Contact tracing
In public health, contact tracing is the process of identification of persons who may have come into contact with an infected person ("contacts") and subsequent collection of further information about these contacts. By tracing the contacts of infected individuals, testing them for infection, isolating or treating the infected and tracing their contacts in turn, public health aims to reduce infections in the population. Diseases for which contact tracing is commonly performed include tuberculosis, vaccine-preventable infections like measles, sexually transmitted infections (including HIV), blood-borne infections, Ebola, some serious bacterial infections, and novel virus infections (e.g. SARS-CoV, H1N1, and SARS-CoV-2). The goals of contact tracing are:
- To interrupt ongoing transmission and reduce the spread of an infection
- To alert contacts to the possibility of infection and offer preventive services or prophylactic care
- To offer diagnosis, counseling and treatment to already infected individuals
- If the infection is treatable, to help prevent reinfection of the originally infected patient
- To learn about the epidemiology of a disease in a particular population

Contact tracing has been a pillar of communicable disease control in public health for decades. The eradication of smallpox, for example, was achieved not by universal immunization, but by exhaustive contact tracing to find all infected persons.[1] This was followed by isolation of infected individuals and immunization of the surrounding community and contacts at-risk of contracting smallpox.
In cases of diseases of uncertain infectious potential, contact tracing is also sometimes performed to learn about disease characteristics, including infectiousness. Contact tracing is not always the most efficient method of addressing infectious disease. In areas of high disease prevalence, screening or focused testing may be more cost-effective.
Partner notification, also called partner care, is a subset of contact tracing aimed specifically at informing sexual partners of an infected person and addressing their health needs.
Steps in contact tracing

Contact tracing generally involves the following steps:
- An individual is identified as having a communicable disease (often called the index case). This case may be reported to public health or managed by the primary health care provider.
- The index case is interviewed to learn about their movements, whom they have been in close contact with or who their sexual partners have been.
- Depending on the disease and the context of the infection, family members, health care providers, and anyone else who may have knowledge of the case's contacts may also be interviewed.
- Once contacts are identified, public health workers contact them to offer counseling, screening, prophylaxis, and/or treatment.
- Contacts may be isolated (e.g. required to remain at home) or excluded (e.g. prohibited from attending a particular location, like a school) if deemed necessary for disease control.
- If contacts are not individually identifiable (e.g. members of the public who attended the same location), broader communications may be issued, like media advisories.
Although contact tracing can be enhanced by letting patients provide information, medication, and referrals to their contacts, evidence demonstrates that direct public health involvement in notification is most effective.[2]
Relevance of contacts
.jpg.webp)

The types of contacts that are relevant for public health management vary with the communicable disease because of differing modes of transmission. For sexually transmitted infections, sexual contacts of the index case are relevant, as well as any babies born to the index case. For blood-borne infections, blood transfusion recipients, contacts who shared a needle, and anyone else who could have been exposed to the blood of the index case are relevant. For pulmonary tuberculosis, people living in the same household or spending a significant amount of time in the same room as the index case are relevant.[3]
Outbreaks
Although contact tracing is most commonly used for control of diseases, it is also a critical tool for investigating new diseases or unusual outbreaks. For example, as was the case with SARS, contact tracing can be used to determine if probable cases are linked to known cases of the disease, and to determine if secondary transmission is taking place in a particular community.[4]
Contact tracing has also been initiated among flight passengers during the containment phase of larger pandemics, such as the 2009 pandemic H1NI influenza. However, there continue to be large challenges in achieving the goals of contact tracing during such chaotic events.[5] Development of better guidelines and strategies for pandemic contact tracing continues.[6]
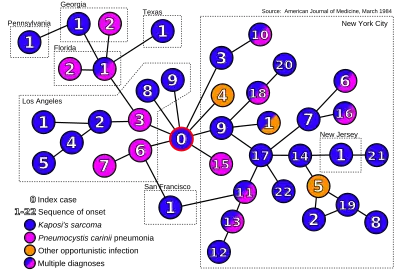
Identification of etiology
Contact tracing can help identify the etiology of a disease outbreak.[8] In 1984, contact tracing provided the first direct evidence that AIDS may be spread by an infectious agent during sexual contacts.[9][7] The infective agent has since been identified as HIV.[10]
Backward and forward tracing
Backward (or reverse or retrospective) tracing seeks to establish the source of an infection, by looking for contacts before infection.
Forward tracing is the process of looking for contacts after infection, so as to prevent further disease spread.
