Periodontal fiber
The periodontal ligament, commonly abbreviated as the PDL, is a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which it sits.[1] It inserts into root cementum one side and onto alveolar bone on the other.
| Periodontal ligament | |
|---|---|
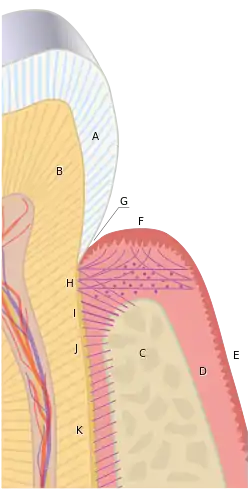 The tissues of the periodontium combine to form an active, dynamic group of tissues. The alveolar bone (C) is surrounded for the most part by the subepithelial connective tissue of the gingiva, which in turn is covered by the various characteristic gingival epithelia. The cementum overlaying the tooth root is attached to the adjacent cortical surface of the alveolar bone by the alveolar crest (I), horizontal (J) and oblique (K) fibers of the periodontal ligament. | |
| Details | |
| Precursor | dental follicle |
| Identifiers | |
| Latin | fibra periodontalis |
| Acronym(s) | PDL |
| MeSH | D010513 |
| FMA | 56665 |
| Anatomical terminology | |
Structure
The PDL consists of principal fibres, loose connective tissue, blast and clast cells, oxytalan fibres and Cell Rest of Malassez.[2]
Alveolodental ligament
The main principal fiber group is the alveolodental ligament, which consists of five fiber subgroups: alveolar crest, horizontal, oblique, apical, and interradicular on multirooted teeth. Principal fibers other than the alveolodental ligament are the transseptal fibers.
All these fibers help the tooth withstand the naturally substantial compressive forces that occur during chewing and remain embedded in the bone. The ends of the principal fibers that are within either cementum or alveolar bone proper are considered Sharpey fibers.
- Alveolar crest fibers (I) run from the cervical part of the root to the alveolar bone crest
- Horizontal fibers (J) attach to the cementum apical to the alveolar crest fibers and run perpendicularly from the root of the tooth to the alveolar bone..
- Oblique fibers (K) are the most numerous fibers in the periodontal ligament, running from cementum in an oblique direction to insert into bone coronally. These fibres resist vertical & intrusive forces
- Apical fibers are found radiating from cementum around the apex of the root to the bone, forming base of the socket or alveolus.
- Interradicular fibers are only found between the roots of multirooted teeth, such as premolars and molars. They extend from radicular cementum to interradicular alveolar bone.
Transseptal fibers
Transseptal fibers (H) extend interproximally over the alveolar bone crest and are embedded in the cementum of adjacent teeth; they form an interdental ligament. These fibers keep all the teeth aligned. These fibers may be considered as belonging to the gingival tissue because they do not have an osseous attachment.[3]
Loose connective tissue
Loose connective tissue contains fibres, extracellular matrix, cells, nerves and blood vessels. The extracellular compartment consists of Type 1, 3, and 5 collagen fibers bundles embedded in intercellular substance. The PDL collagen fibers are categorized according to their orientation and location along the tooth. The cells include fibroblast, defence cells and undifferentiated mesenchymal cells.
Cell Rest of Malassez
These groups of epithelial cells become located in the mature PDL after the disintegration of Hertwig epithelial root sheath during the formation of the root.[2]They form a plexus that surrounds the tooth. Cell Rests of Malassez might proliferate during inflammation which may lead to radicular cyst formation in later life.
Oxytalan fibres
Oxytalan fibres are unique to the PDL and are elastic in nature. It inserts into cementum and runs in 2 directions; parallel to root surface and oblique to root surface. The function is thought to maintain the patency of blood vessels during occlusal loading. Further research is needed to determine the function of oxytalan fibres.[4]
Composition
The PDL substance has been estimated to be 70% water, which is thought to have a significant effect on the tooth's ability to withstand stress loads. The completeness and vitality of the PDL are essential for the functioning of the tooth.
The PDL ranges in width from 0.15 to 0.38mm with its thinnest part located in the middle third of the root.[5] The width progressively decreases with age.
The PDL is a part of the periodontium that provides for the attachment of the teeth to the surrounding alveolar bone by way of the cementum.
The PDL appears as the periodontal space of 0.4 to 1.5 mm on radiographs, a radiolucent area between the radiopaque lamina dura of the alveolar bone proper and the radiopaque cementum.
Development
PDL cells are one of the many cells derived from the dental follicle and this occurs after crown formation is completed and when the roots start developing. These cells will remodel the dental follicle to form the PDL.[5] Formation of PDL will start at the cementoenamel junction and proceeds in an apical direction. .[6]
Function
Functions of PDL are supportive, sensory, nutritive, and remodelling.[7]
Support
The PDL is a part of the periodontium that provides for the attachment of the teeth to the surrounding alveolar bone by way of the cementum. PDL fibres also provide a role in load transfer between the teeth and alveolar bone. (PDL fibres absorb and transmit forces between teeth and alveolar bone. It acts as an effective support during the masticatory function.)[8]
Sensory
PDL is heavily innervated; it involves mechanoreception, nociception and reflexes. Periodontal mechanoreceptors are present in pdl. They will transmit information about the stimulated tooth, direction and amplitude of forces.[9]
Nutritive
It maintains the vitality of the surrounding cells. (PDL is heavily anastomosed). There are 3 principal sources of blood vessels which are apical vessels, perforating vessels and gingival vessels. Apical vessels originate from vessels that supply the pulp. Perforating vessels originate from lamina dura and the vessels perforate the socket wall (cribriform plate). Gingival vessels are derived from the gingival tissue. Outer layers of blood supply in PDL may help in mechanical suspension and support of the tooth while inner layers of blood vessels supply surrounding PDL tissues.[10]
Remodeling
There are progenitor cells in the periodontal ligament that can differentiate into osteoblasts for the physiological maintenance of alveolar bone and, most likely, for its repair as well.
