Hydrogel
A hydrogel is a network of crosslinked polymer chains that are hydrophilic, sometimes found as a colloidal gel in which water is the dispersion medium. A three-dimensional solid results from the hydrophilic polymer chains being held together by cross-links. The crosslinks which bond the polymers of a hydrogel fall under two general categories: physical and chemical. Physical crosslinks consist of hydrogen bonds, hydrophobic interactions, and chain entanglements (among others). Because of the inherent cross-links, the structural integrity of the hydrogel network does not dissolve from the high concentration of water.[1] Hydrogels are highly absorbent (they can contain over 90% water) natural or synthetic polymeric networks.
The first appearance of the term 'hydrogel' in the literature was in 1894.[2]
Uses

Common uses include:
- Scaffolds in tissue engineering.[3] When used as scaffolds, hydrogels may contain human cells to repair tissue. They mimic 3D microenvironment of cells.[4]
- Hydrogel-coated wells have been used for cell culture.[5]
- Investigating biomechanical functions in cells when combined with Holotomography microscopy
- Environmentally sensitive hydrogels (also known as 'Smart Gels' or 'Intelligent Gels'). These hydrogels have the ability to sense changes of pH, temperature, or the concentration of metabolite and release their load as result of such a change.[6]
- Injectable hydrogels which can be used as drug carriers for treatment of diseases or as cell carriers for regenerative purposes or tissue engineering.[7][8][9]
- Sustained-release drug delivery systems. Ionic strength, pH and temperature can be used as a triggering factor to control the release of the drug.[10]
- Providing absorption, desloughing and debriding of necrotic and fibrotic tissue
- Hydrogels that are responsive to specific molecules,[11] such as glucose or antigens, can be used as biosensors, as well as in DDS.[12]
- Disposable diapers where they absorb urine, or in sanitary napkins[13]
- Contact lenses (silicone hydrogels, polyacrylamides, polymacon)
- EEG and ECG medical electrodes using hydrogels composed of cross-linked polymers (polyethylene oxide, polyAMPS and polyvinylpyrrolidone)
- Water gel explosives
- Rectal drug delivery and diagnosis
- Encapsulation of quantum dots
- Breast implants
- Glue
- Granules for holding soil moisture in arid areas
- Dressings for healing of burn or other hard-to-heal wounds. Wound gels are excellent for helping to create or maintain a moist environment.
- Reservoirs in topical drug delivery; particularly ionic drugs, delivered by iontophoresis (see ion exchange resin).
- Materials mimicking animal mucosal tissues to be used for testing mucoadhesive properties of drug delivery systems[14][15]
- Thermodynamic electricity generation. When combined with ions allows for heat dissipation for electronic devices and batteries and converting the heat exchange to an electrical charge.[16]
Chemistry
Common ingredients include polyvinyl alcohol, polyethylene glycol, sodium polyacrylate, acrylate polymers and copolymers with an abundance of hydrophilic groups, and natural proteins such as collagen, gelatin and fibrin.
The crosslinks which bond the polymers of a hydrogel fall under two general categories: physical and chemical. Physical crosslinks consist of hydrogen bonds, hydrophobic interactions, and chain entanglements (among others). A hydrogel generated through the use of physical crosslinks is sometimes called a ‘reversible’ hydrogel. Chemical crosslinks consist of covalent bonds between polymer strands. Hydrogels generated in this manner are sometimes called ‘permanent’ hydrogels.
One notable method of initiating a polymerization reaction involves the use of light as a stimulus. In this method, photoinitiators, compounds that cleave from the absorption of photons, are added to the precursor solution which will become the hydrogel. When the precursor solution is exposed to a concentrated source of light, the photoinitiators will cleave and form free radicals, which will begin a polymerization reaction that forms crosslinks between polymer strands. This reaction will cease if the light source is removed, allowing the amount of crosslinks formed in the hydrogel to be controlled.[17] The properties of a hydrogel are highly dependent on the type and quantity of its crosslinks, making photopolymerization a popular choice for fine-tuning hydrogels. This technique has seen considerable use in cell and tissue engineering applications due to the ability to inject or mold a precursor solution loaded with cells into a wound site, then solidify it in situ.[13][17]
Hydrogels also possess a degree of flexibility very similar to natural tissue, due to their significant water content. As responsive "smart materials," hydrogels can encapsulate chemical systems which upon stimulation by external factors such as a change of pH may cause specific compounds such as glucose to be liberated to the environment, in most cases by a gel-sol transition to the liquid state. Chemomechanical polymers are mostly also hydrogels, which upon stimulation change their volume and can serve as actuators or sensors.
