaza, which was approved in 2004.[3] On 13 December 2019, FDA also approved it as the first drug specifically "to reduce cardiovascular risk among patients with elevated triglyceride levels".[2]
The most common side effects are musculoskeletal pain, peripheral edema (swelling of legs and hands), atrial fibrillation, and arthralgia (joint pain).[2]
It is has been approved by the FDA as a generic medication.[4] However due to ongoing patent litigation, the generic companies have not brought the generic version to market. Oral arguments are scheduled in the Court of Appeals for the Federal Circuit for September 3, 2020, at 10:00 am.
Medical use
Ethyl eicosapentaenoic acid (E-EPA) is used in addition to changes in diet to reduce triglyceride levels in adults with severe (≥ 500 mg/dL) hypertriglyceridemia.[1] Or it may be used in hypertriglyceridemia ≥ 150 mg/dL in those with risk factors for heart disease.[2]
Intake of large doses (2.0 to 4.0 g/day) of long-chain omega-3 fatty acids as prescription drugs or dietary supplements are generally required to achieve significant (> 15%) lowering of triglycerides, and at those doses the effects can be significant (from 20% to 35% and even up to 45% in individuals with levels greater that 500 mg/dL). It appears that both eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) lower triglycerides, however, DHA alone appears to raise low-density lipoprotein (the variant which drives atherosclerosis; sometimes very inaccurately called: "bad cholesterol") and LDL-C values (always only a calculated estimate; not measured by labs from person's blood sample for technical and cost reasons), whilst eicosapentaenoic acid (EPA) alone does not and instead lowers the parameters aforementioned.[5]
Other fish-oil based drugs
There are other omega-3 fish-oil based drugs on the market that have similar uses and mechanisms of action:[6][3][7]
- Omega-3 acid ethyl esters (brand names Omarcor, Lovaza, and Omtryg)[8][9] and, as of March 2016, four generic versions;[10][11]
- Omega-3 carboxylic acids (Epanova);[12][13] the Epanova brand name was discontinued in the United States.[14]
Dietary supplements
There are many fish oil dietary supplements on the market.[3] Evidence does not support a beneficial role for n-3 dietary supplements to reduce cardiovascular disease as an addition to contemporary medical therapy including statin therapy.[15][16][17] The ingredients of dietary supplements are not as carefully controlled as prescription products and have not been fixed and tested in clinical trials, as prescription drugs have,[18] and the prescription forms are more concentrated, requiring fewer capsules to be taken and increasing the likelihood of compliance.[3]
Side effects
Special caution should be taken with people who have fish and shellfish allergies.[1] In addition, as with other omega-3 fatty acids, taking ethyl eicosapentaenoic acid (E-EPA) puts people who are on anticoagulants at risk for prolonged bleeding time.[1][5] The most commonly reported side effect in clinical trials has been joint pain; some people also reported pain in their mouth or throat.[1] E-EPA has not been tested in pregnant women;[19] it is excreted in breast milk and the effects on infants are not known.[1]
Pharmacology
After ingestion, ethyl eicosapentaenoic acid (E-EPA) is metabolized to eicosapentaenoic acid (EPA). EPA is absorbed in the small intestine and enters circulation. Peak plasma concentration occurs about 5 hours after ingestion and the half-life is about 89 hours. EPA is metabolized mostly in the liver like other dietary fatty acids.[1]
Mechanism of action
Eicosapentaenoic acid (EPA), the active metabolite of ethyl eicosapentaenoic acid (E-EPA), like other omega-3 fatty acid based drugs, appears to reduce production of triglycerides in the liver, and to enhance clearance of triglycerides from circulating very low-density lipoprotein (VLDL) particles; the way it does that is not clear, but potential mechanisms include increased breakdown of fatty acids; inhibition of diglyceride acyltransferase which is involved in biosynthesis of triglycerides in the liver; and increased activity of lipoprotein lipase in blood.[1][6]
Chemistry
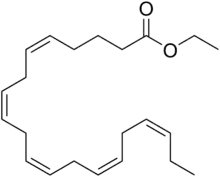
Ethyl eicosapentaenoic acid (E-EPA) is an ethyl ester of eicosapentaenoic acid, which is an omega-3 fatty acid.[1]
History
In July 2012, the US Food and Drug Administration (FDA) approved ethyl eicosapentaenoic acid (E-EPA) for severe hypertriglyceridemia as an adjunct to dietary measures;[20] Amarin Corporation had developed the drug.[21] Amarin Corporation, challenged the FDA's authority to limit its ability to market the drug for off-label use and won its case on appeal in 2012, changing the way the FDA regulates the marketing of medication.
