Urinary catheterization
In urinary catheterization a latex, polyurethane, or silicone tube known as a urinary catheter is inserted into the bladder through the urethra. Catheterization allows urine to drain from the bladder for collection. It may also be used to inject liquids used for treatment or diagnosis of bladder conditions. A clinician, often a nurse, usually performs the procedure, but self-catheterization is also possible. A catheter may be in place for long periods of time (indwelling catheter) or removed after each use (intermittent catheterisation).
| Urinary catheterization | |
|---|---|
 Urinary catheterization with a dummy | |
| ICD-9-CM | 57.94 |
| MeSH | D014546 |
| MedlinePlus | 003981 |
Catheter types
Catheters come in several basic designs:[1]
- A Foley catheter (indwelling urinary catheter) is retained by means of a balloon at the tip that is inflated with sterile water. The balloons typically come in two different sizes: 5 cm3 and 30 cm3. They are commonly made in silicone rubber or natural rubber.
- An intermittent catheter/Robinson catheter is a flexible catheter that is removed after each use. Unlike the Foley catheter, it has no balloon on its tip and therefore cannot stay in place unaided. These can be non-coated or coated (e.g., hydrophilic coated and ready to use).
- A coudé catheter, including Tiemann's catheter, is designed with a curved tip that makes it easier to pass through the curvature of the prostatic urethra.[2]
- A hematuria (or haematuria) catheter is a type of Foley catheter used for Post-TURP hemostasis. This is useful following endoscopic surgical procedures, or in the case of gross hematuria. There are both two-way and three-way hematuria catheters (double and triple lumen).[1]
- A condom catheter can be used by males and carries a lower risk of infection than an indwelling catheter.[3]
Catheter diameters are sized by the French catheter scale (F). The most common sizes are 10 F (3.3mm) to 28 F (9.3mm). The clinician selects a size large enough to allow free flow of urine, and large enough to control leakage of urine around the catheter. A larger size is necessary when the urine is thick, bloody, or contains large amounts of sediment. Larger catheters, however, are more likely to damage the urethra. Some people develop allergies or sensitivities to latex after long-term latex catheter use making it necessary to use silicone or Teflon types.
Evidence does not support an important decrease in the risk of urinary tract infections when silver-alloy catheters are used.[4]
Indications
Common indications for urinary catheterization include acute or chronic urinary retention (which can damage the kidneys), orthopaedic procedures that may limit a patient's movement, the need for accurate monitoring of input and output (such as in an ICU), benign prostatic hyperplasia, incontinence, and the effects of various surgical interventions involving the bladder, prostate or bowel.
Intermittent self-catheterization may be indicated in cases of neurogenic bladder due to damage to the spinal cord or brain. This can be performed by the patient four to six times a day, using a clean technique. Nurses use a sterile technique to perform intermittent catheterization in hospital settings. For patients with neurogenic bladder due to spinal cord injury, intermittent catheterisation (IC) is a standard method for bladder emptying. The technique is safe and effective and results in improved kidney and upper urinary tract status, lessening of vesicoureteral reflux and amelioration of continence.[5] In addition to the clinical benefits, patient quality of life is enhanced by the increased independence and security offered by self-catheterization.[6][7]
- Illustrations
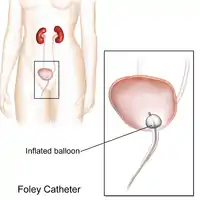 Foley catheter
Foley catheter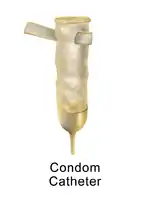 Condom catheter
Condom catheter Male Self-Catheterization
Male Self-Catheterization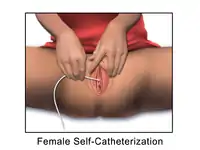 Female Self-Catheterization
Female Self-Catheterization
Catheter maintenance
A catheter that is left in place for more than a short period of time is generally attached to a drainage bag to collect the urine. This also allows for measurement of urine volume. There are three types of drainage bags: The first is a leg bag, a smaller drainage device that attaches by elastic bands to the leg. A leg bag is usually worn during the day, as it fits discreetly under pants or skirts, and is easily emptied into a toilet. The second type of drainage bag is a larger device called a down drain that may be used overnight. This device is hung on a hook under the patient's bed—never placed on the floor, due to the risk of bacterial infection. The third is called a belly bag and is secured around the waist. This bag can be worn at all times. It can be worn under the patient's underwear to provide a totally undetectable look.
During long-term use, the catheter may be left in place all the time, or a patient may be instructed on a procedure for placing a catheter just long enough to empty the bladder and then removing it (known as intermittent self-catheterization). Patients undergoing major surgery are often catheterized and may remain so for some time. The patient may require irrigation of the bladder with sterile saline injected through the catheter to flush out clots or other matter that does not drain.[8]
- Maintenance
 How to properly drain a condom catheter.
How to properly drain a condom catheter. How to properly drain a Foley catheter.
How to properly drain a Foley catheter.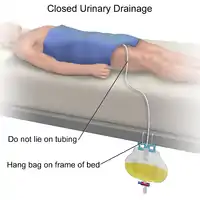 Illustration of a closed urinary drainage method.
Illustration of a closed urinary drainage method. Illustration of how to empty a urinary drainage bag.
