Otorhinolaryngology
Otorhinolaryngology (/oʊtoʊˌraɪnoʊˌlærənˈɡɒlədʒi/ oh-toh-RYE-noh-LAR-ən-GOL-ə-jee; abbreviated ORL; also called otolaryngology; other terms include otolaryngology – head and neck surgery (ORL–H&N, OHNS) and ear, nose, and throat, often called ENT) is a surgical subspecialty within medicine that deals with the surgical and medical management of conditions of the head and neck. Doctors who specialize in this area are called otorhinolaryngologists, otolaryngologists, head and neck surgeons, or ENT surgeons or physicians. Patients seek treatment from an otorhinolaryngologist for diseases of the ear, nose, throat, base of the skull, head, and neck. These commonly include functional diseases that affect the senses and activities of eating, drinking, speaking, breathing, swallowing, and hearing. In addition, ENT surgery encompasses the surgical management and reconstruction of cancers and benign tumors of the head and neck as well as plastic surgery of the face and neck.
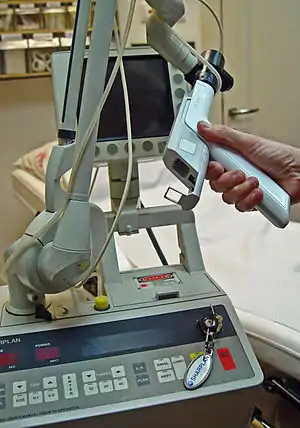
 Otolaryngologist performing an endoscopic sinus surgical procedure | |
| Significant diseases | Dizziness Head and neck cancer Sinusitis |
|---|---|
| Specialist | Otorhinolaryngologist |
| Glossary | Glossary of medicine |
| Occupation | |
|---|---|
| Names |
|
Occupation type | Specialty |
Activity sectors | Medicine, Surgery |
| Description | |
Education required |
|
Fields of employment | Hospitals, Clinics |

Etymology
The term is a combination of New Latin combining forms (oto- + rhino- + laryngo- + -logy) derived from four Ancient Greek words: οὖς ous (gen.: ὠτός otos), "ear", ῥίς rhis, "nose", λάρυγξ larynx, "larynx" and -λογία logia, "study"[1] (cf. Greek ωτορινολαρυγγολόγος, "otorhinolaryngologist").
Training
Otorhinolaryngologists are physicians (MD, DO, MBBS, MBChB, etc.) who complete medical school and then 5–7 years of post-graduate surgical training in ORL-H&N. In the United States, trainees complete at least five years of surgical residency training.[2] This comprises three to six months of general surgical training and four and a half years in ORL-H&N specialist surgery. In Canada and the United States, practitioners complete a five-year residency training after medical school.
Following residency training, some otolaryngologist-head & neck surgeons complete an advanced sub-specialty fellowship, where training can be one to two years in duration. Fellowships include head and neck surgical oncology, facial plastic surgery, rhinology and sinus surgery, neuro-otology, pediatric otolaryngology, and laryngology. In the United States and Canada, otorhinolaryngology is one of the most competitive specialties in medicine in which to obtain a residency position following medical school.[3][4]
In the United Kingdom entrance to otorhinolaryngology higher surgical training is highly competitive and involves a rigorous national selection process.[5] The training programme consists of 6 years of higher surgical training after which trainees frequently undertake fellowships in a sub-speciality prior to becoming a consultant.
