Supraspinous ligament
The supraspinous ligament, also known as the supraspinal ligament, is a ligament found along the vertebral column.
| Supraspinous ligament | |
|---|---|
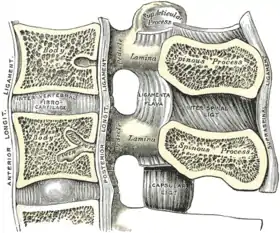 Median sagittal section of two lumbar vertebræ and their ligaments. | |
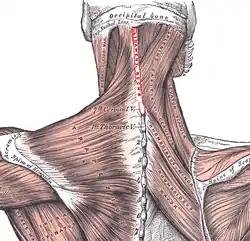 Posterior view of muscles connecting the upper extremity to the vertebral column. Nuchal ligament labeled in red at center. | |
| Details | |
| From | Spinous process of C7 |
| To | Sacrum |
| Identifiers | |
| Latin | ligamentum supraspinale |
| TA98 | A03.2.01.005 |
| TA2 | 1677 |
| FMA | 13425 |
| Anatomical terminology | |
Structure
The supraspinous ligament connects the tips of the spinous processes from the seventh cervical vertebra to the sacrum.[1] Above the seventh cervical vertebra, the supraspinous ligament is continuous with the nuchal ligament.[2]:45
Between the spinous processes it is continuous with the interspinous ligaments.
It is thicker and broader in the lumbar than in the thoracic region, and intimately blended, in both situations, with the neighboring fascia.
The most superficial fibers of this ligament extend over three or four vertebrae; those more deeply seated pass between two or three vertebrae while the deepest connect the spinous processes of neighboring vertebrae.
Function
The supraspinous ligament, along with the posterior longitudinal ligament, interspinous ligaments and ligamentum flavum, help to limit hyperflexion of the vertebral column.
Clinical significance
Lesions to the supraspinous ligament may result in palpable thickening.[3] Ultrasound is effective for detecting lesions.[3][4] A strain injury can also damage the supraspinous ligament.[5]
The supraspinous ligament creates resistance during midline epidural anaesthetics when the needle is being inserted. This increased resistance needs to be taken into account, and is one of the first subcutaneous tissues.[6]
See also
References
- Salinas, Francis (2005-01-01), Benzon, Honorio T.; Raja, Srinivasa N.; Molloy, Robert E.; Liu, Spencer S. (eds.), "Chapter 68 - Spinal Anesthesia", Essentials of Pain Medicine and Regional Anesthesia (Second Edition), Philadelphia: Churchill Livingstone, pp. 566–574, doi:10.1016/b978-0-443-06651-1.50072-1, ISBN 978-0-443-06651-1, retrieved 2020-11-03
- Drake, Richard L.; Vogl, Wayne; Tibbitts, Adam W.M. Mitchell; illustrations by Richard; Richardson, Paul (2005). Gray's anatomy for students (Pbk. ed.). Philadelphia: Elsevier/Churchill Livingstone. ISBN 978-0-443-06612-2.
- Denoix, Jean-Marie; Dyson, Sue J. (2011-01-01), Ross, Mike W.; Dyson, Sue J. (eds.), "Chapter 52 - Thoracolumbar Spine", Diagnosis and Management of Lameness in the Horse (Second Edition), Saint Louis: W.B. Saunders, pp. 592–605, doi:10.1016/b978-1-4160-6069-7.00052-3, ISBN 978-1-4160-6069-7, retrieved 2020-11-03
- Wilson, David A., ed. (2012-01-01), "Back Pain (Thoracolumbar Dysfunction)", Clinical Veterinary Advisor, Saint Louis: W.B. Saunders, pp. 61–63, doi:10.1016/b978-1-4160-9979-6.00039-8, ISBN 978-1-4160-9979-6, retrieved 2020-11-03
- Weaver, Martin P. (2012-01-01), Mair, Tim S; Love, Sandy; Schumacher, Jim; Smith, Roger KW (eds.), "Chapter 18 - Orthopaedics 4. The back and pelvis", Equine Medicine, Surgery and Reproduction (Second Edition), Oxford: W.B. Saunders, pp. 389–397, doi:10.1016/b978-0-7020-2801-4.00018-3, ISBN 978-0-7020-2801-4, retrieved 2020-11-03
- Kim, Kyung-Hoon; Kwon, Jae-Young (2010-01-01), Kim, Daniel H.; Kim, Yong-Chul; Kim, Kyung-Hoon (eds.), "Chapter 5 - Epidural Blocks", Minimally Invasive Percutaneous Spinal Techniques, New York: W.B. Saunders, pp. 111–123, doi:10.1016/b978-0-7020-2913-4.00005-7, ISBN 978-0-7020-2913-4, retrieved 2020-11-03