Tuberculosis
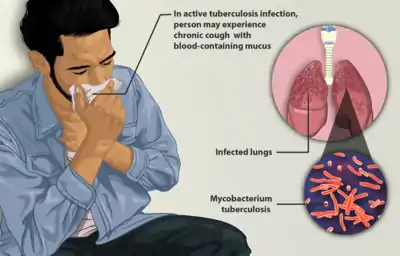
Tuberculosis (TB) is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria.[1] Tuberculosis generally affects the lungs, but can also affect other parts of the body.[1] Most infections show no symptoms, in which case it is known as latent tuberculosis.[1] About 10% of latent infections progress to active disease which, if left untreated, kills about half of those affected.[1] The classic symptoms of active TB are a chronic cough with blood-containing mucus, fever, night sweats, and weight loss.[1] It was historically called consumption due to the weight loss.[8] Infection of other organs can cause a wide range of symptoms.[9]
| Tuberculosis | |
|---|---|
| Other names | Phthisis, phthisis pulmonalis, consumption |
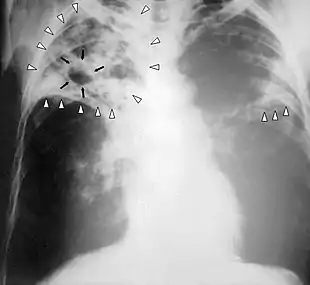 | |
| Chest X-ray of a person with advanced tuberculosis: Infection in both lungs is marked by white arrow-heads, and the formation of a cavity is marked by black arrows. | |
| Specialty | Infectious disease, pulmonology |
| Symptoms | Chronic cough, fever, cough with bloody mucus, weight loss[1] |
| Causes | Mycobacterium tuberculosis[1] |
| Risk factors | Smoking, HIV/AIDS[1] |
| Diagnostic method | CXR, culture, tuberculin skin test[1] |
| Differential diagnosis | Pneumonia, histoplasmosis, sarcoidosis, coccidioidomycosis[2] |
| Prevention | Screening those at high risk, treatment of those infected, vaccination with bacillus Calmette-Guérin (BCG)[3][4][5] |
| Treatment | Antibiotics[1] |
| Frequency | 25% of people (latent TB)[6] |
| Deaths | 1.5 million (2018)[7] |
Tuberculosis is spread from one person to the next through the air when people who have active TB in their lungs cough, spit, speak, or sneeze.[1][10] People with latent TB do not spread the disease.[1] Active infection occurs more often in people with HIV/AIDS and in those who smoke.[1] Diagnosis of active TB is based on chest X-rays, as well as microscopic examination and culture of body fluids.[11] Diagnosis of latent TB relies on the tuberculin skin test (TST) or blood tests.[11]
Prevention of TB involves screening those at high risk, early detection and treatment of cases, and vaccination with the bacillus Calmette-Guérin (BCG) vaccine.[3][4][5] Those at high risk include household, workplace, and social contacts of people with active TB.[4] Treatment requires the use of multiple antibiotics over a long period of time.[1] Antibiotic resistance is a growing problem with increasing rates of multiple drug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB).[1]
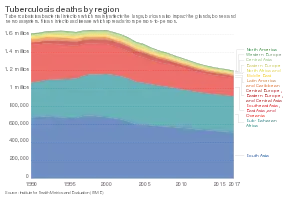
As of 2018 one quarter of the world's population is thought to have latent infection with TB.[6] New infections occur in about 1% of the population each year.[12] In 2018, there were more than 10 million cases of active TB which resulted in 1.5 million deaths.[7] This makes it the number one cause of death from an infectious disease.[13] As of 2018, most TB cases occurred in the regions of South-East Asia (44%), Africa (24%) and the Western Pacific (18%), with more than 50% of cases being diagnosed in eight countries: India (27%), China (9%), Indonesia (8%), the Philippines (6%), Pakistan (6%), Nigeria (4%) and Bangladesh (4%).[13] The number of new cases each year has decreased since 2000.[1] About 80% of people in many Asian and African countries test positive while 5–10% of people in the United States population test positive by the tuberculin test.[14] Tuberculosis has been present in humans since ancient times.[15]
Signs and symptoms
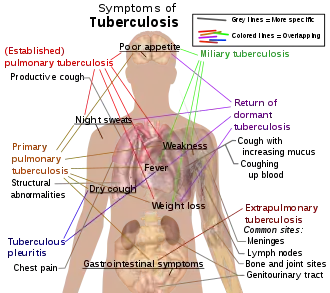
Tuberculosis may infect any part of the body, but most commonly occurs in the lungs (known as pulmonary tuberculosis).[9] Extrapulmonary TB occurs when tuberculosis develops outside of the lungs, although extrapulmonary TB may coexist with pulmonary TB.[9]
General signs and symptoms include fever, chills, night sweats, loss of appetite, weight loss, and fatigue.[9] Significant nail clubbing may also occur.[17]
Pulmonary
If a tuberculosis infection does become active, it most commonly involves the lungs (in about 90% of cases).[15][18] Symptoms may include chest pain and a prolonged cough producing sputum. About 25% of people may not have any symptoms (i.e. they remain "asymptomatic").[15] Occasionally, people may cough up blood in small amounts, and in very rare cases, the infection may erode into the pulmonary artery or a Rasmussen's aneurysm, resulting in massive bleeding.[9][19] Tuberculosis may become a chronic illness and cause extensive scarring in the upper lobes of the lungs. The upper lung lobes are more frequently affected by tuberculosis than the lower ones.[9] The reason for this difference is not clear.[14] It may be due to either better air flow,[14] or poor lymph drainage within the upper lungs.[9]
Extrapulmonary
In 15–20% of active cases, the infection spreads outside the lungs, causing other kinds of TB.[20] These are collectively denoted as "extrapulmonary tuberculosis".[21] Extrapulmonary TB occurs more commonly in people with a weakened immune system and young children. In those with HIV, this occurs in more than 50% of cases.[21] Notable extrapulmonary infection sites include the pleura (in tuberculous pleurisy), the central nervous system (in tuberculous meningitis), the lymphatic system (in scrofula of the neck), the genitourinary system (in urogenital tuberculosis), and the bones and joints (in Pott disease of the spine), among others. A potentially more serious, widespread form of TB is called "disseminated tuberculosis", it is also known as miliary tuberculosis.[9] Miliary TB currently makes up about 10% of extrapulmonary cases.[22]
Causes
Mycobacteria
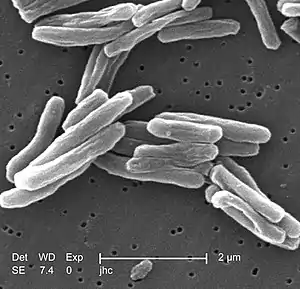
The main cause of TB is Mycobacterium tuberculosis (MTB), a small, aerobic, nonmotile bacillus.[9] The high lipid content of this pathogen accounts for many of its unique clinical characteristics.[23] It divides every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour.[24] Mycobacteria have an outer membrane lipid bilayer.[25] If a Gram stain is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a result of the high lipid and mycolic acid content of its cell wall.[26] MTB can withstand weak disinfectants and survive in a dry state for weeks. In nature, the bacterium can grow only within the cells of a host organism, but M. tuberculosis can be cultured in the laboratory.[27]
Using histological stains on expectorated samples from phlegm (also called "sputum"), scientists can identify MTB under a microscope. Since MTB retains certain stains even after being treated with acidic solution, it is classified as an acid-fast bacillus.[14][26] The most common acid-fast staining techniques are the Ziehl–Neelsen stain[28] and the Kinyoun stain, which dye acid-fast bacilli a bright red that stands out against a blue background.[29] Auramine-rhodamine staining[30] and fluorescence microscopy[31] are also used.
The M. tuberculosis complex (MTBC) includes four other TB-causing mycobacteria: M. bovis, M. africanum, M. canetti, and M. microti.[32] M. africanum is not widespread, but it is a significant cause of tuberculosis in parts of Africa.[33][34] M. bovis was once a common cause of tuberculosis, but the introduction of pasteurized milk has almost completely eliminated this as a public health problem in developed countries.[14][35] M. canetti is rare and seems to be limited to the Horn of Africa, although a few cases have been seen in African emigrants.[36][37] M. microti is also rare and is seen almost only in immunodeficient people, although its prevalence may be significantly underestimated.[38]
Other known pathogenic mycobacteria include M. leprae, M. avium, and M. kansasii. The latter two species are classified as "nontuberculous mycobacteria" (NTM). NTM cause neither TB nor leprosy, but they do cause lung diseases that resemble TB.[39]
Transmission
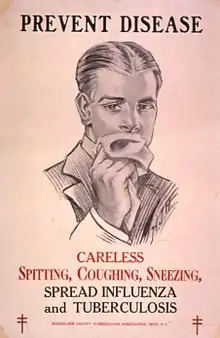
When people with active pulmonary TB cough, sneeze, speak, sing, or spit, they expel infectious aerosol droplets 0.5 to 5.0 µm in diameter. A single sneeze can release up to 40,000 droplets.[40] Each one of these droplets may transmit the disease, since the infectious dose of tuberculosis is very small (the inhalation of fewer than 10 bacteria may cause an infection).[41]
Risk of transmission
People with prolonged, frequent, or close contact with people with TB are at particularly high risk of becoming infected, with an estimated 22% infection rate.[42] A person with active but untreated tuberculosis may infect 10–15 (or more) other people per year.[43] Transmission should occur from only people with active TB – those with latent infection are not thought to be contagious.[14] The probability of transmission from one person to another depends upon several factors, including the number of infectious droplets expelled by the carrier, the effectiveness of ventilation, the duration of exposure, the virulence of the M. tuberculosis strain, the level of immunity in the uninfected person, and others.[44] The cascade of person-to-person spread can be circumvented by segregating those with active ("overt") TB and putting them on anti-TB drug regimens. After about two weeks of effective treatment, subjects with nonresistant active infections generally do not remain contagious to others.[42] If someone does become infected, it typically takes three to four weeks before the newly infected person becomes infectious enough to transmit the disease to others.[45]
Risk factors
A number of factors make individuals more susceptible to TB infection and/or disease.[46]
Active disease risk
The most important risk factor globally is HIV; 13% of those with TB are also infected with HIV.[47] This is a particular problem in sub-Saharan Africa, where rates of HIV are high.[48][49] Of those without HIV who are infected with tuberculosis, about 5–10% develop active disease during their lifetimes;[17] in contrast, 30% of those co-infected with HIV develop the active disease.[17]
Use of certain medications, such as corticosteroids and infliximab (an anti-αTNF monoclonal antibody), is another important risk factor, especially in the developed world.[15]
Other risk factors include: alcoholism,[15] diabetes mellitus (3-fold increased risk),[50] silicosis (30-fold increased risk),[51] tobacco smoking (2-fold increased risk),[52] indoor air pollution, malnutrition, young age,[46] recently acquired TB infection, recreational drug use, severe kidney disease, low body weight, organ transplant, head and neck cancer,[53] and genetic susceptibility[54] (of which the overall importance remains undefined[15]).