Clinical significance
Injury
- When traumatic forces of occlusion are placed on a tooth, the PDL widens to take the extra forces. Thus, early occlusal trauma can be viewed on radiographs as a widening of the periodontal ligament space. Thickening of the lamina dura in response is also possible. Clinically, occlusal trauma is noted by the late manifestation of increased mobility of the tooth and possibly the presence of pathological tooth migration.[5]
- Damage to the PDL may result in tooth ankylosis to the jawbone, making the tooth lose its continuous eruption ability. Dental trauma, such as subluxation, may cause tearing of the PDL and pain during function (eating).[11]
- The PDL cells of an avulsed tooth is at risk of drying and desiccation if left in dry storage. Wet storage in an isotonic liquid, although a superior method to dry storage, can preserve PDL vitality depending on the medium but not for an indefinite period of time. All of these can lead to loss of vitality of the PDL and depending on the duration of storage, this can affect the success of subsequent replantation.[12]
Disease
- The epithelial rests of Malassez can become cystic, usually forming nondiagnostic, radiolucent apical lesions that can be seen on radiographs. This occurs as a result of chronic periapical inflammation after pulpitis occurs and must be surgically removed.[5]
- The PDL also undergoes drastic changes with chronic periodontal disease that involves the deeper structures of the periodontium with periodontitis. The fibers of the PDL become disorganized, and their attachments to either the alveolar bone proper or cementum through Sharpey fibers are lost because of the resorption of these two hard dental tissue.[5]
- Pathological damaged or diseased PDL can result in delayed healing of the alveolar socket in cases where the diseased tooth is ultimately extracted.[13]
References
- Herbert F. Wolf; Klaus H. Rateitschak (2005). Periodontology. Thieme. pp. 12–. ISBN 978-0-86577-902-0. Retrieved 21 June 2011.
- Max A. Listgarten, University of Pennsylvania and Temple University, It is the different composition of collagens which give various ECM functions and abilities. There is a mixture of thick and thin fibres in the PDL. It is important to note that, in reality, the fibres are not as defined as these classifications. http://www.dental.pitt.edu/informatics/periohistology/en/gu0404.htm
- Ten Cate's Oral Histolog, Nanci, Elsevier, 2013, page 274
- The oxytalan fibre network in the periodontium and its possible mechanical function Archives of Oral Biology, Volume 57, Issue 8, Pages 1003-1011 Hardus Strydom, Jaap C. Maltha, Anne M. Kuijpers-Jagtman, Johannes W. Von den Hoff Help
- Yao S, Pan F, Prpic V, Wise GE. Differentiation of stem cells in the dental follicle. J Dent Res. 2008;87:767-771.
- De Jong T, Bakker AD, Everts V, Smit TH. The intricate anatomy of the periodontal ligament and its development: Lessons for periodontal regeneration. J Periodont Res. 2017;00:1–10
- Max A. Listgarten, University of Pennsylvania and Temple University at http://www.dental.pitt.edu/informatics/periohistology/en/gu0401.htm
- McCormack SW, Witzel U, Watson PJ, Fagan MJ, Gröning F. The Biomechanical Function of Periodontal Ligament Fibres in Orthodontic Tooth Movement. Agarwal S, ed. PLoS ONE. 2014;9(7):e102387. doi:10.1371/journal.pone.0102387.
- Trulsson, M. (2006). Sensory-motor function of human periodontal mechanoreceptors*. Journal of Oral Rehabilitation, 33(4), 262-273. doi:10.1111/j.1365-2842.2006.01629.x
- Institute of Anatomy, University of Veterinary Medicine Hannover, Bischofsholer Damm 15, D-30173 Hannover, Germany
- Zadik Y (December 2008). "Algorithm of first-aid management of dental trauma for medics and corpsmen". Dent Traumatol. 24 (6): 698–701. doi:10.1111/j.1600-9657.2008.00649.x. PMID 19021668.
- Layug, M. L.; Barrett, E. J.; Kenny, D. J. (May 1998). "Interim storage of avulsed permanent teeth". Journal (Canadian Dental Association). 64 (5): 357–363, 365–369. ISSN 0709-8936. PMID 9648418.
- Kim, Jung-Hoon; Koo, Ki-Tae; Capetillo, Joseph; Kim, Jung-Ju; Yoo, Jung-Min; Ben Amara, Heithem; Park, Jung-Chul; Schwarz, Frank; Wikesjö, Ulf M.E. (June 2017). "Periodontal and endodontic pathology delays extraction socket healing in a canine model". Journal of Periodontal & Implant Science. 47 (3): 143–153. doi:10.5051/jpis.2017.47.3.143. ISSN 2093-2278. PMC 5494309. PMID 28680710.
External links
- Max A. Listgarten, University of Pennsylvania and Temple University at http://www.dental.pitt.edu/informatics/periohistology/en/gu0401.htm
- Structure of periodontal tissues in health and disease, Nanci and Bosshardt, Periodontology 2000, Vol. 40, 2006, 11–28 at https://web.archive.org/web/20131109221718/http://www.nancicalcifiedtissuegroup.com/documents/Nanci%202006.pdf