The typical total length of education and training, post-secondary school is 12–14 years. Otolaryngology is among the more highly compensated surgical specialties in the United States ($461,000 2019 Average Annual Income).[6]
Sub-specialties
| Head and Neck Oncologic Surgery | Facial plastic and reconstructive surgery* | Otology | Neurotology* | Rhinology/Sinus/Anterior Skull Base Surgery | Laryngology and Voice Disorders | Pediatric Otorhinolaryngology* | Sleep Medicine* |
| Surgical oncology | Facial cosmetic surgery | Ear | Middle and inner ear | Sinusitis | Voice disorders | Velopalatine insufficiency | Sleep disorders |
| Microvascular
reconstruction |
Maxillofacial surgery | Hearing | Temporal bone | Allergy | Phono-surgery | Cleft lip and palate | Sleep apnea surgery |
| Endocrine surgery | Traumatic reconstruction | Balance | Skull base surgery | Anterior skull base | Swallowing disorders | Airway | Sleep investigations |
| Endoscopic Surgery | Craniofacial surgery | Dizziness | Apnea and snoring | Vascular malformations | |||
| Cochlear implant/BAHA | Cochlear implant/BAHA |
(* Currently recognized by American Board of Medical Subspecialties)
Topics by Subspecialty
Head and Neck Surgery
- Head and Neck Surgical Oncology (field of surgery treating cancer/malignancy of the head and neck)
- Head and neck mucosal malignancy (cancer of the pink lining of the upper aerodigestive tract
- Oral cancer (cancer of lips, gums, tongue, hard palate, cheek, floor of mouth)
- Oropharyngeal cancer (cancer of oropharynx, soft palate, tonsil, base of tongue)
- Larynx cancer (voicebox cancer)
- Hypopharynx cancer (lower throat cancer)
- Sinonasal cancer
- Nasopharyngeal cancer
- Skin cancer of the head & neck
- Thyroid cancer
- Salivary gland cancer
- Head and neck sarcoma
- Head and neck mucosal malignancy (cancer of the pink lining of the upper aerodigestive tract
- Endocrine surgery of the head and neck
- Thyroid surgery
- Parathyroid surgery
- Microvascular free flap reconstructive surgery
- Skull base surgery
Otology and Neurotology
Study of diseases of the outer ear, middle ear and mastoid, and inner ear, and surrounding structures (such as the facial nerve and lateral skull base)
- Outer ear diseases
- Middle ear and mastoid diseases
- Otitis media – middle ear inflammation
- Perforated eardrum (hole in the eardrum due to infection, trauma, explosion or loud noise)
- Mastoiditis
- Inner ear diseases
- BPPV – benign paroxysmal positional vertigo
- Labyrinthitis/Vestibular neuronitis
- Ménière's disease/Endolymphatic hydrops
- Perilymphatic fistula
- Acoustic neuroma, vestibular schwannoma
- Facial nerve disease
- Idiopathic facial palsy (Bell's Palsy)
- Facial nerve tumors
- Ramsay Hunt Syndrome
- Symptoms
- Hearing loss
- Tinnitus (subjective noise in the ear)
- Aural fullness (sense of fullness in the ear)
- Otalgia (pain referring to the ear)
- Otorrhea (fluid draining from the ear
- Vertigo
- Imbalance
Rhinology
Rhinology includes nasal dysfunction and sinus diseases.
- Nasal obstruction
- Nasal septum deviation
- Sinusitis – acute, chronic
- Environmental allergies
- Rhinitis
- Pituitary tumor
- Empty nose syndrome
- Severe or recurrent epistaxis
Pediatric Otorhinolaryngology
- Adenoidectomy
- Caustic ingestion
- Cricotracheal resection
- Decannulation
- Laryngomalacia
- Laryngotracheal reconstruction
- Myringotomy and tubes
- Obstructive sleep apnea – pediatric
- Tonsillectomy
Laryngology
- Dysphonia/hoarseness
- Spasmodic dysphonia
- Tracheostomy
- Cancer of the larynx
- Vocology – science and practice of voice habilitation
Facial Plastic and Reconstructive Surgery
Facial Plastic and Reconstructive Surgery is a one-year fellowship open to otorhinolaryngologists and plastic surgeons who wish to specialize in the aesthetic and reconstructive surgery of the head, face, and neck.
- Rhinoplasty and septoplasty
- Facelift (rhytidectomy)
- Browlift
- Blepharoplasty
- Otoplasty
- Genioplasty
- Injectable cosmetic treatments
- Trauma to the face
- Nasal bone fracture
- Mandible fracture
- Orbital fracture
- Frontal sinus fracture
- Complex lacerations and soft tissue damage
- Skin cancer (e.g. Basal Cell Carcinoma)
Free Muscle Transfer
In this type of surgery, a surgeon harvests a muscle from the back or from the abdominal region for reconstruction of the skull or the cranial vault. Latissimus is another word for back in the medical field as well as rectus abdominis which is your abdominal area. The muscle is sometimes useful for sealing off the central nervous system in one's body and allowing it to heal the complex wounds. A study was done with five patients who underwent the free muscle transfer for a smile reconstruction. Two of the five patients prior to this surgery had failed their first free muscle transfer. The next two patients had vascular anomalies and one had a previous distal ligation of the facial vessels. In three of the cases, they used a submental vein, and in all the cases they used a donor submental artery. "In all 5 the gracilis vascular pedicle comprised a muscular branch of the profunda femoris together with its venae comitantes, with the artery and vein ranging in size from 1.0 to 1.5 mm and 2.0 to 2.5 mm, respectively. The submental artery provided an excellent size match in all cases, ranging in size from 1.0 to 1.5 mm"(Faltaous AA, Yetman RJ).[7] The first patient was a 45-year-old woman who developed a dense flaccid right facial paralysis at the age of 33. The second patient was an 8-year-old girl who had developed dense flaccid left facial paralysis after a laser treatment at four weeks for, "bilateral infantile segmental hemangiomas in the distribution of the mandibular division of the trigeminal nerve (V3). "(volume 38, issue 10). The third case was a 19-year-old male who had developed a segmental right facial paralysis after an excision of an infantile parotid hemangioma at the age of 2. The fourth case was a 20-year-old woman who had developed dense flaccid right facial paralysis after a biopsy of a pontomedullary junction tumor at the age of 2. Lastly, case five was a 19-year-old woman who had incomplete flaccid left facial palsy.