Infection susceptibility
Tobacco smoking increases the risk of infections (in addition to increasing the risk of active disease and death). Additional factors increasing infection susceptibility include: young age (children).[46]
Pathogenesis
About 90% of those infected with M. tuberculosis have asymptomatic, latent TB infections (sometimes called LTBI),[55] with only a 10% lifetime chance that the latent infection will progress to overt, active tuberculous disease.[56] In those with HIV, the risk of developing active TB increases to nearly 10% a year.[56] If effective treatment is not given, the death rate for active TB cases is up to 66%.[43]
TB infection begins when the mycobacteria reach the alveolar air sacs of the lungs, where they invade and replicate within endosomes of alveolar macrophages.[14][57][58] Macrophages identify the bacterium as foreign and attempt to eliminate it by phagocytosis. During this process, the bacterium is enveloped by the macrophage and stored temporarily in a membrane-bound vesicle called a phagosome. The phagosome then combines with a lysosome to create a phagolysosome. In the phagolysosome, the cell attempts to use reactive oxygen species and acid to kill the bacterium. However, M. tuberculosis has a thick, waxy mycolic acid capsule that protects it from these toxic substances. M. tuberculosis is able to reproduce inside the macrophage and will eventually kill the immune cell.
The primary site of infection in the lungs, known as the "Ghon focus", is generally located in either the upper part of the lower lobe, or the lower part of the upper lobe.[14] Tuberculosis of the lungs may also occur via infection from the blood stream. This is known as a Simon focus and is typically found in the top of the lung.[59] This hematogenous transmission can also spread infection to more distant sites, such as peripheral lymph nodes, the kidneys, the brain, and the bones.[14][60] All parts of the body can be affected by the disease, though for unknown reasons it rarely affects the heart, skeletal muscles, pancreas, or thyroid.[61]
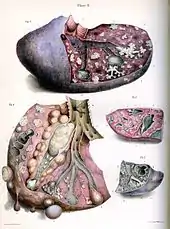
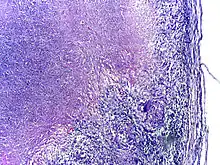
Tuberculosis is classified as one of the granulomatous inflammatory diseases. Macrophages, epithelioid cells, T lymphocytes, B lymphocytes, and fibroblasts aggregate to form granulomas, with lymphocytes surrounding the infected macrophages. When other macrophages attack the infected macrophage, they fuse together to form a giant multinucleated cell in the alveolar lumen. The granuloma may prevent dissemination of the mycobacteria and provide a local environment for interaction of cells of the immune system.[63] However, more recent evidence suggests that the bacteria use the granulomas to avoid destruction by the host's immune system. Macrophages and dendritic cells in the granulomas are unable to present antigen to lymphocytes; thus the immune response is suppressed.[64] Bacteria inside the granuloma can become dormant, resulting in latent infection. Another feature of the granulomas is the development of abnormal cell death (necrosis) in the center of tubercles. To the naked eye, this has the texture of soft, white cheese and is termed caseous necrosis.[63]
If TB bacteria gain entry to the blood stream from an area of damaged tissue, they can spread throughout the body and set up many foci of infection, all appearing as tiny, white tubercles in the tissues.[65] This severe form of TB disease, most common in young children and those with HIV, is called miliary tuberculosis.[66] People with this disseminated TB have a high fatality rate even with treatment (about 30%).[22][67]
In many people, the infection waxes and wanes. Tissue destruction and necrosis are often balanced by healing and fibrosis.[63] Affected tissue is replaced by scarring and cavities filled with caseous necrotic material. During active disease, some of these cavities are joined to the air passages (bronchi) and this material can be coughed up. It contains living bacteria, and thus can spread the infection. Treatment with appropriate antibiotics kills bacteria and allows healing to take place. Upon cure, affected areas are eventually replaced by scar tissue.[63]
Diagnosis

Active tuberculosis
Diagnosing active tuberculosis based only on signs and symptoms is difficult,[68] as is diagnosing the disease in those who have a weakened immune system.[69] A diagnosis of TB should, however, be considered in those with signs of lung disease or constitutional symptoms lasting longer than two weeks.[69] A chest X-ray and multiple sputum cultures for acid-fast bacilli are typically part of the initial evaluation.[69] Interferon-γ release assays and tuberculin skin tests are of little use in most of the developing world.[70][71] Interferon gamma release assays (IGRA) have similar limitations in those with HIV.[71][72]
A definitive diagnosis of TB is made by identifying M. tuberculosis in a clinical sample (e.g., sputum, pus, or a tissue biopsy). However, the difficult culture process for this slow-growing organism can take two to six weeks for blood or sputum culture.[73] Thus, treatment is often begun before cultures are confirmed.[74]
Nucleic acid amplification tests and adenosine deaminase testing may allow rapid diagnosis of TB.[68] These tests, however, are not routinely recommended, as they rarely alter how a person is treated.[74] Blood tests to detect antibodies are not specific or sensitive, so they are not recommended.[75]
Latent tuberculosis
The Mantoux tuberculin skin test is often used to screen people at high risk for TB.[69] Those who have been previously immunized with the Bacille Calmette-Guerin vaccine may have a false-positive test result.[76] The test may be falsely negative in those with sarcoidosis, Hodgkin's lymphoma, malnutrition, and most notably, active tuberculosis.[14] Interferon gamma release assays, on a blood sample, are recommended in those who are positive to the Mantoux test.[74] These are not affected by immunization or most environmental mycobacteria, so they generate fewer false-positive results.[77] However, they are affected by M. szulgai, M. marinum, and M. kansasii.[78] IGRAs may increase sensitivity when used in addition to the skin test, but may be less sensitive than the skin test when used alone.[79]
The US Preventive Services Task Force (USPSTF) has recommended screening people who are at high risk for latent tuberculosis with either tuberculin skin tests or interferon-gamma release assays.[80] While some have recommend testing health care workers, evidence of benefit for this is poor as of 2019.[81] The Centers for Disease Control and Prevention (CDC) stopped recommending yearly testing of health care workers without known exposure in 2019.[82]
Prevention
.jpg.webp)
Tuberculosis prevention and control efforts rely primarily on the vaccination of infants and the detection and appropriate treatment of active cases.[15] The World Health Organization (WHO) has achieved some success with improved treatment regimens, and a small decrease in case numbers.[15]
Vaccines
The only available vaccine as of 2011 is Bacillus Calmette-Guérin (BCG).[83] In children it decreases the risk of getting the infection by 20% and the risk of infection turning into active disease by nearly 60%.[84]
It is the most widely used vaccine worldwide, with more than 90% of all children being vaccinated.[15] The immunity it induces decreases after about ten years.[15] As tuberculosis is uncommon in most of Canada, Western Europe, and the United States, BCG is administered to only those people at high risk.[85][86][87] Part of the reasoning against the use of the vaccine is that it makes the tuberculin skin test falsely positive, reducing the test's usefulness as a screening tool.[87] Several vaccines are being developed.[15]
Intradermal MVA85A Vaccine in addition to BCG injection is not effective in preventing tuberculosis.[88]
Public health
The World Health Organization (WHO) declared TB a "global health emergency" in 1993,[15] and in 2006, the Stop TB Partnership developed a Global Plan to Stop Tuberculosis that aimed to save 14 million lives between its launch and 2015.[89] A number of targets they set were not achieved by 2015, mostly due to the increase in HIV-associated tuberculosis and the emergence of multiple drug-resistant tuberculosis.[15] A tuberculosis classification system developed by the American Thoracic Society is used primarily in public health programs.[90]
The benefits and risks of giving anti-tubercular drugs in those exposed to MDR-TB is unclear.[91]
Treatment
Treatment of TB uses antibiotics to kill the bacteria. Effective TB treatment is difficult, due to the unusual structure and chemical composition of the mycobacterial cell wall, which hinders the entry of drugs and makes many antibiotics ineffective.[92]
Active TB is best treated with combinations of several antibiotics to reduce the risk of the bacteria developing antibiotic resistance.[15] The routine use of rifabutin instead of rifampicin in HIV-positive people with tuberculosis is of unclear benefit as of 2007.[93]
Latent
Latent TB is treated with either isoniazid or rifampin alone, or a combination of isoniazid with either rifampicin or rifapentine.[94][95][96]
The treatment takes three to nine months depending on the medications used.[44][94][97][96] People with latent infections are treated to prevent them from progressing to active TB disease later in life.[98]
Education or counselling may improve the latent tuberculosis treatment completion rates.[99]
New onset
The recommended treatment of new-onset pulmonary tuberculosis, as of 2010, is six months of a combination of antibiotics containing rifampicin, isoniazid, pyrazinamide, and ethambutol for the first two months, and only rifampicin and isoniazid for the last four months.[15] Where resistance to isoniazid is high, ethambutol may be added for the last four months as an alternative.[15] Treatment with anti-TB drugs for at least 6 months results in higher success rates when compared with treatment less than 6 months; even though the difference is small. Shorter treatment regimen may be recommended for those with compliance issues.[100] There is also no evidence to support shorter anti-tubeculosis treatment regimen when compared to 6 months treatment regimen.[101]
Recurrent disease
If tuberculosis recurs, testing to determine which antibiotics it is sensitive to is important before determining treatment.[15] If multiple drug-resistant TB (MDR-TB) is detected, treatment with at least four effective antibiotics for 18 to 24 months is recommended.[15]
Medication administration
Directly observed therapy, i.e., having a health care provider watch the person take their medications, is recommended by the World Health Organization (WHO) in an effort to reduce the number of people not appropriately taking antibiotics.[102] The evidence to support this practice over people simply taking their medications independently is of poor quality.[103] There is no strong evidence indicating that directly observed therapy improves the number of people who were cured or the number of people who complete their medicine.[103] Moderate quality evidence suggests that there is also no difference if people are observed at home versus at a clinic, or by a family member versus a health care worker.[103] Methods to remind people of the importance of treatment and appointments may result in a small but important improvement.[104] There is also not enough evidence to support intermittent rifampicin-containing therapy given two to three times a week has equal effectiveness as daily dose regimen on improving cure rates and reducing relapsing rates.[105] There is also not enough evidence on effectiveness of giving intermittent twice or thrice weekly short course regimen compared to daily dosing regimen in treating children with tuberculosis.[106]
Medication resistance