Backward contact tracing has been advised as a way of finding people with tuberculosis who are missed by routine health services.[11]
For epidemics with high heterogeneity in infectiousness, it might make sense, depending on local contact tracing capacity, to adopt a hybrid strategy of "regular" forward contact tracing combined with contact tracing backwards in time to find the source of infection of the index case itself. Indeed, due to a statistical effect similar to the friendship paradox, the index case is expected to have a much higher number of infected "offspring".
During the COVID-19 pandemic, the adoption by Japan in early spring 2020 of an approach focusing on backward contact tracing was hailed as successful,[12][13][14][15] and other countries which managed to keep the epidemic under control, such as South Korea[16] and Uruguay,[17][18] are said to have also used the approach.[19] There is mounting theoretical support for the adoption of this strategy in the context of COVID, if local resources allow.[20][21][22][23] Journalist and author Laurie Garrett pointed out in late October 2020, however, that the amount of the virus in the U.S. is now so large that no health departments has the resources to contact and trace.[24]
In September 2020, science writer and sociologist Zeynep Tufekci wrote a long piece in The Atlantic on the lack of attention by many public health authorities to the index of dispersion of the SARS-CoV-2 virus and its implications for contact tracing.[25]
In October 2020, German virologist Christian Drosten called on all citizens of Germany to maintain a diary of their close contacts, in order to facilitate backward tracing and thus help contact tracing teams to find disease clusters.[26]
Technology
Case management
Case management software is often used by contact tracers to maintain records of cases and contact tracing activities.[27] This is typically a cloud database that may have specialized features such as the ability to use SMS or email directly within the software to notify people believed to have been in close contact with someone carrying an infectious disease.[28] Vendors offering contact tracing case management software include Salesforce, Microsoft and Watkyn.[29][30][31]
Mobile phones
Smartphones can provide proximity information useful for contact tracing using GPS, Bluetooth or Wifi signals.[32] Facebook Labs patented the use of Bluetooth on smartphones for this in 2018.[33] On 10 April 2020, Apple and Google, who account for most of the world's mobile operating systems, announced COVID-19 apps for iOS and Android.[34] Relying on Bluetooth Low Energy (BLE) wireless radio signals for proximity information,[35] the new tools would warn people that they had been in contact with who are infected by SARS-CoV-2.[34]
Protocols
Various protocols, such as Pan-European Privacy-Preserving Proximity Tracing (PEPP-PT),[36] Whisper Tracing Protocol,[37] Decentralized Privacy-Preserving Proximity Tracing (DP-PPT/DP-3T),[38][39] TCN Protocol, Contact Event Numbers (CEN), Privacy Sensitive Protocols And Mechanisms for Mobile Contact Tracing (PACT)[40] and others, are being discussed to preserve user privacy.
The DP-3T and TCN protocols are currently used by Switzerland, Austria, Estonia, Finland, and Italy. While the UK, France, Australia, New Zealand, and Singapore use PEPP-PT or BlueTrace based systems.[41]
Ethical and legal issues
Challenges with contact tracing can arise related to issues of medical privacy and confidentiality. Public health practitioners often are mandated reporters, required to act to contain a communicable disease within a broader population and also ethically obliged to warn individuals of their exposure. Simultaneously, infected individuals have a recognized right to medical confidentiality. Public health teams typically disclose the minimum amount of information required to achieve the objectives of contact tracing. For example, contacts are only told that they have been exposed to a particular infection, but not informed of the person who was the source of the exposure.[2]
Some activists and health care providers have expressed concerns that contact tracing may discourage persons from seeking medical treatment. for fear of loss of confidentiality and subsequent stigma, discrimination, or abuse. This has been of particular concern regarding contact tracing for HIV. Public health officials have recognized that the goals of contact tracing must be balanced with the maintenance of trust with vulnerable populations and sensitivity to individual situations.[2]
See also
References
- Scutchfield, F. Douglas (2003). Principles of public health practice. Clifton Park, New York: Delmar Learning. p. 71. ISBN 0-76682843-3.
- Ontario Provincial Infectious Diseases Advisory Committee (2009). Sexually transmitted infections best practices and contact tracing best practice recommendations. Toronto, Canada: Ontario Ministry of Health and Long-Term Care. ISBN 978-1-42497946-2.
- Australasian Contact Tracing Manual. Darlinghurst, New South Wales, Australia: Australasian Society for HIV Medicine. 2010. ISBN 978-1-920773-95-3.
- "Severe Acute Respiratory Syndrome (SARS) – multi-country outbreak". Global Alert and Response. WHO. Retrieved 2013-05-28.