Free Bone Transfer
Bone defects are often the most difficult reconstructions as it requires precise alignment. Bone transfer is commonly used for the mandibular reconstruction, but it now allows surgeons to use it for the midface and the orbito maxillary. If for some reason the fibula is not available for transfer, another option the team may go is using the back rib free flap. This allows the transfer to give the bone volume for the patients. The earliest first bone transfer was done all the way back in 2000 BCE when the Peruvian priest implanted a metallic plate to reconstruct the contour defects of the religious trephination. In 1668, a man by the name of Jobs van Meekeren reported the use of dog bone grafts to reconstruct the calvarium in the soldier. "…the ideal of the future: the insertion of a piece of living bone which will exactly fill the gap and will continue to live without absorption." (The Epitome of Medicine).
Free Skin and Free Fat Transfer
The radial forearm is the most commonly dominant use of flap to be used to coverage up damages. Today, the anterolateral thigh flap is being used on patients for the head and the neck because it has an ideal match for the site and it is easy to harvest. If a surgeon chose to remove/harvest the tissue, safe places are the following; skin, skin and fat, fat and fascia, or just the fascia by itself.
Microvascular reconstruction repair
Microvascular reconstruction repair is a common operation that is done on patients who see an Otorhinolaryngologist. Microvascular reconstruction repair is a surgical procedure that involves moving a composite piece of tissue from the patient's body and moves it to the head and or neck. Microvascular head and neck reconstruction is used to treat head and neck cancers, including those of the larynx and pharynx, oral cavity, salivary glands, jaws, calvarium, sinuses, tongue and skin. The tissue that is most common moved during this procedure is from the arms, legs, back, and can come from the skin, bone, fat, and or muscle.[8] When doing this procedure, the decision on which is moved is determined on the reconstructive needs. Transfer of the tissue to the head and neck allows surgeons to rebuild the patient's jaw, optimize tongue function, and reconstruct the throat. When the pieces of tissue are moved, they require their own blood supply for a chance of survival in their new location. After the surgery is completed, the blood vessels that feed the tissue transplant are reconnected to new blood vessels in the neck. These blood vessels are typically no more than 1 to 3 millimeters in diameter which means these connections need to be made with a microscope which is why this procedure is called "microvascular surgery."
See also
References
- "otolaryngologist" entry in: Peter Harris, Sue Nagy, Nicholas Vardaxis, Mosby's Dictionary of Medicine, Nursing & Health Professions - Australian & New Zealand Edition, Elsevier Health Sciences, 2009.
- "Otolaryngology Specialty Description". American Medical Association.
- "Is There a Crisis in the Otolaryngology Match?". ENTtoday. Retrieved 16 April 2020.
- "National Residency Match Program 2020" (PDF). National Residency Match Program.
- "Training and development (otorhinolaryngology)". Health Careers. 16 April 2015. Retrieved 16 April 2020.
- Goyal, Neerav; Jowett, Nathan; Dwojak, Sunshine; Cunane, Mary Beth; Zander, David; Hadlock, Tessa A.; Emerick, Kevin S. (24 June 2016). "Use of the submental vessels for free gracilis muscle transfer for smile reanimation". Head & Neck. 38 (10): E2499–E2503. doi:10.1002/hed.24478. ISSN 1043-3074. PMID 27341470.
- "Microvascular Head and Neck Reconstruction | Conditions & Treatments | UCSF Medical Center". www.ucsfhealth.org. Retrieved 6 December 2018.