Primary resistance occurs when a person becomes infected with a resistant strain of TB. A person with fully susceptible MTB may develop secondary (acquired) resistance during therapy because of inadequate treatment, not taking the prescribed regimen appropriately (lack of compliance), or using low-quality medication.[107] Drug-resistant TB is a serious public health issue in many developing countries, as its treatment is longer and requires more expensive drugs. MDR-TB is defined as resistance to the two most effective first-line TB drugs: rifampicin and isoniazid. Extensively drug-resistant TB is also resistant to three or more of the six classes of second-line drugs.[108] Totally drug-resistant TB is resistant to all currently used drugs.[109] It was first observed in 2003 in Italy,[110] but not widely reported until 2012,[109][111] and has also been found in Iran and India.[112][113] Bedaquiline is tentatively supported for use in multiple drug-resistant TB.[114]
XDR-TB is a term sometimes used to define extensively resistant TB, and constitutes one in ten cases of MDR-TB. Cases of XDR TB have been identified in more than 90% of countries.[112] There is some efficacy for linezolid to treat those with XDR-TB but side effects and discontinuation of medications were common.[115]
For those with known rifampicin or MDR-TB, Genotype® MTBDRsl Assay performed on culture isolates or smear positive specimens may be useful to detect second-line anti-tubercular drug resistance.[116]
Prognosis

|
no data
≤10
10–25
25–50
50–75
75–100
100–250
|
250–500
500–750
750–1000
1000–2000
2000–3000
≥ 3000
|
Progression from TB infection to overt TB disease occurs when the bacilli overcome the immune system defenses and begin to multiply. In primary TB disease (some 1–5% of cases), this occurs soon after the initial infection.[14] However, in the majority of cases, a latent infection occurs with no obvious symptoms.[14] These dormant bacilli produce active tuberculosis in 5–10% of these latent cases, often many years after infection.[17]
The risk of reactivation increases with immunosuppression, such as that caused by infection with HIV. In people coinfected with M. tuberculosis and HIV, the risk of reactivation increases to 10% per year.[14] Studies using DNA fingerprinting of M. tuberculosis strains have shown reinfection contributes more substantially to recurrent TB than previously thought,[118] with estimates that it might account for more than 50% of reactivated cases in areas where TB is common.[119] The chance of death from a case of tuberculosis is about 4% as of 2008, down from 8% in 1995.[15]
In people with smear-positive pulmonary TB (without HIV co-infection), after 5 years without treatment, 50-60% die while 20-25% achieve spontaneous resolution (cure). TB is almost always fatal in those with untreated HIV co-infection and death rates are increased even with antiretroviral treatment of HIV.[120]
Epidemiology
Roughly one-quarter of the world's population has been infected with M. tuberculosis,[6] with new infections occurring in about 1% of the population each year.[12] However, most infections with M. tuberculosis do not cause TB disease,[121] and 90–95% of infections remain asymptomatic.[55] In 2012, an estimated 8.6 million chronic cases were active.[122] In 2010, 8.8 million new cases of TB were diagnosed, and 1.20–1.45 million deaths occurred (most of these occurring in developing countries).[47][123] Of these, about 0.35 million occur in those also infected with HIV.[124] In 2018, tuberculosis was the leading cause of death worldwide from a single infectious agent.[125] The total number of tuberculosis cases has been decreasing since 2005, while new cases have decreased since 2002.[47]
Tuberculosis incidence is seasonal, with peaks occurring every spring/summer.[126][127][128][129] The reasons for this are unclear, but may be related to vitamin D deficiency during the winter.[129][130] There are also studies linking Tuberculosis to different weather conditions like low temperature, low humidity and low rainfall. It has also been suggested that Tuberculosis incidence rates may be connected to climate change.[131]
At-risk groups
Tuberculosis is closely linked to both overcrowding and malnutrition, making it one of the principal diseases of poverty.[15] Those at high risk thus include: people who inject illicit drugs, inhabitants and employees of locales where vulnerable people gather (e.g. prisons and homeless shelters), medically underprivileged and resource-poor communities, high-risk ethnic minorities, children in close contact with high-risk category patients, and health-care providers serving these patients.[132]
The rate of TB varies with age. In Africa, it primarily affects adolescents and young adults.[133] However, in countries where incidence rates have declined dramatically (such as the United States), TB is mainly a disease of older people and the immunocompromised (risk factors are listed above).[14][134] Worldwide, 22 "high-burden" states or countries together experience 80% of cases as well as 83% of deaths.[112]
In Canada and Australia, tuberculosis is many times more common among the aboriginal peoples, especially in remote areas.[135][136] Factors contributing to this include higher prevalence of predisposing health conditions and behaviours, and overcrowding and poverty. In some Canadian aboriginal groups, genetic susceptibility may play a role.[46]
Socioeconomic status (SES) strongly affects TB risk. People of low SES are both more likely to contract TB and to be more severely affected by the disease. Those with low SES are more likely to be affected by risk factors for developing TB (e.g. malnutrition, indoor air pollution, HIV co-infection, etc.), and are additionally more likely to be exposed to crowded and poorly ventilated spaces. Inadequate healthcare also means that people with active disease who facilitate spread are not diagnosed and treated promptly; sick people thus remain in the infectious state and (continue to) spread the infection.[46]
Geographical epidemiology
The distribution of tuberculosis is not uniform across the globe; about 80% of the population in many African, Caribbean, south Asian, and eastern European countries test positive in tuberculin tests, while only 5–10% of the U.S. population test positive.[14] Hopes of totally controlling the disease have been dramatically dampened because of a number of factors, including the difficulty of developing an effective vaccine, the expensive and time-consuming diagnostic process, the necessity of many months of treatment, the increase in HIV-associated tuberculosis, and the emergence of drug-resistant cases in the 1980s.[15]
In developed countries, tuberculosis is less common and is found mainly in urban areas. In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health, such that when the Medical Research Council was formed in Britain in 1913 its initial focus was tuberculosis research.[137]
In 2010, rates per 100,000 people in different areas of the world were: globally 178, Africa 332, the Americas 36, Eastern Mediterranean 173, Europe 63, Southeast Asia 278, and Western Pacific 139.[124]
Russia
Russia has achieved particularly dramatic progress with decline in its TB mortality rate—from 61.9 per 100,000 in 1965 to 2.7 per 100,000 in 1993;[138][139] however, mortality rate increased to 24 per 100,000 in 2005 and then recoiled to 11 per 100,000 by 2015.[140]
China
China has achieved particularly dramatic progress, with about an 80% reduction in its TB mortality rate between 1990 and 2010.[124] The number of new cases has declined by 17% between 2004 and 2014.[112]
Africa
In 2007, the country with the highest estimated incidence rate of TB was Eswatini, with 1,200 cases per 100,000 people. In 2017, the country with the highest estimated incidence rate as a % of the population was Lesotho, with 665 cases per 100,000 people.[141]
India
As of 2017, India had the largest total incidence, with an estimated 2 740 000 cases.[141] According to the World Health Organization (WHO), in 2000–2015, India's estimated mortality rate dropped from 55 to 36 per 100 000 population per year with estimated 480 thousand people died of TB in 2015.[142][143] In India a major proportion of tuberculosis patient are being treated by private partners and private hospitals. Evidence indicates that the tuberculosis national survey does not represent the number of cases that are diagnosed and recorded by private clinics and hospitals in India [144]
North America
In the United States Native Americans have a fivefold greater mortality from TB,[145] and racial and ethnic minorities accounted for 84% of all reported TB cases.[146]
In the United States, the overall tuberculosis case rate was 3 per 100,000 persons in 2017.[141] In Canada, tuberculosis is still endemic in some rural areas.[147]
Western Europe
In 2017, in the United Kingdom, the national average was 9 per 100,000 and the highest incidence rates in Western Europe were 20 per 100,000 in Portugal.
History

Tuberculosis has existed since antiquity.[15] The oldest unambiguously detected M. tuberculosis gives evidence of the disease in the remains of bison in Wyoming dated to around 17,000 years ago.[150] However, whether tuberculosis originated in bovines, then transferred to humans, or whether both bovine and human tuberculosis diverged from a common ancestor, remains unclear.[151] A comparison of the genes of M. tuberculosis complex (MTBC) in humans to MTBC in animals suggests humans did not acquire MTBC from animals during animal domestication, as researchers previously believed. Both strains of the tuberculosis bacteria share a common ancestor, which could have infected humans even before the Neolithic Revolution.[152] Skeletal remains show some prehistoric humans (4000 BC) had TB, and researchers have found tubercular decay in the spines of Egyptian mummies dating from 3000 to 2400 BC.[153] Genetic studies suggest the presence of TB in the Americas from about 100 AD.[154]
Before the Industrial Revolution, folklore often associated tuberculosis with vampires. When one member of a family died from the disease, the other infected members would lose their health slowly. People believed this was caused by the original person with TB draining the life from the other family members.[155]
Although Richard Morton established the pulmonary form associated with tubercles as a pathology in 1689,[156][157] due to the variety of its symptoms, TB was not identified as a single disease until the 1820s. Benjamin Marten conjectured in 1720 that consumptions were caused by microbes which were spread by people living in close proximity to each other.[158] In 1819 René Laennec claimed that tubercles were the cause of pulmonary tuberculosis.[159] J. L. Schönlein first published the name "tuberculosis" (German: Tuberkulose) in 1832.[160][161] Between 1838 and 1845, Dr. John Croghan, the owner of Mammoth Cave in Kentucky from 1839 onwards, brought a number of people with tuberculosis into the cave in the hope of curing the disease with the constant temperature and purity of the cave air; each died within a year.[162] Hermann Brehmer opened the first TB sanatorium in 1859 in Görbersdorf (now Sokołowsko) in Silesia.[163] In 1865 Jean Antoine Villemin demonstrated that tuberculosis could be transmitted, via inoculation, from humans to animals and among animals.[164] (Villemin's findings were confirmed in 1867 and 1868 by John Burdon-Sanderson.[165])
Robert Koch identified and described the bacillus causing tuberculosis, M. tuberculosis, on 24 March 1882.[166] He received the Nobel Prize in physiology or medicine in 1905 for this discovery.[167] Koch did not believe the cattle and human tuberculosis diseases were similar, which delayed the recognition of infected milk as a source of infection. During the first half of the 1900s the risk of transmission from this source was dramatically reduced after the application of the pasteurization process. Koch announced a glycerine extract of the tubercle bacilli as a "remedy" for tuberculosis in 1890, calling it "tuberculin". Although it was not effective, it was later successfully adapted as a screening test for the presence of pre-symptomatic tuberculosis.[168] World Tuberculosis Day is marked on 24 March each year, the anniversary of Koch's original scientific announcement.