- Swaan, Corien M.; Appels, Rolf; Kretzschmar, Mirjam E. E.; van Steenbergen, Jim E. (2011-12-28). "Timeliness of contact tracing among flight passengers for influenza A/H1N1 2009". BMC Infectious Diseases. 11 (1): 355. doi:10.1186/1471-2334-11-355. ISSN 1471-2334. PMC 3265549. PMID 22204494.
- Ferretti, Luca; Wymant, Chris; Kendall, Michelle; Zhao, Lele; Nurtay, Anel; Abeler-Dörner, Lucie; Parker, Michael; Bonsall, David; Fraser, Christophe (2020-03-31). "Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing". Science. 368 (6491): eabb6936. doi:10.1126/science.abb6936. ISSN 0036-8075. PMC 7164555. PMID 32234805.
- Auerbach, David M.; Darrow, William W.; Jaffe, Harold W.; Curran, James W. (1984). "Cluster of cases of the acquired immune deficiency syndrome. Patients linked by sexual contact". The American Journal of Medicine. 76 (3): 487–92. doi:10.1016/0002-9343(84)90668-5. PMID 6608269.
- Riley, Steven; Fraser, Christophe; Donnelly, Christl A.; Ghani, Azra C.; Abu-Raddad, Laith J.; Hedley, Anthony J.; Leung, Gabriel M.; Ho, Lai-Ming; Lam, Tai-Hing; Thach, Thuan Q.; Chau, Patsy (2003-06-20). "Transmission Dynamics of the Etiological Agent of SARS in Hong Kong: Impact of Public Health Interventions". Science. 300 (5627): 1961–1966. doi:10.1126/science.1086478. ISSN 0036-8075. PMID 12766206.
- Klovdahl, Alden S. (1985-01-01). "Social networks and the spread of infectious diseases: The AIDS example". Social Science & Medicine. 21 (11): 1203–1216. doi:10.1016/0277-9536(85)90269-2. ISSN 0277-9536.
- Blattner, W.; Gallo, R. C.; Temin, H. M. (1988-07-29). "HIV causes AIDS". Science. 241 (4865): 515–515. doi:10.1126/science.3399881. ISSN 0036-8075. PMID 3399881.
- "StopTB Field guide 6: Using Contact Investigation to Improve TB Case Detection" (PDF). Stop TB Partnership. 2018.
- "The 'Japan model' that tackled coronavirus". Financial Times.
- Nishimura, Yasutoshi (2020-07-07). "Opinion | How Japan Beat Coronavirus Without Lockdowns". The Wall Street Journal. ISSN 0099-9660. Retrieved 2020-10-19.
- Oshitani, Hitoshi; The Experts Members of The National COVID-19 Cluster Taskforce at Ministry of Health, Labour and Welfare, Japan (2020). "Cluster-based approach to Coronavirus Disease 2019 (COVID-19) response in Japan—February–April 2020". Japanese Journal of Infectious Diseases. doi:10.7883/yoken.JJID.2020.363. ISSN 1344-6304. S2CID 220310375.CS1 maint: multiple names: authors list (link)
- "[Addendum] Japan's Cluster-based Approach" (PDF). Ministry of Health, Labour and Welfare. 2020-05-28.
- Lee, Seung Won; Yuh, Woon Tak; Yang, Jee Myung; Cho, Yoon-Sik; Yoo, In Kyung; Koh, Hyun Yong; Marshall, Dominic; Oh, Donghwan; Ha, Eun Kyo; Han, Man Yong; Yon, Dong Keon (2020-08-25). "Nationwide Results of COVID-19 Contact Tracing in South Korea: Individual Participant Data From an Epidemiological Survey". JMIR Medical Informatics. 8 (8): e20992. doi:10.2196/20992. ISSN 2291-9694. PMC 7470235. PMID 32784189.
- Taylor, Luke (2020-09-18). "Uruguay is winning against covid-19. This is how". BMJ. 370: m3575. doi:10.1136/bmj.m3575. ISSN 1756-1833. PMID 32948599. S2CID 221778076.
- Moreno, Pilar; Moratorio, Gonzalo Andres; Iraola, Gregorio; Fajardo, Alvaro; Aldunate, Fabian; Pereira, Marianoel; Perbolianachis, Paula; Costabile, Alicia; Lopez-Tort, Fernando; Simon, Diego; Salazar, Cecilia (2020-07-27). "An effective COVID-19 response in South America: the Uruguayan Conundrum". MedRxiv (Preprint): 2020.07.24.20161802. doi:10.1101/2020.07.24.20161802. S2CID 220793010.
- Crozier, Alex; Mckee, Martin; Rajan, Selina (2020-10-15). "Fixing England's COVID-19 response: learning from international experience". Journal of the Royal Society of Medicine. 113 (11): 422–427. doi:10.1177/0141076820965533. PMC 7686527. PMID 33058751. S2CID 222839822.