Ethyl eicosapentaenoic acid (E-EPA) was the second fish-oil drug to be approved, after omega-3 acid ethyl esters (GlaxoSmithKline's Lovaza which was approved in 2004[22][3][23]) and sales were not as robust as Amarin had hoped. The labels for the two drugs were similar, but doctors prescribed Lovaza for people who had triglycerides lower than 500 mg/dL based on some clinical evidence. Amarin wanted to actively market E-EPA for that population as well which would have greatly expanded its revenue, and applied to the FDA for permission to do so in 2013, which the FDA denied.[24] In response, in May 2015 Amarin sued the FDA for infringing its First Amendment rights,[25] and in August 2015, a judge ruled that the FDA could not "prohibit the truthful promotion of a drug for unapproved uses because doing so would violate the protection of free speech."[26] The ruling left open the question of what the FDA would allow Amarin to say about E-EPA, and in March 2016 the FDA and Amarin agreed that Amarin would submit specific marketing material to the FDA for the FDA to review, and if the parties disagreed on whether the material was truthful, they would seek a judge to mediate.[27]
In December 2019, the FDA approved the use of icosapent ethyl as an adjunctive (secondary) therapy to reduce the risk of cardiovascular events among adults with elevated triglyceride levels (a type of fat in the blood) of 150 milligrams per deciliter or higher.[2] Patients must also have either established cardiovascular disease or diabetes and two or more additional risk factors for cardiovascular disease.[2]
Icosapent ethyl is the first FDA approved drug to reduce cardiovascular risk among patients with elevated triglyceride levels as an add-on to maximally tolerated statin therapy.[2]
The efficacy and safety of icosapent ethyl were established in a study with 8,179 patients who were either 45 years and older with a documented history of coronary artery, cerebrovascular, carotid artery and peripheral artery disease, or 50 years and older with diabetes and additional risk factors for cardiovascular disease.[2] Patients who received icosapent ethyl were significantly less likely to experience a cardiovascular event, such as a stroke or heart attack.[2]
In clinical trials, icosapent ethyl was associated with an increased risk of atrial fibrillation or atrial flutter (irregular heart rhythms) requiring hospitalization.[2] The incidence of atrial fibrillation was greater among patients with a history of atrial fibrillation or atrial flutter.[2] Icosapent ethyl was also associated with an increased risk of bleeding events.[2] The incidence of bleeding was higher among patients who were also taking other medications that increase the risk of bleeding, such as aspirin, clopidogrel or warfarin at the same time.[2]
Society and culture
Legal status
On 28 January 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) adopted a positive opinion, recommending the granting of a marketing authorization for the medicinal product Vazkepa, intended to reduce the risk of cardiovascular events in patients at high cardiovascular risk.[28] The applicant for this medicinal product is Amarin Pharmaceuticals Ireland Limited.[28]
References
- "Vascepa- icosapent ethyl capsule". DailyMed. 23 December 2019. Retrieved 15 January 2020.
- "FDA approves use of drug to reduce risk of cardiovascular events in certain adult patient groups". U.S. Food and Drug Administration (FDA) (Press release). 13 December 2019. Archived from the original on 22 December 2019. Retrieved 21 December 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Ito MK (December 2015). "A Comparative Overview of Prescription Omega-3 Fatty Acid Products". P T. 40 (12): 826–57. PMC 4671468. PMID 26681905.
- "Icosapent ethyl: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 15 August 2020.
- Jacobson TA, Maki KC, Orringer CE, Jones PH, Kris-Etherton P, Sikand G, et al. (2015). "National Lipid Association Recommendations for Patient-Centered Management of Dyslipidemia: Part 2". Journal of Clinical Lipidology. 9 (6 Suppl): S1–122.e1. doi:10.1016/j.jacl.2015.09.002. PMID 26699442.
- Weintraub HS (November 2014). "Overview of prescription omega-3 fatty acid products for hypertriglyceridemia". Postgraduate Medicine. 126 (7): 7–18. doi:10.3810/pgm.2014.11.2828. PMID 25387209.
- Brinton EA, Mason RP (January 2017). "Prescription omega-3 fatty acid products containing highly purified eicosapentaenoic acid (EPA)". Lipids Health Dis. 16 (1): 23. doi:10.1186/s12944-017-0415-8. PMC 5282870. PMID 28137294.