Albert Calmette and Camille Guérin achieved the first genuine success in immunization against tuberculosis in 1906, using attenuated bovine-strain tuberculosis. It was called bacille Calmette–Guérin (BCG). The BCG vaccine was first used on humans in 1921 in France,[169] but achieved widespread acceptance in the US, Great Britain, and Germany only after World War II.[170]
Tuberculosis caused widespread public concern in the 19th and early 20th centuries as the disease became common among the urban poor. In 1815 one in four deaths in England was due to "consumption". By 1918, TB still caused one in six deaths in France. After TB was determined to be contagious, in the 1880s, it was put on a notifiable-disease list in Britain; campaigns started to stop people from spitting in public places, and the infected poor were "encouraged" to enter sanatoria that resembled prisons (the sanatoria for the middle and upper classes offered excellent care and constant medical attention).[163] Whatever the benefits of the "fresh air" and labor in the sanatoria, even under the best conditions, 50% of those who entered died within five years (c. 1916).[163] When the Medical Research Council formed in Britain in 1913, it initially focused on tuberculosis research.[171]
In Europe, rates of tuberculosis began to rise in the early 1600s to a peak level in the 1800s, when it caused nearly 25% of all deaths.[172] By the 1950s mortality in Europe had decreased about 90%.[173] Improvements in sanitation, vaccination, and other public-health measures began significantly reducing rates of tuberculosis even before the arrival of streptomycin and other antibiotics, although the disease remained a significant threat.[173] In 1946 the development of the antibiotic streptomycin made effective treatment and cure of TB a reality. Prior to the introduction of this medication, the only treatment was surgical intervention, including the "pneumothorax technique", which involved collapsing an infected lung to "rest" it and to allow tuberculous lesions to heal.[174]
Because of the emergence of MDR-TB, surgery has been re-introduced for certain cases of TB infections. It involves the removal of infected chest cavities ("bullae") in the lungs to reduce the number of bacteria and to increase exposure of the remaining bacteria to antibiotics in the bloodstream.[175] Hopes of completely eliminating TB ended with the rise of drug-resistant strains in the 1980s. The subsequent resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization (WHO) in 1993.[176]
Society and culture
Names
Tuberculosis has been known by many names from the technical to the familiar.[177] Phthisis (Φθισις) is a Greek word for consumption, an old term for pulmonary tuberculosis;[8] around 460 BCE, Hippocrates described phthisis as a disease of dry seasons.[178] The abbreviation "TB" is short for tubercle bacillus. "Consumption" was the most common nineteenth century English word for the disease. The Latin root "con" meaning "completely" is linked to "sumere" meaning "to take up from under."[179] In The Life and Death of Mr Badman by John Bunyan, the author calls consumption "the captain of all these men of death."[180] "Great white plague" has also been used.[177]
Art and literature

Tuberculosis was for centuries associated with poetic and artistic qualities among those infected, and was also known as "the romantic disease".[177][181] Major artistic figures such as the poets John Keats, Percy Bysshe Shelley, and Edgar Allan Poe, the composer Frédéric Chopin,[182] the playwright Anton Chekhov, the novelists Franz Kafka, Katherine Mansfield,[183] Charlotte Brontë, Fyodor Dostoevsky, Thomas Mann, W. Somerset Maugham,[184] George Orwell,[185] and Robert Louis Stevenson, and the artists Alice Neel,[186] Jean-Antoine Watteau, Elizabeth Siddal, Marie Bashkirtseff, Edvard Munch, Aubrey Beardsley and Amedeo Modigliani either had the disease or were surrounded by people who did. A widespread belief was that tuberculosis assisted artistic talent. Physical mechanisms proposed for this effect included the slight fever and toxaemia that it caused, allegedly helping them to see life more clearly and to act decisively.[187][188][189]
Tuberculosis formed an often-reused theme in literature, as in Thomas Mann's The Magic Mountain, set in a sanatorium;[190] in music, as in Van Morrison's song "T.B. Sheets";[191] in opera, as in Puccini's La bohème and Verdi's La Traviata;[189] in art, as in Monet's painting of his first wife Camille on her deathbed;[192] and in film, such as the 1945 The Bells of St. Mary's starring Ingrid Bergman as a nun with tuberculosis.[193]
Public health efforts
The World Health Organization (WHO), the Bill and Melinda Gates Foundation, and the U.S. government are subsidizing a fast-acting diagnostic tuberculosis test for use in low- and middle-income countries as of 2012.[194][195][196] In addition to being fast-acting, the test can determine if there is resistance to the antibiotic rifampicin which may indicate multi-drug resistant tuberculosis and is accurate in those who are also infected with HIV.[194][197] Many resource-poor places as of 2011 have access to only sputum microscopy.[198]
India had the highest total number of TB cases worldwide in 2010, in part due to poor disease management within the private and public health care sector. Programs such as the Revised National Tuberculosis Control Program are working to reduce TB levels among people receiving public health care.[199][200]
A 2014 the EIU-healthcare report finds there is a need to address apathy and urges for increased funding. The report cites among others Lucica Ditui "[TB] is like an orphan. It has been neglected even in countries with a high burden and often forgotten by donors and those investing in health interventions."[112]
Slow progress has led to frustration, expressed by the executive director of the Global Fund to Fight AIDS, Tuberculosis and Malaria – Mark Dybul: "we have the tools to end TB as a pandemic and public health threat on the planet, but we are not doing it."[112] Several international organizations are pushing for more transparency in treatment, and more countries are implementing mandatory reporting of cases to the government as of 2014, although adherence is often variable. Commercial treatment providers may at times overprescribe second-line drugs as well as supplementary treatment, promoting demands for further regulations.[112] The government of Brazil provides universal TB-care, which reduces this problem.[112] Conversely, falling rates of TB-infection may not relate to the number of programs directed at reducing infection rates but may be tied to increased level of education, income, and health of the population.[112] Costs of the disease, as calculated by the World Bank in 2009 may exceed US$150 billion per year in "high burden" countries.[112] Lack of progress eradicating the disease may also be due to lack of patient follow-up – as among the 250M rural migrants in China.[112]
There is insufficient data to show that active contact tracing helps to improve case detection rates for tuberculosis.[201] Interventions such as house-to-house visits, educational leaflets, mass media strategies, educational sessions may increase tuberculosis detection rates in short-term.[202] There is no study that compare new method of contact tracing such as social network analysis with existing contact tracing methods.[203]
Stigma
Slow progress in preventing the disease may in part be due to stigma associated with TB.[112] Stigma may be due to the fear of transmission from affected individuals. This stigma may additionally arise due to links between TB and poverty, and in Africa, AIDS.[112] Such stigmatization may be both real and perceived; for example, in Ghana individuals with TB are banned from attending public gatherings.[204]
Stigma towards TB may result in delays in seeking treatment,[112] lower treatment compliance, and family members keeping cause of death secret[204] – allowing the disease to spread further.[112] In contrast, in Russia stigma was associated with increased treatment compliance.[204] TB stigma also affects socially marginalized individuals to a greater degree and varies between regions.[204]
One way to decrease stigma may be through the promotion of "TB clubs", where those infected may share experiences and offer support, or through counseling.[204] Some studies have shown TB education programs to be effective in decreasing stigma, and may thus be effective in increasing treatment adherence.[204] Despite this, studies on the relationship between reduced stigma and mortality are lacking as of 2010, and similar efforts to decrease stigma surrounding AIDS have been minimally effective.[204] Some have claimed the stigma to be worse than the disease, and healthcare providers may unintentionally reinforce stigma, as those with TB are often perceived as difficult or otherwise undesirable.[112] A greater understanding of the social and cultural dimensions of tuberculosis may also help with stigma reduction.[205]
Research
The BCG vaccine has limitations, and research to develop new TB vaccines is ongoing.[206] A number of potential candidates are currently in phase I and II clinical trials.[206][207] Two main approaches are used to attempt to improve the efficacy of available vaccines. One approach involves adding a subunit vaccine to BCG, while the other strategy is attempting to create new and better live vaccines.[206] MVA85A, an example of a subunit vaccine, is in trials in South Africa as of 2006, is based on a genetically modified vaccinia virus.[208] Vaccines are hoped to play a significant role in treatment of both latent and active disease.[209]
To encourage further discovery, researchers and policymakers are promoting new economic models of vaccine development as of 2006, including prizes, tax incentives, and advance market commitments.[210][211] A number of groups, including the Stop TB Partnership,[212] the South African Tuberculosis Vaccine Initiative, and the Aeras Global TB Vaccine Foundation, are involved with research.[213] Among these, the Aeras Global TB Vaccine Foundation received a gift of more than $280 million (US) from the Bill and Melinda Gates Foundation to develop and license an improved vaccine against tuberculosis for use in high burden countries.[214][215]
A number of medications are being studied as of 2012 for multidrug-resistant tuberculosis, including bedaquiline and delamanid.[216] Bedaquiline received U.S. Food and Drug Administration (FDA) approval in late 2012.[217] The safety and effectiveness of these new agents are uncertain as of 2012, because they are based on the results of relatively small studies.[216][218] However, existing data suggest that patients taking bedaquiline in addition to standard TB therapy are five times more likely to die than those without the new drug,[219] which has resulted in medical journal articles raising health policy questions about why the FDA approved the drug and whether financial ties to the company making bedaquiline influenced physicians' support for its use.[218][220]
Steroids add-on therapy has not shown any benefits for people with active pulmonary tuberculosis infection.[221]
Other animals
Mycobacteria infect many different animals, including birds,[222] fish, rodents,[223] and reptiles.[224] The subspecies Mycobacterium tuberculosis, though, is rarely present in wild animals.[225] An effort to eradicate bovine tuberculosis caused by Mycobacterium bovis from the cattle and deer herds of New Zealand has been relatively successful.[226] Efforts in Great Britain have been less successful.[227][228]
As of 2015, tuberculosis appears to be widespread among captive elephants in the US. It is believed that the animals originally acquired the disease from humans, a process called reverse zoonosis. Because the disease can spread through the air to infect both humans and other animals, it is a public health concern affecting circuses and zoos.[229][230]
References
- "Tuberculosis (TB)". www.who.int. Retrieved 8 May 2020.
- Ferri FF (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter T. ISBN 978-0-323-07699-9.
- Hawn TR, Day TA, Scriba TJ, Hatherill M, Hanekom WA, Evans TG, et al. (December 2014). "Tuberculosis vaccines and prevention of infection". Microbiology and Molecular Biology Reviews. 78 (4): 650–71. doi:10.1128/MMBR.00021-14. PMC 4248657. PMID 25428938.
- Organization, World Health (2008). Implementing the WHO Stop TB Strategy: a handbook for national TB control programmes. Geneva: World Health Organization (WHO). p. 179. ISBN 978-92-4-154667-6.
- Harris RE (2013). Epidemiology of chronic disease: global perspectives. Burlington, MA: Jones & Bartlett Learning. p. 682. ISBN 978-0-7637-8047-0.
- "Tuberculosis (TB)". World Health Organization (WHO). 16 February 2018. Retrieved 15 September 2018.
- "Global Tuberculosis Report" (PDF). WHO. WHO. 2019. Retrieved 24 March 2020.
- The Chambers Dictionary. New Delhi: Allied Chambers India Ltd. 1998. p. 352. ISBN 978-81-86062-25-8. Archived from the original on 6 September 2015.
