Functional endoscopic sinus surgery
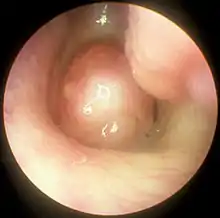
Functional endoscopic sinus surgery (FESS) is a minimally invasive surgical treatment which uses nasal endoscopes to enlarge the nasal drainage pathways of the paranasal sinuses to improve sinus ventilation and allow access of topical medications.[1][2] This procedure is generally used to treat inflammatory and infectious sinus diseases, including chronic rhinosinusitis that doesn't respond to drugs,[3][4] nasal polyps,[5][3] some cancers,[6] and decompression of eye sockets/optic nerve in Graves ophthalmopathy.[1]
| Functional endoscopic sinus surgery | |
|---|---|
 Otolaryngologist performing Functional Endoscopic Sinus Surgery. An endoscopic view of the nasal cavity is displayed in real-time on the monitor. | |
| Specialty | Otolaryngology |
In the surgery, an otolaryngologist removes the uncinate process of the ethmoid bone, while visualizing the nasal passage using a fiberoptic endoscope.[1] FESS can be performed under local anesthesia as an outpatient procedure.[5] Generally patients experience only minimal discomfort during and after surgery. The procedure can take from 2 to 4 hours to complete.[2]
History
The first recorded instance of endoscopy being used for visualization of the nasal passage was in Berlin, Germany in 1901.[7] Alfred Hirschmann, who designed and made medical instruments, modified a cystoscope to be used in the nasal cavity. In October 1903, Hirschmann published "Endoscopy of the nose and its accessory sinuses."[8] In 1910, M. Reichart performed the first endoscopic sinus surgery using a 7 mm endoscope. In 1925, Maxwell Maltz, MD created the term "sinuscopy," referring to the endoscopic method of visualizing the sinuses. Maltz also encouraged the use of endoscopes as a diagnostic tool for nasal and sinus abnormalities.[7]
In the 1960s, Harold Hopkins, PhD at Reading University used his background in physics to develop an endoscope that provided more light and had drastically better resolution than previous endoscopes. Hopkins' rod optic system is widely credited with being a turning point for nasal endoscopy.[7] Utilizing Hopkins' rod optic system, Austrian doctor Walter Messenklinger visualized and recorded the anatomy of the paranasal sinuses and the lateral nasal walls in cadavers. Specifically, Messerklinger focused on mapping out mucociliary routes.[9] In 1978, Messerklinger published the book titled "Endoscopy of the Nose" on his findings, and his proposed methods to utilize nasal endoscopy for diagnosis.[10]
After learning of Messenklinger's endoscopic techniques, David Kennedy, MD, of Johns Hopkins University worked with the surgical instrument maker, Karl Storz to develop instruments for use in endoscopic sinus surgery, and coined the term Functional Endoscopic Sinus Surgery.[9] Kennedy published multiple papers on FESS use and technique, and in 1985 the first course on FESS was taught at Johns Hopkins Medical Center.[7] Kennedy and Heinz Stammberger, a junior associate of Messerklinger, refined the techniques and provided hands-on teaching courses on the techniques throughout the World.