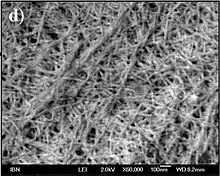 A short-peptide-based hydrogel matrix, capable of holding about one hundred times its own weight in water. Developed as a medical dressing. The thickness of the fibers was on the order of tens of nm, mimicking the fibrous microenvironment found in the extracellular matrix. Field emission scanning electron microscopy image
A short-peptide-based hydrogel matrix, capable of holding about one hundred times its own weight in water. Developed as a medical dressing. The thickness of the fibers was on the order of tens of nm, mimicking the fibrous microenvironment found in the extracellular matrix. Field emission scanning electron microscopy image Photo of the same short-peptide-based hydrogel, held in forceps to demonstrate its stiffness and transparency.
Photo of the same short-peptide-based hydrogel, held in forceps to demonstrate its stiffness and transparency.
Mechanical properties
Hydrogels possess a vast range of mechanical properties, which is one of the primary reasons why they have recently been investigated for a wide spread of applications. By modifying the polymer concentration of a hydrogel (or conversely, the water concentration), the Young’s Modulus, Shear Modulus, and Storage Modulus can vary from 10 Pa to 3 MPa, a range of about five orders of magnitude.[19] A similar effect can be seen by altering the crosslinking concentration.[19] This much variability of the mechanical stiffness is why hydrogels are so appealing for biomedical applications, where it is vital for implants to match the mechanical properties of the surrounding tissues.[20]
Hydrogels have two main regimes of mechanical properties: rubber elasticity and viscoelasticity:
Rubber elasticity
In the unswollen state, hydrogels can be modelled as highly crosslinked chemical gels, in which the system can be described as one continuous polymer network. In this case:
where G is the shear modulus, k is the Boltzmann constant, T is temperature, Np is the number of polymer chains per unit volume, ρ is the density, R is the ideal gas constant, and is the (number) average molecular weight between two adjacent cross-linking points. can be calculated from the swell ratio, Q, which is relatively easy to test and measure.[19]
For the swollen state, a perfect gel network can be modeled as:[19]
In a simple uniaxial extension or compression test, the true stress, , and engineering stress, , can be calculated as:
where is the stretch.[19]
Viscoelasticity
In order to describe the time-dependent creep and stress-relaxation behavior of hydrogel, a variety of physical lumped parameter models can be used.[19] These modeling methods vary greatly and are extremely complex, so the empirical Prony Series description is commonly used to describe the viscoelastic behavior in hydrogels.[19]
Environmental response
The most commonly seen environmental sensitivity in hydrogels is a response to temperature.[21] Many polymers/hydrogels exhibit a temperature dependent phase transition, which can be classified as either an Upper Critical Solution Temperature (UCST) or Lower Critical Solution Temperature (LCST). UCST polymers increase in their water-solubility at higher temperatures, which lead to UCST hydrogels transitioning from a gel (solid) to a solution (liquid) as the temperature is increased (similar to the melting point behavior of pure materials). This phenomenon also causes UCST hydrogels to expand (increase their swell ratio) as temperature increases while they are below their UCST.[21] However, polymers with LCSTs display an inverse (or negative) temperature-dependence, where their water-solubility decreases at higher temperatures. LCST hydrogels transition from a liquid solution to a solid gel as the temperature is increased, and they also shrink (decrease their swell ratio) as the temperature increases while they are above their LCST.[21]
Different applications call for different thermal responses. For example, in the biomedical field, LCST hydrogels are being investigated as drug delivery systems due to being injectable (liquid) at room temp and then solidifying into a rigid gel upon exposure to the higher temperatures of the human body.[21] There are many other stimuli that hydrogels can be responsive to, including: pH, glucose, electrical signals, light, pressure, ions, antigens, and more.[21]
Additives