- Adkinson NF, Bennett JE, Douglas RG, Mandell GL (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia, PA: Churchill Livingstone/Elsevier. p. Chapter 250. ISBN 978-0-443-06839-3.
- "Basic TB Facts". Centers for Disease Control and Prevention (CDC). 13 March 2012. Archived from the original on 6 February 2016. Retrieved 11 February 2016.
- Konstantinos A (2010). "Testing for tuberculosis". Australian Prescriber. 33 (1): 12–18. doi:10.18773/austprescr.2010.005.
- "Tuberculosis". World Health Organization (WHO). 2002. Archived from the original on 17 June 2013.
- "Global tuberculosis report". World Health Organization (WHO). Retrieved 9 November 2017.
- Kumar V, Robbins SL (2007). Robbins Basic Pathology (8th ed.). Philadelphia: Elsevier. ISBN 978-1-4160-2973-1. OCLC 69672074.
- Lawn SD, Zumla AI (July 2011). "Tuberculosis". Lancet. 378 (9785): 57–72. doi:10.1016/S0140-6736(10)62173-3. PMID 21420161. S2CID 208791546.
- Schiffman G (15 January 2009). "Tuberculosis Symptoms". eMedicine Health. Archived from the original on 16 May 2009.
- Gibson PG, Abramson M, Wood-Baker R, Volmink J, Hensley M, Costabel U, eds. (2005). Evidence-Based Respiratory Medicine (1st ed.). BMJ Books. p. 321. ISBN 978-0-7279-1605-1. Archived from the original on 8 December 2015.
- Behera D (2010). Textbook of Pulmonary Medicine (2nd ed.). New Delhi: Jaypee Brothers Medical Publishers. p. 457. ISBN 978-81-8448-749-7. Archived from the original on 6 September 2015.
- Halezeroğlu S, Okur E (March 2014). "Thoracic surgery for haemoptysis in the context of tuberculosis: what is the best management approach?". Journal of Thoracic Disease. 6 (3): 182–85. doi:10.3978/j.issn.2072-1439.2013.12.25. PMC 3949181. PMID 24624281.
- Jindal SK, ed. (2011). Textbook of Pulmonary and Critical Care Medicine. New Delhi: Jaypee Brothers Medical Publishers. p. 549. ISBN 978-93-5025-073-0. Archived from the original on 7 September 2015.
- Golden MP, Vikram HR (November 2005). "Extrapulmonary tuberculosis: an overview". American Family Physician. 72 (9): 1761–68. PMID 16300038.
- Habermann TM, Ghosh A (2008). Mayo Clinic internal medicine: concise textbook. Rochester, MN: Mayo Clinic Scientific Press. p. 789. ISBN 978-1-4200-6749-1. Archived from the original on 6 September 2015.
- Southwick F (2007). "Chapter 4: Pulmonary Infections". Infectious Diseases: A Clinical Short Course, 2nd ed. McGraw-Hill Medical Publishing Division. pp. 104, 313–14. ISBN 978-0-07-147722-2.
- Jindal SK (2011). Textbook of Pulmonary and Critical Care Medicine. New Delhi: Jaypee Brothers Medical Publishers. p. 525. ISBN 978-93-5025-073-0. Archived from the original on 6 September 2015.
- Niederweis M, Danilchanka O, Huff J, Hoffmann C, Engelhardt H (March 2010). "Mycobacterial outer membranes: in search of proteins". Trends in Microbiology. 18 (3): 109–16. doi:10.1016/j.tim.2009.12.005. PMC 2931330. PMID 20060722.
- Madison BM (May 2001). "Application of stains in clinical microbiology". Biotechnic & Histochemistry. 76 (3): 119–25. doi:10.1080/714028138. PMID 11475314.
- Parish T, Stoker NG (December 1999). "Mycobacteria: bugs and bugbears (two steps forward and one step back)". Molecular Biotechnology. 13 (3): 191–200. doi:10.1385/MB:13:3:191. PMID 10934532. S2CID 28960959.
- Medical Laboratory Science: Theory and Practice. New Delhi: Tata McGraw-Hill. 2000. p. 473. ISBN 978-0-07-463223-9. Archived from the original on 6 September 2015.
- "Acid-Fast Stain Protocols". 21 August 2013. Archived from the original on 1 October 2011. Retrieved 26 March 2016.
- Kommareddi S, Abramowsky CR, Swinehart GL, Hrabak L (November 1984). "Nontuberculous mycobacterial infections: comparison of the fluorescent auramine-O and Ziehl-Neelsen techniques in tissue diagnosis". Human Pathology. 15 (11): 1085–9. doi:10.1016/S0046-8177(84)80253-1. PMID 6208117.
- van Lettow M, Whalen C (2008). Semba RD, Bloem MW (eds.). Nutrition and health in developing countries (2nd ed.). Totowa, N.J.: Humana Press. p. 291. ISBN 978-1-934115-24-4. Archived from the original on 6 September 2015.
- van Soolingen D, Hoogenboezem T, de Haas PE, Hermans PW, Koedam MA, Teppema KS, et al. (October 1997). "A novel pathogenic taxon of the Mycobacterium tuberculosis complex, Canetti: characterization of an exceptional isolate from Africa". International Journal of Systematic Bacteriology. 47 (4): 1236–45. doi:10.1099/00207713-47-4-1236. PMID 9336935.
- Niemann S, Rüsch-Gerdes S, Joloba ML, Whalen CC, Guwatudde D, Ellner JJ, et al. (September 2002). "Mycobacterium africanum subtype II is associated with two distinct genotypes and is a major cause of human tuberculosis in Kampala, Uganda". Journal of Clinical Microbiology. 40 (9): 3398–405. doi:10.1128/JCM.40.9.3398-3405.2002. PMC 130701. PMID 12202584.
- Niobe-Eyangoh SN, Kuaban C, Sorlin P, Cunin P, Thonnon J, Sola C, et al. (June 2003). "Genetic biodiversity of Mycobacterium tuberculosis complex strains from patients with pulmonary tuberculosis in Cameroon". Journal of Clinical Microbiology. 41 (6): 2547–53. doi:10.1128/JCM.41.6.2547-2553.2003. PMC 156567. PMID 12791879.
- Thoen C, Lobue P, de Kantor I (February 2006). "The importance of Mycobacterium bovis as a zoonosis". Veterinary Microbiology. 112 (2–4): 339–45. doi:10.1016/j.vetmic.2005.11.047. PMID 16387455.
- Acton QA (2011). Mycobacterium Infections: New Insights for the Healthcare Professional. ScholarlyEditions. p. 1968. ISBN 978-1-4649-0122-5. Archived from the original on 6 September 2015.
- Pfyffer GE, Auckenthaler R, van Embden JD, van Soolingen D (1998). "Mycobacterium canettii, the smooth variant of M. tuberculosis, isolated from a Swiss patient exposed in Africa". Emerging Infectious Diseases. 4 (4): 631–4. doi:10.3201/eid0404.980414. PMC 2640258. PMID 9866740.
- Panteix G, Gutierrez MC, Boschiroli ML, Rouviere M, Plaidy A, Pressac D, et al. (August 2010). "Pulmonary tuberculosis due to Mycobacterium microti: a study of six recent cases in France". Journal of Medical Microbiology. 59 (Pt 8): 984–989. doi:10.1099/jmm.0.019372-0. PMID 20488936.
- American Thoracic Society (August 1997). "Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association". American Journal of Respiratory and Critical Care Medicine. 156 (2 Pt 2): S1–25. doi:10.1164/ajrccm.156.2.atsstatement. PMID 9279284.
- Cole EC, Cook CE (August 1998). "Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies". American Journal of Infection Control. 26 (4): 453–64. doi:10.1016/S0196-6553(98)70046-X. PMC 7132666. PMID 9721404.
- Nicas M, Nazaroff WW, Hubbard A (March 2005). "Toward understanding the risk of secondary airborne infection: emission of respirable pathogens". Journal of Occupational and Environmental Hygiene. 2 (3): 143–54. doi:10.1080/15459620590918466. PMC 7196697. PMID 15764538.
- Ahmed N, Hasnain SE (September 2011). "Molecular epidemiology of tuberculosis in India: moving forward with a systems biology approach". Tuberculosis. 91 (5): 407–13. doi:10.1016/j.tube.2011.03.006. PMID 21514230.
- "Tuberculosis Fact sheet N°104". World Health Organization (WHO). November 2010. Archived from the original on 4 October 2006. Retrieved 26 July 2011.
- "Core Curriculum on Tuberculosis: What the Clinician Should Know" (PDF) (5th ed.). Centers for Disease Control and Prevention (CDC), Division of Tuberculosis Elimination. 2011. p. 24. Archived (PDF) from the original on 19 May 2012.
- "Causes of Tuberculosis". Mayo Clinic. 21 December 2006. Archived from the original on 18 October 2007. Retrieved 19 October 2007.
- Narasimhan, Padmanesan; Wood, James; MacIntyre, Chandini Raina; Mathai, Dilip (2013). "Risk Factors for Tuberculosis". Pulmonary Medicine. 2013: 828939. doi:10.1155/2013/828939. ISSN 2090-1836. PMC 3583136. PMID 23476764.
- "The sixteenth global report on tuberculosis" (PDF). World Health Organization (WHO). 2011. Archived from the original (PDF) on 6 September 2012.
- "Global tuberculosis control–surveillance, planning, financing WHO Report 2006". World Health Organization (WHO). Archived from the original on 12 December 2006. Retrieved 13 October 2006.
- Chaisson RE, Martinson NA (March 2008). "Tuberculosis in Africa – combating an HIV-driven crisis". The New England Journal of Medicine. 358 (11): 1089–92. doi:10.1056/NEJMp0800809. PMID 18337598.
- Restrepo BI (August 2007). "Convergence of the tuberculosis and diabetes epidemics: renewal of old acquaintances". Clinical Infectious Diseases. 45 (4): 436–38. doi:10.1086/519939. PMC 2900315. PMID 17638190.
- "Targeted tuberculin testing and treatment of latent tuberculosis infection. American Thoracic Society". MMWR. Recommendations and Reports. 49 (RR-6): 1–51. June 2000. PMID 10881762. Archived from the original on 17 December 2004.
- van Zyl Smit RN, Pai M, Yew WW, Leung CC, Zumla A, Bateman ED, et al. (January 2010). "Global lung health: the colliding epidemics of tuberculosis, tobacco smoking, HIV and COPD". The European Respiratory Journal. 35 (1): 27–33. doi:10.1183/09031936.00072909. PMC 5454527. PMID 20044459.
These analyses indicate that smokers are almost twice as likely to be infected with TB and to progress to active disease (RR of about 1.5 for latent TB infection (LTBI) and RR of ∼2.0 for TB disease). Smokers are also twice as likely to die from TB (RR of about 2.0 for TB mortality), but data are difficult to interpret because of heterogeneity in the results across studies.