Medical applications
Functional Endoscopic Sinus Surgery is most commonly used to treat chronic rhinosinusitis,[1] only after all non-surgical treatment options such as antibiotics, topical nasal corticosteroids, and nasal lavage with saline solutions[3] have been exhausted. Chronic rhinosinusitis (CRS) is an inflammatory condition in which the nose and at least one sinus become swollen and interfere with mucus drainage.[3] It can be caused by anatomical factors such as a deviated septum or nasal polyps (growths), as well as infection. Symptoms include difficulty breathing through the nose, swelling and pain around the nose and eyes, postnasal drainage down the throat, and difficulty sleeping.[11] CRS is a common condition in pediatric patients and young adults.[12]
The purpose of FESS in treatment of CRS is to remove any anatomical obstructions that prevent proper mucosal drainage. A standard FESS includes removal of the uncinate process, and opening of the ethmoid air cells and Haller cells[13] as well as the maxillary ostium, if necessary. If any nasal polyps obstructing ventilation or drainage are present, they are also removed.[1] In the case of paranasal sinus/nasal cavity tumors (benign or cancerous), an otolaryngologist can perform FESS to remove the growths, sometimes with the help of a neurosurgeon, depending on the extent of the tumor. In some cases, a graft of bone or skin is placed by FESS to repair damages by the tumor.[14]
In the thyroid disorder known as Graves Ophthalmopathy, inflammation and fat accumulation in the orbitonasal region cause severe proptosis.[15] In cases that have not responded to corticosteroid treatment, FESS can be used to decompress the orbital region by removing the ethmoid air cells and lamina papyracea. Bones of the orbital cavity or portions of the orbital floor may also be removed.[7]
The endoscopic approach to FESS is a less invasive method than open sinus surgery, which allows patients to be more comfortable during and after the procedure. Entering the surgical field via the nose, rather than through an incision in the mouth as in the previous Caldwell-Luc method, decreases risk of damaging nerves which innervate the teeth.[1] Because of its less-invasive nature, FESS is a common option for children with CRS or other sinonasal complications.
Outcomes and complications
Functional Endoscopic Sinus Surgery is considered a success if most of the symptoms, including nasal obstruction, sleep quality, olfaction and facial pain, are resolved after a 1-2 month postoperative healing period.[1][16][4] Reviews of FESS as a method for treating chronic rhinosinusitis have shown that a majority of patients report increased quality of life after undergoing surgery.[17][16] The success rate of FESS in treating adults with CRS has been reported as 80-90%,[18] and the success rate in treating children with CRS has been reported as 86-97%.[12] The most common complication of FESS is cerebrospinal fluid leak (CSFL), which has been observed in about 0.2% of patients. Generally, CSFL arises during surgery and can be repaired with no additional related complications postoperatively. Other risks of surgery include infection, bleeding, double vision usually lasting a few hours, numbness of the front teeth, orbital hematoma, decreased sense of smell, and blindness.[2][19] Blindness is the single most serious complication of FESS, and results from damage to the optic nerve during surgery. Serious complications such as blindness occur in only 0.44% of cases, as determined by a study performed in the United Kingdom.[1] A Cochrane review in 2006 based on three randomized control trials concluded that FESS has not been shown to provide significantly better results than medical treatment for chronic rhinosinusitis.[20] Another Cochrane review looked at postoperative care of patients after FESS using debridement (removal of blood clots, crusts, and secretions from the nasal and sinus cavities under local anaesthetic), but the evidence from the available clinical trials was uncertain. The debridement procedure after FESS may make little or no difference to health‐related quality of life or disease severity. There may be a lower risk of adhesions but whether this has any impact on long‐term outcomes is unknown.[21]
References
- Slack R, Bates G (September 1998). "Functional endoscopic sinus surgery". American Family Physician. 58 (3): 707–18. PMID 9750539.
- "Functional Endoscopic Sinus Surgery". UNC Otolaryngology/Head and Neck Surgery. Retrieved 2018-06-09.
- Cazzavillan A, Castelnuovo P, Berlucchi M, Baiardini I, Franzetti A, Nicolai P, Gallo S, Passalacqua G (August 2012). "Management of chronic rhinosinusitis". Pediatric Allergy and Immunology. 23 Suppl 22: 32–44. doi:10.1111/j.1399-3038.2012.01322.x. PMID 22762852.
- Sukato DC, Abramowitz JM, Boruk M, Goldstein NA, Rosenfeld RM (February 2018). "Endoscopic Sinus Surgery Improves Sleep Quality in Chronic Rhinosinusitis: A Systematic Review and Meta-analysis". Otolaryngology–Head and Neck Surgery. 158 (2): 249–256. doi:10.1177/0194599817737977. PMID 29065273.