There are many ways to fine-tune the mechanical properties of hydrogels. One of the most simple is to use different molecules for the backbone and crosslinkers of the hydrogel system, as different molecules will have different intermolecular interactions with each other and different interactions with the absorbed water.[21][22] Another method of modifying the strength or elasticity of hydrogels is to graft or surface coat them onto a stronger/stiffer support, or by making superporous hydrogel (SPH) composites, in which a cross-linkable matrix swelling additive is added.[23] Other additives, such as nanoparticles and microparticles, have been shown to significantly modify the stiffness and gelation temperature of certain hydrogels used in biomedical applications.[24][25][26]
Research
Natural hydrogel materials are being investigated for tissue engineering; these materials include agarose, methylcellulose, hyaluronan, Elastin like polypeptides and other naturally derived polymers. Hydrogels show promise for use in agriculture, as they can release agrochemicals including pesticides and phosphate fertiliser slowly, increasing efficiency and reducing runoff, and at the same time improve the water retention of drier soils such as sandy loams.[27]
In the 2000 there has been an increase in research on the use of hydrogels for drug delivery. Polymeric drug delivery systems have overcome challenge due to their biodegradability, biocompatibility and anti-toxicity.[28] Recent advances have fueled the formulation and synthesis of hydrogels that provide strong backbone for efficient component for drug delivery systems.[29] Materials such as collagen, chitosan, cellulose and poly (lactic-co-glycolic acid) all have been implemented extensively for drug delivery to various important organs in the human body such as: the eye,[30] nose, kidneys,[31] lungs,[32] intestines,[33] skin[34] and the brain. Future work is focused on better anti-toxicity of hydrogels, varying assembly techniques for hydrogels making them more biocompatible[35] and the delivery of complex systems such as using hydrogels to deliver therapeutic cells.[36]
References
- Warren, David S.; Sutherland, Sam P. H.; Kao, Jacqueline Y.; Weal, Geoffrey R.; Mackay, Sean M. (2017-04-20). "The Preparation and Simple Analysis of a Clay Nanoparticle Composite Hydrogel". Journal of Chemical Education. 94 (11): 1772–1779. Bibcode:2017JChEd..94.1772W. doi:10.1021/acs.jchemed.6b00389. ISSN 0021-9584.
- "Der Hydrogel und das kristallinische Hydrat des Kupferoxydes". Zeitschrift für Chemie und Industrie der Kolloide. 1 (7): 213–214. 1907. doi:10.1007/BF01830147. S2CID 197928622.
- Talebian, Sepehr; Mehrali, Mehdi; Taebnia, Nayere; Pennisi, Cristian Pablo; Kadumudi, Firoz Babu; Foroughi, Javad; Hasany, Masoud; Nikkhah, Mehdi; Akbari, Mohsen; Orive, Gorka; Dolatshahi‐Pirouz, Alireza (2019). "Self-Healing Hydrogels: The Next Paradigm Shift in Tissue Engineering?". Advanced Science. 6 (16): 1801664. doi:10.1002/advs.201801664. ISSN 2198-3844. PMC 6702654. PMID 31453048.
- Mellati, Amir; Dai, Sheng; Bi, Jingxiu; Jin, Bo; Zhang, Hu (2014). "A biodegradable thermosensitive hydrogel with tuneable properties for mimicking three-dimensional microenvironments of stem cells". RSC Adv. 4 (109): 63951–63961. doi:10.1039/C4RA12215A. ISSN 2046-2069.
- Discher, D. E.; Janmey, P.; Wang, Y.L. (2005). "Tissue Cells Feel and Respond to the Stiffness of Their Substrate" (PDF). Science. 310 (5751): 1139–43. Bibcode:2005Sci...310.1139D. CiteSeerX 10.1.1.318.690. doi:10.1126/science.1116995. PMID 16293750. S2CID 9036803.
- Brudno, Yevgeny (2015-12-10). "On-demand drug delivery from local depots". Journal of Controlled Release. 219: 8–17. doi:10.1016/j.jconrel.2015.09.011. PMID 26374941.
- Lee, Jin Hyun (December 2018). "Injectable hydrogels delivering therapeutic agents for disease treatment and tissue engineering". Biomaterials Research. 22 (1): 27. doi:10.1186/s40824-018-0138-6. ISSN 2055-7124. PMC 6158836. PMID 30275970.
- Liu, Mei; Zeng, Xin; Ma, Chao; Yi, Huan; Ali, Zeeshan; Mou, Xianbo; Li, Song; Deng, Yan; He, Nongyue (December 2017). "Injectable hydrogels for cartilage and bone tissue engineering". Bone Research. 5 (1): 17014. doi:10.1038/boneres.2017.14. ISSN 2095-6231. PMC 5448314. PMID 28584674.
- Pupkaite, Justina; Rosenquist, Jenny; Hilborn, Jöns; Samanta, Ayan (2019-09-09). "Injectable Shape-Holding Collagen Hydrogel for Cell Encapsulation and Delivery Cross-linked Using Thiol-Michael Addition Click Reaction". Biomacromolecules. 20 (9): 3475–3484. doi:10.1021/acs.biomac.9b00769. ISSN 1525-7797. PMID 31408340.