- "TB Risk Factors | Basic TB Facts | TB | CDC". www.cdc.gov. 26 May 2020. Retrieved 25 August 2020.
- Möller M, Hoal EG (March 2010). "Current findings, challenges and novel approaches in human genetic susceptibility to tuberculosis". Tuberculosis. 90 (2): 71–83. doi:10.1016/j.tube.2010.02.002. PMID 20206579.
- Skolnik R (2011). Global health 101 (2nd ed.). Burlington, MA: Jones & Bartlett Learning. p. 253. ISBN 978-0-7637-9751-5.
- Mainous III AG, Pomeroy C (2009). Management of antimicrobials in infectious diseases: impact of antibiotic resistance (2nd rev. ed.). Totowa, NJ: Humana Press. p. 74. ISBN 978-1-60327-238-4. Archived from the original on 6 September 2015.
- Houben EN, Nguyen L, Pieters J (February 2006). "Interaction of pathogenic mycobacteria with the host immune system". Current Opinion in Microbiology. 9 (1): 76–85. doi:10.1016/j.mib.2005.12.014. PMID 16406837.
- Queval CJ, Brosch R, Simeone R (2017). "Mycobacterium tuberculosis". Frontiers in Microbiology. 8: 2284. doi:10.3389/fmicb.2017.02284. PMC 5703847. PMID 29218036.
- Khan (2011). Essence of Paediatrics. Elsevier India. p. 401. ISBN 978-81-312-2804-3. Archived from the original on 6 September 2015.
- Herrmann JL, Lagrange PH (February 2005). "Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse?". Pathologie-Biologie. 53 (1): 35–40. doi:10.1016/j.patbio.2004.01.004. PMID 15620608.
- Agarwal R, Malhotra P, Awasthi A, Kakkar N, Gupta D (April 2005). "Tuberculous dilated cardiomyopathy: an under-recognized entity?". BMC Infectious Diseases. 5 (1): 29. doi:10.1186/1471-2334-5-29. PMC 1090580. PMID 15857515.
- Good JM, Cooper S, Doane AS (1835). The Study of Medicine. Harper. p. 32. Archived from the original on 10 August 2016.
- Grosset J (March 2003). "Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary". Antimicrobial Agents and Chemotherapy. 47 (3): 833–36. doi:10.1128/AAC.47.3.833-836.2003. PMC 149338. PMID 12604509.
- Bozzano F, Marras F, De Maria A (2014). "Immunology of tuberculosis". Mediterranean Journal of Hematology and Infectious Diseases. 6 (1): e2014027. doi:10.4084/MJHID.2014.027. PMC 4010607. PMID 24804000.
- Crowley LV (2010). An introduction to human disease: pathology and pathophysiology correlations (8th ed.). Sudbury, MA: Jones and Bartlett. p. 374. ISBN 978-0-7637-6591-0. Archived from the original on 6 September 2015.
- Anthony H (2005). TB/HIV a Clinical Manual (2nd ed.). Geneva: World Health Organization (WHO). p. 75. ISBN 978-92-4-154634-8. Archived from the original on 6 September 2015.
- Jacob JT, Mehta AK, Leonard MK (January 2009). "Acute forms of tuberculosis in adults". The American Journal of Medicine. 122 (1): 12–17. doi:10.1016/j.amjmed.2008.09.018. PMID 19114163.
- Bento J, Silva AS, Rodrigues F, Duarte R (2011). "[Diagnostic tools in tuberculosis]". Acta Medica Portuguesa. 24 (1): 145–54. PMID 21672452.
- Escalante P (June 2009). "In the clinic. Tuberculosis". Annals of Internal Medicine. 150 (11): ITC61-614, quiz ITV616. doi:10.7326/0003-4819-150-11-200906020-01006. PMID 19487708. S2CID 639982.
- Metcalfe JZ, Everett CK, Steingart KR, Cattamanchi A, Huang L, Hopewell PC, Pai M (November 2011). "Interferon-γ release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis". The Journal of Infectious Diseases. 204 Suppl 4 (suppl_4): S1120-9. doi:10.1093/infdis/jir410. PMC 3192542. PMID 21996694.
- Sester M, Sotgiu G, Lange C, Giehl C, Girardi E, Migliori GB, et al. (January 2011). "Interferon-γ release assays for the diagnosis of active tuberculosis: a systematic review and meta-analysis". The European Respiratory Journal. 37 (1): 100–11. doi:10.1183/09031936.00114810. PMID 20847080.
- Chen J, Zhang R, Wang J, Liu L, Zheng Y, Shen Y, et al. (2011). Vermund SH (ed.). "Interferon-gamma release assays for the diagnosis of active tuberculosis in HIV-infected patients: a systematic review and meta-analysis". PLOS ONE. 6 (11): e26827. Bibcode:2011PLoSO...626827C. doi:10.1371/journal.pone.0026827. PMC 3206065. PMID 22069472.
- Diseases, Special Programme for Research & Training in Tropical (2006). Diagnostics for tuberculosis: global demand and market potential. Geneva: World Health Organization (WHO). p. 36. ISBN 978-92-4-156330-7. Archived from the original on 6 September 2015.
- National Institute for Health and Clinical Excellence. Clinical guideline 117: Tuberculosis. London, 2011.
- Steingart KR, Flores LL, Dendukuri N, Schiller I, Laal S, Ramsay A, et al. (August 2011). Evans C (ed.). "Commercial serological tests for the diagnosis of active pulmonary and extrapulmonary tuberculosis: an updated systematic review and meta-analysis". PLOS Medicine. 8 (8): e1001062. doi:10.1371/journal.pmed.1001062. PMC 3153457. PMID 21857806.
- Rothel JS, Andersen P (December 2005). "Diagnosis of latent Mycobacterium tuberculosis infection: is the demise of the Mantoux test imminent?". Expert Review of Anti-Infective Therapy. 3 (6): 981–93. doi:10.1586/14787210.3.6.981. PMID 16307510. S2CID 25423684.
- Pai M, Zwerling A, Menzies D (August 2008). "Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update". Annals of Internal Medicine. 149 (3): 177–84. doi:10.7326/0003-4819-149-3-200808050-00241. PMC 2951987. PMID 18593687.
- Jindal SK, ed. (2011). Textbook of Pulmonary and Critical Care Medicine. New Delhi: Jaypee Brothers Medical Publishers. p. 544. ISBN 978-93-5025-073-0. Archived from the original on 6 September 2015.
- Amicosante M, Ciccozzi M, Markova R (April 2010). "Rational use of immunodiagnostic tools for tuberculosis infection: guidelines and cost effectiveness studies". The New Microbiologica. 33 (2): 93–107. PMID 20518271.
- Bibbins-Domingo K, Grossman DC, Curry SJ, Bauman L, Davidson KW, Epling JW, et al. (September 2016). "Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement". JAMA. 316 (9): 962–9. doi:10.1001/jama.2016.11046. PMID 27599331.
- Gill J, Prasad V (November 2019). "Testing Healthcare Workers for Latent Tuberculosis: Is It Evidence Based, Bio-Plausible, Both, Or Neither?". The American Journal of Medicine. 132 (11): 1260–1261. doi:10.1016/j.amjmed.2019.03.017. PMID 30946831.
- Sosa LE, Njie GJ, Lobato MN, Bamrah Morris S, Buchta W, Casey ML, et al. (May 2019). "Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations from the National Tuberculosis Controllers Association and CDC, 2019". MMWR. Morbidity and Mortality Weekly Report. 68 (19): 439–443. doi:10.15585/mmwr.mm6819a3. PMC 6522077. PMID 31099768.
- McShane H (October 2011). "Tuberculosis vaccines: beyond bacille Calmette-Guerin". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 366 (1579): 2782–89. doi:10.1098/rstb.2011.0097. PMC 3146779. PMID 21893541.
- Roy A, Eisenhut M, Harris RJ, Rodrigues LC, Sridhar S, Habermann S, et al. (August 2014). "Effect of BCG vaccination against Mycobacterium tuberculosis infection in children: systematic review and meta-analysis". BMJ. 349: g4643. doi:10.1136/bmj.g4643. PMC 4122754. PMID 25097193.
- "Vaccine and Immunizations: TB Vaccine (BCG)". Centers for Disease Control and Prevention. 2011. Archived from the original on 17 November 2011. Retrieved 26 July 2011.
- "BCG Vaccine Usage in Canada – Current and Historical". Public Health Agency of Canada. September 2010. Archived from the original on 30 March 2012. Retrieved 30 December 2011.
- Teo SS, Shingadia DV (June 2006). "Does BCG have a role in tuberculosis control and prevention in the United Kingdom?". Archives of Disease in Childhood. 91 (6): 529–31. doi:10.1136/adc.2005.085043. PMC 2082765. PMID 16714729.
- Kashangura R, Jullien S, Garner P, Johnson S, et al. (Cochrane Infectious Diseases Group) (April 2019). "MVA85A vaccine to enhance BCG for preventing tuberculosis". The Cochrane Database of Systematic Reviews. 4: CD012915. doi:10.1002/14651858.CD012915.pub2. PMC 6488980. PMID 31038197.
- "The Global Plan to Stop TB". World Health Organization (WHO). 2011. Archived from the original on 12 June 2011. Retrieved 13 June 2011.
- Warrell DA, Cox TM, Firth JD, Benz EJ (2005). Sections 1–10 (4. ed., paperback ed.). Oxford [u.a.]: Oxford Univ. Press. p. 560. ISBN 978-0-19-857014-1. Archived from the original on 6 September 2015.
- Fraser A, Paul M, Attamna A, Leibovici L, et al. (Cochrane Infectious Diseases Group) (April 2006). "Drugs for preventing tuberculosis in people at risk of multiple-drug-resistant pulmonary tuberculosis". The Cochrane Database of Systematic Reviews (2): CD005435. doi:10.1002/14651858.CD005435.pub2. PMC 6532726. PMID 16625639.
- Brennan PJ, Nikaido H (1995). "The envelope of mycobacteria". Annual Review of Biochemistry. 64: 29–63. doi:10.1146/annurev.bi.64.070195.000333. PMID 7574484.
- Davies G, Cerri S, Richeldi L (October 2007). "Rifabutin for treating pulmonary tuberculosis". The Cochrane Database of Systematic Reviews (4): CD005159. doi:10.1002/14651858.CD005159.pub2. PMC 6532710. PMID 17943842.
- Latent tuberculosis infection. World Health Organization (WHO). 2018. p. 23. ISBN 978-92-4-155023-9.
- Borisov AS, Bamrah Morris S, Njie GJ, Winston CA, Burton D, Goldberg S, et al. (June 2018). "Update of Recommendations for Use of Once-Weekly Isoniazid-Rifapentine Regimen to Treat Latent Mycobacterium tuberculosis Infection". MMWR. Morbidity and Mortality Weekly Report. 67 (25): 723–726. doi:10.15585/mmwr.mm6725a5. PMC 6023184. PMID 29953429.