- Bradshaw, William J.; Alley, Ethan C.; Huggins, Jonathan H.; Lloyd, Alun L.; Esvelt, Kevin M. (2020). "Bidirectional contact tracing dramatically improves COVID-19 control". doi:10.1101/2020.05.06.20093369. S2CID 218561613. Cite journal requires
|journal=(help) - Endo, Akira; Leclerc, Quentin J.; Knight, Gwenan M.; Medley, Graham F.; Atkins, Katherine E.; Funk, Sebastian; Kucharski, Adam J.; Kucharski, A. J. (2020). "Implication of backward contact tracing in the presence of overdispersed transmission in COVID-19 outbreaks". Wellcome Open Research. 5: 239. doi:10.12688/WELLCOMEOPENRES.16344.1. PMC 7610176. PMID 33154980.
- Lambert, Amaury (2020). "A mathematical assessment of the efficiency of quarantining and contact tracing in curbing the COVID-19 epidemic". doi:10.1101/2020.05.04.20091009. S2CID 218964036. Cite journal requires
|journal=(help) - Kojaku, Sadamori; Hébert-Dufresne, Laurent; Mones, Enys; Lehmann, Sune; Ahn, Yong-Yeol (2020). "The effectiveness of backward contact tracing in networks". arXiv:2005.02362 [q-bio.PE].
- https://www.msnbc.com/deadline-white-house/watch/laurie-garrett-the-amount-of-virus-in-the-u-s-is-so-large-that-no-one-has-health-departments-large-enough-to-do-contact-tracing-94794821630?cid=sm_npd_ms_tw_ma
- Tufekci, Zeynep (2020-09-30). "This Overlooked Variable Is the Key to the Pandemic". The Atlantic. Retrieved 2020-10-19.
- Scharpenberg, Jan (2020-10-13). "Drosten fordert Corona-Tagebuch zur besseren Kontaktnachverfolgung". www.waz.de (in German). Retrieved 2020-10-21.
- "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 2020-06-17. Retrieved 2020-07-18.
- "ContactPath by Watkyn Launches to Reduce the Spread of COVID-19". prnewswire.com. Retrieved 2020-07-14.
- "Marc Benioff says 35 states are now using Salesforce's contact tracing technology for coronavirus". cnbc.com. Retrieved 2020-07-14.
- "Greater Manchester plans case management for contact tracing". ukauthority.com. Retrieved 2020-07-14.
- "Contact Tracing Platform Developed in QuickBase". insightfromanalytics.com. Retrieved 2020-07-14.
- "Privacy-preserving controls for sharing mHealth data - ProQuest". search.proquest.com. Retrieved 2020-07-01.
- , "Proximity-based trust", issued 2018-01-16
- Sherr, Ian; Nieva, Richard (2020-04-10). "Apple and Google are building coronavirus tracking tech into iOS and Android – The two companies are working together, representing most of the phones used around the world". CNET. Archived from the original on 2020-04-10. Retrieved 2020-04-10.
- "Contact Tracing – Bluetooth Specification" (PDF). covid19-static.cdn-apple.com (Preliminary ed.). 2020-04-10. Archived (PDF) from the original on 2020-04-10. Retrieved 2020-04-10.
- Lomas, Natasha (2020-04-01). "An EU coalition of techies is backing a 'privacy-preserving' standard for COVID-19 contacts tracing". TechCrunch. Archived from the original on 2020-04-10. Retrieved 2020-04-11.
- "Latest weapon in tracing and tracking coronavirus infections: your smartphone". SFChronicle.com. 2020-04-23. Retrieved 2020-05-06.
- Lomas, Natasha (2020-04-06). "EU privacy experts push a decentralized approach to COVID-19 contacts tracing". TechCrunch. Archived from the original on 2020-04-10. Retrieved 2020-04-11.
- https://github.com/DP-3T/documents/blob/master/DP3T%20White%20Paper.pdf Github.com
- Chan, Justin; Gollakota, Shyam; Horvitz, Eric; Jaeger, Joseph; Kakade, Sham; Kohno, Tadayoshi; Langford, John; Larson, Jonathan; Singanamalla, Sudheesh; Sunshine, Jacob; Tessaro, Stefano (2020-04-07). "PACT: Privacy Sensitive Protocols And Mechanisms for Mobile Contact Tracing". arXiv:2004.03544v1 [cs.CR].
- "Contact tracing apps: How to fight COVID-19 and protect your privacy". ProtonMail Blog. 2020-05-15. Retrieved 2020-07-02.