- Malmsten, Martin; Bysell, Helena; Hansson, Per (2010-12-01). "Biomacromolecules in microgels — Opportunities and challenges for drug delivery". Current Opinion in Colloid & Interface Science. 15 (6): 435–444. doi:10.1016/j.cocis.2010.05.016. ISSN 1359-0294.
- Chemoresponsive Materials, Editor: Hans-Jörg Schneider, Royal Society of Chemistry, Cambridge 2015, https://pubs.rsc.org/en/content/ebook/978-1-78262-242-0
- Yetisen, A. K.; Naydenova, I; Da Cruz Vasconcellos, F; Blyth, J; Lowe, C. R. (2014). "Holographic Sensors: Three-Dimensional Analyte-Sensitive Nanostructures and their Applications". Chemical Reviews. 114 (20): 10654–96. doi:10.1021/cr500116a. PMID 25211200.
- Caló, Enrica; Khutoryanskiy, Vitaliy V. (2015). "Biomedical applications of hydrogels: A review of patents and commercial products". European Polymer Journal. 65: 252–267. doi:10.1016/j.eurpolymj.2014.11.024.
- Cook, Michael T.; Smith, Sarah L.; Khutoryanskiy, Vitaliy V. (2015). "Novel glycopolymer hydrogels as mucosa-mimetic materials to reduce animal testing". Chem. Commun. 51 (77): 14447–14450. doi:10.1039/C5CC02428E. PMID 26221632.
- Cook, Michael T.; Khutoryanskiy, Vitaliy V. (2015). "Mucoadhesion and mucosa-mimetic materials—A mini-review". International Journal of Pharmaceutics. 495 (2): 991–8. doi:10.1016/j.ijpharm.2015.09.064. hdl:2299/16856. PMID 26440734.
- "A new way to cool down electronic devices, recover waste heat". Phys.org. April 22, 2020. Retrieved April 23, 2020.
- Choi, J. R.; Yong, K. W.; Choi, J. Y.; Cowie, A. C. (2019). "Recent advances in photo-crosslinkable hydrogels for biomedical applications". BioTechniques. 66 (1): 40–53. doi:10.2144/btn-2018-0083. PMID 30730212.
- Kwon, Gu Han; Jeong, Gi Seok; Park, Joong Yull; Moon, Jin Hee; Lee, Sang-Hoon (2011). "A low-energy-consumption electroactive valveless hydrogel micropump for long-term biomedical applications". Lab on a Chip. 11 (17): 2910–5. doi:10.1039/C1LC20288J. PMID 21761057.
- Oyen, M. L. (January 2014). "Mechanical characterisation of hydrogel materials". International Materials Reviews. 59 (1): 44–59. doi:10.1179/1743280413Y.0000000022. ISSN 0950-6608. S2CID 136844625.
- Los, Marek J.; Hudecki, Andrzej; Wiechec, Emilia (2018-11-07). Stem Cells and Biomaterials for Regenerative Medicine. Academic Press. ISBN 978-0-12-812278-5.
- Qiu, Yong; Park, Kinam (December 2001). "Environment-sensitive hydrogels for drug delivery". Advanced Drug Delivery Reviews. 53 (3): 321–339. doi:10.1016/S0169-409X(01)00203-4. PMID 11744175.
- Zaragoza, J; Chang, A; Asuri, P (January 2017). "Effect of crosslinker length on the elastic and compression modulus of poly(acrylamide) nanocomposite hydrogels". Journal of Physics: Conference Series. 790 (1): 012037. doi:10.1088/1742-6596/790/1/012037. ISSN 1742-6588.
- Ahmed, Enas M. (March 2015). "Hydrogel: Preparation, characterization, and applications: A review". Journal of Advanced Research. 6 (2): 105–121. doi:10.1016/j.jare.2013.07.006. PMC 4348459. PMID 25750745.
- Cidade, M.; Ramos, D.; Santos, J.; Carrelo, H.; Calero, N.; Borges, J. (2019-04-02). "Injectable Hydrogels Based on Pluronic/Water Systems Filled with Alginate Microparticles for Biomedical Applications". Materials. 12 (7): 1083. Bibcode:2019Mate...12.1083C. doi:10.3390/ma12071083. ISSN 1996-1944. PMC 6479463. PMID 30986948.