- Patel A (2 March 2016). "Functional Endoscopic Sinus Surgery: Overview, Preparation, Technique". eMedicine. Cite journal requires
|journal=(help) - Meccariello G, Deganello A, Choussy O, Gallo O, Vitali D, De Raucourt D, Georgalas C (April 2016). "Endoscopic nasal versus open approach for the management of sinonasal adenocarcinoma: A pooled-analysis of 1826 patients" (PDF). Head & Neck. 38 Suppl 1 (S1): E2267-74. doi:10.1002/hed.24182. hdl:11379/493402. PMID 26335008.
- Tajudeen BA, Kennedy DW (June 2017). "Thirty years of endoscopic sinus surgery: What have we learned?". World Journal of Otorhinolaryngology - Head and Neck Surgery. 3 (2): 115–121. doi:10.1016/j.wjorl.2016.12.001. PMC 5683659. PMID 29204590.
- Hirschmann A (October 1903). "Endoscopy of the nose and its accessory sinuses". The Laryngoscope. 13 (10): 810. doi:10.1288/00005537-190310000-00015.
- Kane KJ (2018-01-17). "The early history and development of endoscopic sinonasal surgery in Australia: 1985–2005". Australian Journal of Otolaryngology. 1 (1): 7. doi:10.21037/ajo.2018.01.08.
- Walter M (1978). Endoscopy of the nose. Baltimore: Urban & Schwarzenberg. ISBN 0806712112. OCLC 3447558.
- "Chronic sinusitis - Symptoms and causes". Mayo Clinic. Retrieved 2018-06-09.
- Makary CA, Ramadan HH (June 2013). "The role of sinus surgery in children". The Laryngoscope. 123 (6): 1348–52. doi:10.1002/lary.23961. PMID 23361382.
- Levine CG, Casiano RR (February 2017). "Revision Functional Endoscopic Sinus Surgery". Otolaryngologic Clinics of North America. 50 (1): 143–164. doi:10.1016/j.otc.2016.08.012. PMID 27888911.
- "Treatment of Sinus Tumors". care.american-rhinologic.org. Retrieved 2018-06-09.
- Cury SS, Oliveira M, Síbio MT, Clara S, Luvizotto RA, Conde S, Jorge EN, Nunes VD, Nogueira CR, Mazeto GM (May 2018). "Graves' ophthalmopathy: low-dose dexamethasone reduces retinoic acid receptor-alpha gene expression in orbital fibroblasts". Archives of Endocrinology and Metabolism. 62 (AHEAD): 366–369. doi:10.20945/2359-3997000000044. PMID 29791662.
- Prasad S, Fong E, Ooi EH (July 2017). "Systematic review of patient-reported outcomes after revision endoscopic sinus surgery". American Journal of Rhinology & Allergy. 31 (4): 248–255. doi:10.2500/ajra.2017.31.4446. PMID 28716176.
- Soler ZM, Jones R, Le P, Rudmik L, Mattos JL, Nguyen SA, Schlosser RJ (March 2018). "Sino-Nasal outcome test-22 outcomes after sinus surgery: A systematic review and meta-analysis". The Laryngoscope. 128 (3): 581–592. doi:10.1002/lary.27008. PMC 5814358. PMID 29164622.
- Stammberger H, Posawetz W (1990). "Functional endoscopic sinus surgery. Concept, indications and results of the Messerklinger technique". European Archives of Oto-Rhino-Laryngology. 247 (2): 63–76. doi:10.1007/bf00183169. PMID 2180446.
- "Functional Endoscopic Sinus Surgery - Otorhinolaryngology - Head & Neck Surgery". Otorhinolaryngology - Head & Neck Surgery. McGovern Medical School. 2012-09-07. Retrieved 2018-06-11.
- Khalil HS, Nunez DA (July 2006). "Functional endoscopic sinus surgery for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews (3): CD004458. doi:10.1002/14651858.cd004458.pub2. PMID 16856048.
- Tzelnick S, Alkan U, Leshno M, Hwang P, Soudry E, et al. (Cochrane ENT Group) (November 2018). "Sinonasal debridement versus no debridement for the postoperative care of patients undergoing endoscopic sinus surgery". The Cochrane Database of Systematic Reviews. 11: CD011988. doi:10.1002/14651858.CD011988.pub2. PMC 6517168. PMID 30407624.