Illustration of how to empty a urinary drainage bag.
Complications
Catheterization can have short and long term complications. Generally long-term catheterization carries higher risk of complications. Long-term catheterization carries a significant risk of urinary tract infection. Because of this risk catheterization is a last resort for the management of incontinence where other measures have proved unsuccessful. Other long term complications may include blood infections (sepsis), urethral injury, skin breakdown, bladder stones, and blood in the urine (hematuria). After many years of catheter use, bladder cancer may also develop.
Some people experience bladder spasms with catheterization and may be more common in males. If bladder spasms occur, or there is no urine in the drainage bag, the catheter may be blocked by blood, thick sediment, or a kink in the catheter or drainage tubing. Sometimes spasms are caused by the catheter irritating the bladder, prostate, or penis. Such spasms can be controlled with medication such as butylscopolamine, although most patients eventually adjust to the irritation and the spasms go away.[9]
Preventing infection
Everyday care of catheter and drainage bag is important to reduce the risk of infection.[10] Such precautions include:
- Cleansing the urethral area (the area where the catheter exits body) and the catheter itself.
- Disconnecting drainage bag from catheter only with clean hands
- Disconnecting drainage bag as seldom as possible.
- Keeping drainage bag connector as clean as possible and cleaning the drainage bag periodically.
- Use of a thin catheter where possible to reduce the risk of harming the urethra during insertion.
- Drinking sufficient liquid to produce at least two litres of urine daily
- Sexual activity is very high risk for urinary infections, especially for catheterized women.
There is no clear evidence that any one catheter type or insertion technique is superior than another in preventing infection.[11] In the UK it is generally accepted that cleaning the area surrounding the urethral meatus with 0.9% sodium chloride solution is sufficient for both male and female patients as there is no reliable evidence to suggest that the use of antiseptic agents reduces the risk of urinary tract infection.[12]
Recent developments in the field of the temporary prostatic stent have been viewed as a possible alternative to indwelling catheterization and the infections associated with their use.[13]
History
Ancient Egyptian and Roman physicians have been described using reeds as urinary catheters to overcome blockages, and catheterisation to relieve urinary retention has also been described in ancient Indian and Chinese texts.[14]
References
- Hanno PM, Wein AJ, Malkowicz SB (2001). Clinical manual of urology.. McGraw-Hill Professional. p. 78.
- Elroy D. Kursh (1987). Urology: Problems in Primary Care. Medical Economics Books. ISBN 9780874894196.
- Black MA (1994). Medical nursing (2nd ed.). Springhouse, Pa.: Springhouse Corp. p. 97. ISBN 0-87434-738-6. LCCN 94035389.
- Lam TB, Omar MI, Fisher E, Gillies K, MacLennan S (September 2014). "Types of indwelling urethral catheters for short-term catheterisation in hospitalised adults". Cochrane Database Syst Rev (9): CD004013. doi:10.1002/14651858.CD004013.pub4. PMID 25248140.
- Hedlund H, Hjelmås K, Jonsson O, Klarskov P, Talja M (February 2001). "Hydrophilic versus non-coated catheters for intermittent catheterization". Scand. J. Urol. Nephrol. 35 (1): 49–53. doi:10.1080/00365590151030822. PMID 11291688.
- Lapides J, Diokno AC, Silber SJ, Lowe BS (March 1972). "Clean, intermittent self-catheterization in the treatment of urinary tract disease". J. Urol. 107 (3): 458–61. doi:10.1016/s0022-5347(17)61055-3. PMID 5010715.
- Winder A (2002). "Intermittent self-catheterisation". Nurs Times. 98 (48): 50. PMID 12501532.
- Best practices : evidence-based nursing procedures (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. 2007. ISBN 978-1-58255-532-4. LCCN 2006012245.
- "Urinary catheters". MedlinePlus, the National Institutes of Health's Web site. 2010-03-09. Retrieved 2010-12-01.
- "Care for your catheter". healthline. Retrieved 2008-09-12.
- Prieto J, Murphy CL, Moore KN, Fader M (September 2014). "Intermittent catheterisation for long-term bladder management" (PDF). Cochrane Database Syst Rev (9): CD006008. doi:10.1002/14651858.CD006008.pub3. PMID 25208303. (Retracted, see doi:10.1002/14651858.cd006008.pub4. If this is an intentional citation to a retracted paper, please replace
{{Retracted}}with{{Retracted|intentional=yes}}.) - Dougherty Lisa; Lister Sara (2011-08-15). The Royal Marsden Hospital Manual of Clinical Nursing Procedures. John Wiley & Sons. ISBN 978-1-4443-3509-5.
- Shore ND, Dineen MK, Saslawsky MJ, Lumerman JH, Corica AP (March 2007). "A temporary intraurethral prostatic stent relieves prostatic obstruction following transurethral microwave thermotherapy". J. Urol. 177 (3): 1040–6. doi:10.1016/j.juro.2006.10.059. PMID 17296408.
- Nahon, I; Waddington, G; Dorey, G; Adams, R (2011). "The history of urologic surgery: from reeds to robotics". Urologic nursing. 31 (3): 173–80. PMID 21805756.
External links
- Female urinary catherization, Merck Manual Professional Edition
- Male urinary catherization, Merck Manual Professional Edition