- Rose, Séverine; Prevoteau, Alexandre; Elzière, Paul; Hourdet, Dominique; Marcellan, Alba; Leibler, Ludwik (January 2014). "Nanoparticle solutions as adhesives for gels and biological tissues". Nature. 505 (7483): 382–385. doi:10.1038/nature12806. ISSN 1476-4687. PMID 24336207. S2CID 205236639.
- Zaragoza, Josergio; Fukuoka, Scott; Kraus, Marcus; Thomin, James; Asuri, Prashanth (November 2018). "Exploring the Role of Nanoparticles in Enhancing Mechanical Properties of Hydrogel Nanocomposites". Nanomaterials. 8 (11): 882. doi:10.3390/nano8110882. PMC 6265757. PMID 30380606.
- Puoci, Francesco; et al. (2008). "Polymer in Agriculture: A Review" (PDF). American Journal of Agricultural and Biological Sciences. 3 (1): 299–314. doi:10.3844/ajabssp.2008.299.314.
- Tang, Yiqing; Heaysman, Clare L.; Willis, Sean; Lewis, Andrew L. (2011-09-01). "Physical hydrogels with self-assembled nanostructures as drug delivery systems". Expert Opinion on Drug Delivery. 8 (9): 1141–1159. doi:10.1517/17425247.2011.588205. ISSN 1742-5247. PMID 21619469. S2CID 24843309.
- Aurand, Emily R.; Lampe, Kyle J.; Bjugstad, Kimberly B. (March 2012). "Defining and designing polymers and hydrogels for neural tissue engineering". Neuroscience Research. 72 (3): 199–213. doi:10.1016/j.neures.2011.12.005. PMC 3408056. PMID 22192467.
- Ozcelik, Berkay; Brown, Karl D.; Blencowe, Anton; Daniell, Mark; Stevens, Geoff W.; Qiao, Greg G. (May 2013). "Ultrathin chitosan–poly(ethylene glycol) hydrogel films for corneal tissue engineering". Acta Biomaterialia. 9 (5): 6594–6605. doi:10.1016/j.actbio.2013.01.020. PMID 23376126.
- Gao, Jiasheng; Liu, Rongfu; Wu, Jie; Liu, Zhiqiang; Li, Junjie; Zhou, Jin; Hao, Tong; Wang, Yan; Du, Zhiyan; Duan, Cuimi; Wang, Changyong (May 2012). "The use of chitosan based hydrogel for enhancing the therapeutic benefits of adipose-derived MSCs for acute kidney injury". Biomaterials. 33 (14): 3673–3681. doi:10.1016/j.biomaterials.2012.01.061. PMID 22361096.
- Otani, Yuto; Tabata, Yasuhiko; Ikada, Yoshito (April 1999). "Sealing effect of rapidly curable gelatin-poly (l-glutamic acid) hydrogel glue on lung air leak". The Annals of Thoracic Surgery. 67 (4): 922–926. doi:10.1016/S0003-4975(99)00153-8. PMID 10320229.
- Ramdas, M.; Dileep, K. J.; Anitha, Y.; Paul, Willi; Sharma, Chandra P. (April 1999). "Alginate Encapsulated Bioadhesive Chitosan Microspheres for Intestinal Drug Delivery". Journal of Biomaterials Applications. 13 (4): 290–296. doi:10.1177/088532829901300402. ISSN 0885-3282. PMID 10340211. S2CID 31364133.
- Liu, Xing; Ma, Lie; Mao, Zhengwei; Gao, Changyou (2011), Jayakumar, Rangasamy; Prabaharan, M.; Muzzarelli, Riccardo A. A. (eds.), "Chitosan-Based Biomaterials for Tissue Repair and Regeneration", Chitosan for Biomaterials II, Advances in Polymer Science, Springer Berlin Heidelberg, pp. 81–127, doi:10.1007/12_2011_118, ISBN 978-3-642-24061-4
- Wu, Zi Liang; Gong, Jian Ping (June 2011). "Hydrogels with self-assembling ordered structures and their functions". NPG Asia Materials. 3 (6): 57–64. doi:10.1038/asiamat.2010.200. ISSN 1884-4057.
- Kim, Jinku; Yaszemski, Michael J.; Lu, Lichun (December 2009). "Three-dimensional porous biodegradable polymeric scaffolds fabricated with biodegradable hydrogel porogens". Tissue Engineering. Part C, Methods. 15 (4): 583–594. doi:10.1089/ten.TEC.2008.0642. ISSN 1937-3392. PMC 2819712. PMID 19216632.