- Sterling TR, Njie G, Zenner D, Cohn DL, Reves R, Ahmed A, et al. (February 2020). "Guidelines for the Treatment of Latent Tuberculosis Infection: Recommendations from the National Tuberculosis Controllers Association and CDC, 2020". MMWR. Recommendations and Reports. 69 (1): 1–11. doi:10.15585/mmwr.rr6901a1. PMC 7041302. PMID 32053584.
- Njie GJ, Morris SB, Woodruff RY, Moro RN, Vernon AA, Borisov AS (August 2018). "Isoniazid-Rifapentine for Latent Tuberculosis Infection: A Systematic Review and Meta-analysis". American Journal of Preventive Medicine. 55 (2): 244–252. doi:10.1016/j.amepre.2018.04.030. PMC 6097523. PMID 29910114.
- Menzies D, Al Jahdali H, Al Otaibi B (March 2011). "Recent developments in treatment of latent tuberculosis infection". The Indian Journal of Medical Research. 133 (3): 257–66. PMC 3103149. PMID 21441678.
- M'imunya JM, Kredo T, Volmink J, et al. (Cochrane Infectious Diseases Group) (May 2012). "Patient education and counselling for promoting adherence to treatment for tuberculosis". The Cochrane Database of Systematic Reviews (5): CD006591. doi:10.1002/14651858.CD006591.pub2. PMC 6532681. PMID 22592714.
- Gelband H, et al. (Cochrane Infectious Diseases Group) (25 October 1999). "Regimens of less than six months for treating tuberculosis". The Cochrane Database of Systematic Reviews (2): CD001362. doi:10.1002/14651858.CD001362. PMC 6532732. PMID 10796641.
- Grace AG, Mittal A, Jain S, Tripathy JP, Satyanarayana S, Tharyan P, Kirubakaran R, et al. (Cochrane Infectious Diseases Group) (December 2019). "Shortened treatment regimens versus the standard regimen for drug-sensitive pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 12: CD012918. doi:10.1002/14651858.CD012918.pub2. PMC 6953336. PMID 31828771.
- Mainous III AB (2010). Management of Antimicrobials in Infectious Diseases: Impact of Antibiotic Resistance. Totowa, NJ: Humana Press. p. 69. ISBN 978-1-60327-238-4. Archived from the original on 6 September 2015.
- Karumbi J, Garner P (May 2015). "Directly observed therapy for treating tuberculosis". The Cochrane Database of Systematic Reviews (5): CD003343. doi:10.1002/14651858.CD003343.pub4. PMC 4460720. PMID 26022367.
- Liu Q, Abba K, Alejandria MM, Sinclair D, Balanag VM, Lansang MA, et al. (Cochrane Infectious Diseases Group) (November 2014). "Reminder systems to improve patient adherence to tuberculosis clinic appointments for diagnosis and treatment". The Cochrane Database of Systematic Reviews (11): CD006594. doi:10.1002/14651858.CD006594.pub3. PMC 4448217. PMID 25403701.
- Mwandumba HC, Squire SB, et al. (Cochrane Infectious Diseases Group) (23 October 2001). "Fully intermittent dosing with drugs for treating tuberculosis in adults". The Cochrane Database of Systematic Reviews (4): CD000970. doi:10.1002/14651858.CD000970. PMC 6532565. PMID 11687088.
- Bose A, Kalita S, Rose W, Tharyan P, et al. (Cochrane Infectious Diseases Group) (January 2014). "Intermittent versus daily therapy for treating tuberculosis in children". The Cochrane Database of Systematic Reviews (1): CD007953. doi:10.1002/14651858.CD007953.pub2. PMC 6532685. PMID 24470141.
- O'Brien RJ (June 1994). "Drug-resistant tuberculosis: etiology, management and prevention". Seminars in Respiratory Infections. 9 (2): 104–12. PMID 7973169.
- Centers for Disease Control and Prevention (CDC) (March 2006). "Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs--worldwide, 2000-2004". MMWR. Morbidity and Mortality Weekly Report. 55 (11): 301–5. PMID 16557213. Archived from the original on 22 May 2017.
- McKenna M (12 January 2012). "Totally Resistant TB: Earliest Cases in Italy". Wired. Archived from the original on 14 January 2012. Retrieved 12 January 2012.
- Migliori GB, De Iaco G, Besozzi G, Centis R, Cirillo DM (May 2007). "First tuberculosis cases in Italy resistant to all tested drugs". Euro Surveillance. 12 (5): E070517.1. doi:10.2807/esw.12.20.03194-en. PMID 17868596.
- "Totally Drug-Resistant TB: a WHO consultation on the diagnostic definition and treatment options" (PDF). World Health Organization (WHO). Archived (PDF) from the original on 21 October 2016. Retrieved 25 March 2016.
- Kielstra P (30 June 2014). Tabary Z (ed.). "Ancient enemy, modern imperative – A time for greater action against tuberculosis". Economist Intelligence Unit. Archived from the original on 31 July 2014. Retrieved 1 August 2014. Cite journal requires
|journal=(help) - Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, ZiaZarifi AH, Hoffner SE (August 2009). "Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in iran". Chest. 136 (2): 420–425. doi:10.1378/chest.08-2427. PMID 19349380.
- "Provisional CDC Guidelines for the Use and Safety Monitoring of Bedaquiline Fumarate (Sirturo) for the Treatment of Multidrug-Resistant Tuberculosis". Archived from the original on 4 January 2014.
- Singh B, Cocker D, Ryan H, Sloan DJ, et al. (Cochrane Infectious Diseases Group) (March 2019). "Linezolid for drug-resistant pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 3: CD012836. doi:10.1002/14651858.CD012836.pub2. PMC 6426281. PMID 30893466.
- Theron G, Peter J, Richardson M, Warren R, Dheda K, Steingart KR, et al. (Cochrane Infectious Diseases Group) (September 2016). "® MTBDRsl assay for resistance to second-line anti-tuberculosis drugs". The Cochrane Database of Systematic Reviews. 9: CD010705. doi:10.1002/14651858.CD010705.pub3. PMC 5034505. PMID 27605387.
- "WHO Disease and injury country estimates". World Health Organization (WHO). 2004. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- Lambert ML, Hasker E, Van Deun A, Roberfroid D, Boelaert M, Van der Stuyft P (May 2003). "Recurrence in tuberculosis: relapse or reinfection?". The Lancet. Infectious Diseases. 3 (5): 282–7. doi:10.1016/S1473-3099(03)00607-8. PMID 12726976.
- Wang JY, Lee LN, Lai HC, Hsu HL, Liaw YS, Hsueh PR, Yang PC (July 2007). "Prediction of the tuberculosis reinfection proportion from the local incidence". The Journal of Infectious Diseases. 196 (2): 281–8. doi:10.1086/518898. PMID 17570116.
- "1.4 Prognosis - Tuberculosis". medicalguidelines.msf.org. Retrieved 25 August 2020.
- "Fact Sheets: The Difference Between Latent TB Infection and Active TB Disease". Centers for Disease Control and Prevention (CDC). 20 June 2011. Archived from the original on 4 August 2011. Retrieved 26 July 2011.
- "Global tuberculosis report 2013". World Health Organization (WHO). 2013. Archived from the original on 12 December 2006.
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253.
- "Global Tuberculosis Control 2011" (PDF). World Health Organization (WHO). Archived from the original (PDF) on 17 June 2012. Retrieved 15 April 2012.
- "Tuberculosis". WHO. 24 March 2020. Retrieved 31 May 2020.
- Douglas AS, Strachan DP, Maxwell JD (1996). "Seasonality of tuberculosis: the reverse of other respiratory diseases in the UK". Thorax. 51 (9): 944–946. doi:10.1136/thx.51.9.944. PMC 472621. PMID 8984709.
- Martineau AR, Nhamoyebonde S, Oni T, Rangaka MX, Marais S, et al. (2011). "Reciprocal seasonal variation in vitamin D status and tuberculosis notifications in Cape Town, South Africa". Proc Natl Acad Sci U S A. 108 (47): 19013–19017. doi:10.1073/pnas.1111825108. PMC 3223428. PMID 22025704.
- Parrinello CM, Crossa A, Harris TG (2012). "Seasonality of tuberculosis in New York City, 1990–2007". Int J Tuberc Lung Dis. 16 (1): 32–37. doi:10.5588/ijtld.11.0145. PMID 22236842.
- Korthals Altes H, Kremer K, Erkens C, Van Soolingen D, Wallinga J (2012). "Tuberculosis seasonality in the Netherlands differs between natives and non-natives: a role for vitamin D deficiency?". Int J Tuberc Lung Dis. 16 (5): 639–644. doi:10.5588/ijtld.11.0680. PMID 22410705.
- Koh GCKW; Hawthorne G; Turner AM; Kunst H; Dedicoat M (2013). "Tuberculosis incidence correlates with sunshine: an ecological 28-year time series study". PLOS ONE. 8 (3): e57752. Bibcode:2013PLoSO...857752K. doi:10.1371/journal.pone.0057752. PMC 3590299. PMID 23483924.
- Kuddus, Md Abdul; McBryde, Emma; Adegboye, Oyelola A. (2019). "Delay effect and burden of weather-related tuberculosis cases in Rajshahi province, Bangladesh, 2007–2012". Scientific Reports. 9 (1): 12720. Bibcode:2019NatSR...912720K. doi:10.1038/s41598-019-49135-8. PMC 6722246. PMID 31481739. Retrieved 19 September 2020.
- Griffith DE, Kerr CM (August 1996). "Tuberculosis: disease of the past, disease of the present". Journal of PeriAnesthesia Nursing. 11 (4): 240–45. doi:10.1016/S1089-9472(96)80023-2. PMID 8964016.
- "Global Tuberculosis Control Report, 2006 – Annex 1 Profiles of high-burden countries" (PDF). World Health Organization (WHO). Archived from the original (PDF) on 26 July 2009. Retrieved 13 October 2006.
- "2005 Surveillance Slide Set". Centers for Disease Control and Prevention. 12 September 2006. Archived from the original on 23 November 2006. Retrieved 13 October 2006.
- FitzGerald JM, Wang L, Elwood RK (February 2000). "Tuberculosis: 13. Control of the disease among aboriginal people in Canada". Canadian Medical Association Journal. 162 (3): 351–55. PMC 1231016. PMID 10693593.
- Quah SR, Carrin G, Buse K, Heggenhougen K (2009). Health Systems Policy, Finance, and Organization. Boston: Academic Press. p. 424. ISBN 978-0-12-375087-7. Archived from the original on 6 September 2015.
- Medical Research Council.Origins of the MRC. Accessed 7 October 2006.