- "University of Utah Pharmacy Services (15 August 2007) "Omega-3-acid Ethyl Esters Brand Name Changed from Omacor to Lovaza"". Archived from the original on 3 March 2016. Retrieved 1 April 2016.
- "Omtryg- omega-3-acid ethyl esters capsule". DailyMed. 31 March 2016. Retrieved 15 January 2020.
- FDA Omega-3 acid ethyl esters products Page accessed 31 March 2016
- "Omega-3-acid ethyl esters". DailyMed. Retrieved 2 February 2020.
- "Epanova (omega-3-carboxylic acids)". CenterWatch. Retrieved 15 December 2014.
- "Drug Approval Package: Epanova (Omega-3-carboxylic acids)". U.S. Food and Drug Administration (FDA). 28 March 2016. Retrieved 15 January 2020.
- "Epanova (omega-3-carboxylic acids) FDA Approval History". Drugs.com. 5 May 2014. Retrieved 15 January 2020.
- American Diabetes Association (20 December 2019). "Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2020". Diabetes Care. American Diabetes Association. 43 (Supplement 1): S53. doi:10.2337/dc20-S005. ISSN 1935-5548. PMID 31862748.
- Jellinger, Paul S.; Handelsman, Yehuda; Rosenblit, Paul D.; Bloomgarden, Zachary T.; Fonseca, Vivian A.; Garber, Alan J.; Grunberger, George; Guerin, Chris K.; Bell, David S. H.; Mechanick, Jeffrey I.; Pessah-Pollack, Rachel; Wyne, Kathleen; Smith, Donald; Brinton, Eliot A.; Fazio, Sergio; Davidson, Michael (13 June 2019). "AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY GUIDELINES FOR MANAGEMENT OF DYSLIPIDEMIA AND PREVENTION OF CARDIOVASCULAR DISEASE". Endocrine Practice. AACECOR. 23 (Supplement 2): 14. doi:10.4158/EP171764.APPGL. ISSN 1934-2403. PMID 28437620.
- Skulas-Ray, Ann C.; Wilson, Peter W.F.; Harris, William S.; Brinton, Eliot A.; Kris-Etherton, Penny M.; Richter, Chesney K.; Jacobson, Terry A.; Engler, Mary B.; Miller, Michael; Robinson, Jennifer G.; Blum, Conrad B.; Rodriguez-Leyva, Delfin; de Ferranti, Sarah D.; Welty, Francine K. (17 September 2019). "Omega-3 Fatty Acids for the Management of Hypertriglyceridemia: A Science Advisory From the American Heart Association". Circulation. Lippincott Williams & Wilkins. 140 (12): e687. doi:10.1161/CIR.0000000000000709. ISSN 1524-4539. PMID 31422671.
- Sweeney ME (14 April 2015). Khardori R (ed.). "Hypertriglyceridemia Pharmacologic Therapy". Medscape Drugs & Diseases. Retrieved 1 April 2016.
- "Icosapent (Vascepa) Use During Pregnancy". Drugs.com. 18 February 2019. Retrieved 15 January 2020.
- "Drug Approval Package: Vascepa (icosapent ethyl) NDA #202057". U.S. Food and Drug Administration (FDA). 6 March 2013. Retrieved 15 January 2020.
- CenterWatch Vascepa (icosapent ethyl) Page accessed 31 March 2016
- "Drug Approval Package: Omacor (Omega-3-Acid Ethyl Esters) NDA #021654". U.S. Food and Drug Administration (FDA). 24 December 1999. Retrieved 15 January 2020.
- VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel. October 2005 National PBM Drug Monograph Omega-3-acid ethyl esters (Lovaza, formerly Omacor)
- Herper M (17 October 2013). "Why The FDA Is Right To Block Amarin's Push To Market Fish Oil To Millions". Forbes.
- Thomas K (7 May 2015). "Drugmaker Sues F.D.A. Over Right to Discuss Off-Label Uses". The New York Times. Retrieved 17 May 2017.
- Pollack A (7 August 2015). "Court Forbids F.D.A. From Blocking Truthful Promotion of Drug". The New York Times. Retrieved 21 December 2019.
- Thomas K (9 March 2016). "F.D.A. Deal Allows Amarin to Promote Drug for Off-Label Use". The New York Times. Retrieved 21 December 2019.
- "Vazkepa: Pending EC decision". European Medicines Agency (EMA). 29 January 2021. Retrieved 1 February 2021.
External links
- "Icosapent ethyl". Drug Information Portal. U.S. National Library of Medicine.
