Hyperphosphatemia
Hyperphosphatemia is an electrolyte disorder in which there is an elevated level of phosphate in the blood.[1] Most people have no symptoms while others develop calcium deposits in the soft tissue.[1] Often there is also low calcium levels which can result in muscle spasms.[1]
| Hyperphosphatemia | |
|---|---|
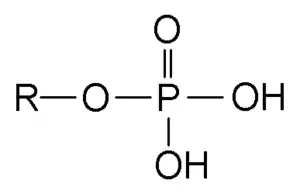 | |
| Phosphate group chemical structure | |
| Specialty | Endocrinology, nephrology |
| Symptoms | None, calcium deposits, muscle spasms[1] |
| Complications | Low blood calcium[1] |
| Causes | Kidney failure, pseudohypoparathyroidism, hypoparathyroidism, diabetic ketoacidosis, tumor lysis syndrome, rhabdomyolysis[1] |
| Diagnostic method | Blood phosphate > 1.46 mmol/L (4.5 mg/dL)[1] |
| Differential diagnosis | High blood lipids, high blood protein, high blood bilirubin[1] |
| Treatment | Decreasing intake, calcium carbonate[1] |
| Frequency | Unclear[2] |
Causes include kidney failure, pseudohypoparathyroidism, hypoparathyroidism, diabetic ketoacidosis, tumor lysis syndrome, and rhabdomyolysis.[1] Diagnosis is generally based on a blood phosphate levels of greater than 1.46 mmol/L (4.5 mg/dL).[1] When levels are greater than 4.54 mmol/L (14 mg/dL) it is deemed severe.[3] Levels may appear falsely elevated with high blood lipid levels, high blood protein levels, or high blood bilirubin levels.[1]
Treatment may include eating a phosphate low diet and antacids, like calcium carbonate, that bind phosphate.[1] Occasionally intravenous normal saline or dialysis may be used.[1] How commonly it occurs is unclear.[2]
Signs and symptoms
Signs and symptoms include ectopic calcification, secondary hyperparathyroidism, and renal osteodystrophy. Abnormalities in phosphate metabolism such as hyperphosphatemia are included in the definition of the new chronic kidney disease-mineral and bone disorder (CKD-MBD).[4]
Causes
| Impaired renal phosphate excretion[5] |
|
| Massive extracellular fluid phosphate loads[5] |
|
Hypoparathyroidism: In this situation, there are low levels of parathyroid hormone (PTH). PTH normally inhibits reabsorption of phosphate by the kidney. Therefore, without enough PTH there is more reabsorption of the phosphate leading to a high phosphate level in the blood.
Chronic kidney failure: When the kidneys are not working well, there will be increased phosphate retention.
Drugs: hyperphosphatemia can also be caused by taking oral sodium phosphate solutions prescribed for bowel preparation for colonoscopy in children.
Diagnosis
The diagnosis of hyperphosphatemia is made through measuring the concentration of phosphate in the blood. A phosphate concentration greater than 1.46 mmol/l (4.5 mg/dl) is indicative of hyperphosphatemia, though further tests may be needed to identify the underlying cause of the elevated phosphate levels.[6] It is considered severe when levels are greater than 1.6 mmol/l ( 5mg/dl).[2]
Units
Phosphates in blood exist in a chemical equilibrium of hydrogen phosphate (HPO42–) and dihydrogen phosphate (H2PO4–), which have different masses. Phosphate (PO43–) and phosphoric acid (H3PO4) are not present in significant amounts. Thus millimoles per liter (mmol/l) are often used to denote the phosphate concententration. If milligrams per decililiter (mg/dl) is used, it often denotes the mass of phosphorus bound to phosphates, but not the mass of some individual phosphate.[7]
Treatment
High phosphate levels can be avoided with phosphate binders and dietary restriction of phosphate.[6] If the kidneys are operating normally, a saline diuresis can be induced to renally eliminate the excess phosphate. In extreme cases, the blood can be filtered in a process called hemodialysis, removing the excess phosphate.[6] Phosphate-binding medications include sevelamer, lanthanum carbonate, calcium carbonate, and calcium acetate.[8] Previously aluminum hydroxide was the medication of choice, but its use has been largely abandoned due to the increased risk of aluminum toxicity.[9]
References
- "Hyperphosphatemia". Merck Manuals Professional Edition. Retrieved 27 October 2018.
- Ronco, Claudio; Bellomo, Rinaldo; Kellum, John A. (2008). SPEC - Critical Care Nephrology Expert Consult (Book Program) Pincard. Elsevier Health Sciences. p. 533. ISBN 978-1437711110.
- Adams, James G. (2012). Emergency Medicine: Clinical Essentials (Expert Consult - Online and Print). Elsevier Health Sciences. p. 1416. ISBN 978-1455733941.
- "KDIGO Guideline for Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD)". Archived from the original on 4 March 2017. Retrieved 7 February 2016. Cite journal requires
|journal=(help) - Longo et al., Harrison's Principles of Internal Medicine, 18th ed., p.3089
- "Hyperphosphatemia - Endocrine and Metabolic Disorders - Merck Manuals Professional Edition". Merck Manuals Professional Edition. Merck Sharp & Dohme Corp. Retrieved 23 October 2017.
- Lerma EV, et al. (2019). Nephrology secrets (4th ed.). pp. 532–533. ISBN 9780323478717.
- Critical care nursing : diagnosis and management. Urden, Linda Diann. (7th ed.). St. Louis, Mo.: Elsevier/Mosby. 2014. p. 716. ISBN 978-0-323-09178-7. OCLC 830669119.CS1 maint: others (link)
- Hutchison, Alastair J.; Smith, Craig P.; Brenchley, Paul E. C. (October 2011). "Pharmacology, efficacy and safety of oral phosphate binders". Nature Reviews Nephrology. 7 (10): 578–589. doi:10.1038/nrneph.2011.112. ISSN 1759-5061. PMID 21894188. S2CID 19833271.
External links
| Classification | |
|---|---|
| External resources |