- Vladimir M. Shkolnikov and France Meslé. The Russian Epidemiological Crisis as Mirrored by Mortality Trends, Table 4.11, The RAND Corporation.
- Global Tuberculosis Control, World Health Organization, 2011.
- WHO global tuberculosis report 2016. Annex 2. Country profiles: Russian Federation
- "Global Tuberculosis Report 2018" (PDF). Retrieved 27 September 2019.
- WHO Global tuberculosis report 2016: India
- "Govt revisits strategy to combat tuberculosis". Daily News and Analysis. 8 April 2017.
- Mahla, RS; et al. (2021). "Prevalence of drug-resistant tuberculosis in South Africa". Tuberculosis. 18 (8): 836. doi:10.1016/S1473-3099(18)30401-8. PMID 30064674.
- Birn A (2009). Textbook of International Health: Global Health in a Dynamic World. p. 261. ISBN 978-0-19-988521-3. Archived from the original on 6 September 2015.
- "CDC Surveillance Slides 2012 – TB". Centers for Disease Control and Prevention. 24 October 2018. Archived from the original on 9 November 2013. Retrieved 17 September 2017.
- Al-Azem A, Kaushal Sharma M, Turenne C, Hoban D, Hershfield E, MacMorran J, Kabani A (1998). "Rural outbreaks of Mycobacterium tuberculosis in a Canadian province". Abstr Intersci Conf Antimicrob Agents Chemother. 38: 555. abstract no. L-27. Archived from the original on 18 November 2011.
- "Tuberculosis incidence (per 100,000 people)". Our World in Data. Retrieved 7 March 2020.
- "Tuberculosis deaths by region". Our World in Data. Retrieved 7 March 2020.
- Rothschild BM, Martin LD, Lev G, Bercovier H, Bar-Gal GK, Greenblatt C, et al. (August 2001). "Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present". Clinical Infectious Diseases. 33 (3): 305–11. doi:10.1086/321886. PMID 11438894.
- Pearce-Duvet JM (August 2006). "The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease". Biological Reviews of the Cambridge Philosophical Society. 81 (3): 369–82. doi:10.1017/S1464793106007020. PMID 16672105. S2CID 6577678.
- Comas I, Gagneux S (October 2009). Manchester M (ed.). "The past and future of tuberculosis research". PLOS Pathogens. 5 (10): e1000600. doi:10.1371/journal.ppat.1000600. PMC 2745564. PMID 19855821.
- Zink AR, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, et al. (January 2003). "Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping". Journal of Clinical Microbiology. 41 (1): 359–67. doi:10.1128/JCM.41.1.359-367.2003. PMC 149558. PMID 12517873.
- Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D (December 2002). "Detection of mycobacterial DNA in Andean mummies". Journal of Clinical Microbiology. 40 (12): 4738–40. doi:10.1128/JCM.40.12.4738-4740.2002. PMC 154635. PMID 12454182.
- Sledzik PS, Bellantoni N (June 1994). "Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief" (PDF). American Journal of Physical Anthropology. 94 (2): 269–74. doi:10.1002/ajpa.1330940210. PMID 8085617. Archived (PDF) from the original on 18 February 2017.
- Léon Charles Albert Calmette at Who Named It?
- Trail RR (April 1970). "Richard Morton (1637-1698)". Medical History. 14 (2): 166–74. doi:10.1017/S0025727300015350. PMC 1034037. PMID 4914685.
- Marten, Benjamin (1720). A New Theory of Consumptions—More Especially a Phthisis or Consumption of the Lungs. London, England: T. Knaplock. P. 51: "The Original and Essential Cause … may possibly be some certain Species of Animalcula or wonderfully minute living Creatures, … " P. 79: "It may be therefore very likely, that by an habitual lying in the same Bed with a Consumptive Patient, constantly Eating and Drinking with him, or by very frequently conversing so nearly, as to draw in part of the Breath he emits from his Lungs, a Consumption may be caught by a sound Person; … "
- Laennec, R.T.H. (1819). De l'auscultation médiate … (in French). vol. 1. Paris, France: J.-A. Brosson et J.-S Chaudé. p. 20. From p. 20: "L'existence des tubercules dans le poumon est la cause et constitue le charactère anatomique propre de la phthisie pulmonaire (a). (a) … l'effet dont cette maladie tire son nom, c'est-à-dire, la consumption." (The existence of tubercles in the lung is the cause and constitutes the unique anatomical characteristic of pulmonary tuberculosis (a). (a) … the effect from which this malady [pulmonary tuberculosis] takes its name, that is, consumption.)
- Schönlein, J.L. (1832). Allgemeine und specielle Pathologie und Therapie [General and Special Pathology and Therapy] (in German). vol. 3. Würzburg, (Germany): C. Etlinger. p. 103.
- The word "tuberculosis" first appeared in Schönlein's clinical notes in 1829. See: Jay, S. J.; Kırbıyık, U.; Woods, J. R.; Steele, G. A.; Hoyt, G. R.; Schwengber, R. B.; Gupta, P. (2018). "Modern theory of tuberculosis: culturomic analysis of its historical origin in Europe and North America". International Journal of Tuberculosis and Lung Disease. 22 (11): 1249–1257. doi:10.5588/ijtld.18.0239. PMID 30355403. See especially Appendix, p. iii.
- Kentucky: Mammoth Cave long on history. Archived 13 August 2006 at the Wayback Machine CNN. 27 February 2004. Accessed 8 October 2006.
- McCarthy OR (August 2001). "The key to the sanatoria". Journal of the Royal Society of Medicine. 94 (8): 413–17. doi:10.1177/014107680109400813. PMC 1281640. PMID 11461990.
- Villemin, J.A. (1865). "Cause et nature de la tuberculose" [Cause and nature of tuberculosis]. Bulletin de l'Académie Impériale de Médecine (in French). 31: 211–216.
- See also: Villemin, J.-A. (1868). Etudes sur la tuberculose: preuves rationnelles et expérimentales de sa spécificité et de son inoculabilité [Studies of tuberculosis: rational and experimental evidence of its specificity and inoculability] (in French). Paris, France: J.-B. Baillière et fils.
- Burdon-Sanderson, John Scott. (1870) "Introductory Report on the Intimate Pathology of Contagion." Appendix to: Twelfth Report to the Lords of Her Majesty's Most Honourable Privy Council of the Medical Officer of the Privy Council [for the year 1869], Parliamentary Papers (1870), vol. 38, 229-256.
- "History: World TB Day". Centers for Disease Control and Prevention (CDC). 12 December 2016. Archived from the original on 7 December 2018. Retrieved 23 March 2019.
- Nobel Foundation. The Nobel Prize in Physiology or Medicine 1905. Archived 10 December 2006 at the Wayback Machine Accessed 7 October 2006.
- Waddington K (January 2004). "To stamp out 'so terrible a malady': bovine tuberculosis and tuberculin testing in Britain, 1890–1939". Medical History. 48 (1): 29–48. doi:10.1017/S0025727300007043. PMC 546294. PMID 14968644.
- Bonah C (December 2005). "The 'experimental stable' of the BCG vaccine: safety, efficacy, proof, and standards, 1921–1933". Studies in History and Philosophy of Biological and Biomedical Sciences. 36 (4): 696–721. doi:10.1016/j.shpsc.2005.09.003. PMID 16337557.
- Comstock GW (September 1994). "The International Tuberculosis Campaign: a pioneering venture in mass vaccination and research". Clinical Infectious Diseases. 19 (3): 528–40. doi:10.1093/clinids/19.3.528. PMID 7811874.
- Hannaway C (2008). Biomedicine in the twentieth century: practices, policies, and politics. Amsterdam: IOS Press. p. 233. ISBN 978-1-58603-832-8. Archived from the original on 7 September 2015.
- Bloom BR (1994). Tuberculosis: pathogenesis, protection, and control. Washington, DC: ASM Press. ISBN 978-1-55581-072-6.
- Persson S (2010). Smallpox, Syphilis and Salvation: Medical Breakthroughs That Changed the World. ReadHowYouWant.com. p. 141. ISBN 978-1-4587-6712-7. Archived from the original on 6 September 2015.
- Shields T (2009). General thoracic surgery (7th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 792. ISBN 978-0-7817-7982-1. Archived from the original on 6 September 2015.
- Lalloo UG, Naidoo R, Ambaram A (May 2006). "Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis". Current Opinion in Pulmonary Medicine. 12 (3): 179–85. doi:10.1097/01.mcp.0000219266.27439.52. PMID 16582672. S2CID 24221563.
- "Frequently asked questions about TB and HIV". World Health Organization (WHO). Archived from the original on 8 August 2011. Retrieved 15 April 2012.
- Lawlor C. "Katherine Byrne, Tuberculosis and the Victorian Literary Imagination". British Society for Literature and Science. Retrieved 11 June 2017.
- "Hippocrates 3.16 Classics, MIT". Archived from the original on 11 February 2005. Retrieved 15 December 2015.CS1 maint: unfit URL (link)
- Caldwell M (1988). The Last Crusade. New York: Macmillan. p. 21. ISBN 978-0-689-11810-4.
- Bunyan J (1808). The Life and Death of Mr. Badman. London: W. Nicholson. p. 244. Retrieved 28 September 2016 – via Internet Archive.
captain.
- Byrne K (2011). Tuberculosis and the Victorian Literary Imagination. Cambridge University Press. ISBN 978-1-107-67280-2.
- "About Chopin's illness". Icons of Europe. Retrieved 11 June 2017.
- Vilaplana C (March 2017). "A literary approach to tuberculosis: lessons learned from Anton Chekhov, Franz Kafka, and Katherine Mansfield". International Journal of Infectious Diseases. 56: 283–85. doi:10.1016/j.ijid.2016.12.012. PMID 27993687.
- Rogal SJ (1997). A William Somerset Maugham Encyclopedia. Greenwood Publishing. p. 245. ISBN 978-0-313-29916-2.
- Eschner K. "George Orwell Wrote '1984' While Dying of Tuberculosis". Smithsonian. Retrieved 25 March 2019.
- "Tuberculosis (whole issue)". Journal of the American Medical Association. 293 (22): cover. 8 June 2005.
- Lemlein RF (1981). "Influence of Tuberculosis on the Work of Visual Artists: Several Prominent Examples". Leonardo. 14 (2): 114–11. doi:10.2307/1574402. JSTOR 1574402. S2CID 191371443.
- Wilsey AM (May 2012). 'Half in Love with Easeful Death:' Tuberculosis in Literature. Humanities Capstone Projects (PhD Thesis thesis). Pacific University. Archived from the original on 11 October 2017. Retrieved 28 September 2017.
- Morens DM (November 2002). "At the deathbed of consumptive art". Emerging Infectious Diseases. 8 (11): 1353–8. doi:10.3201/eid0811.020549. PMC 2738548. PMID 12463180.
- "Pulmonary Tuberculosis/In Literature and Art". McMaster University History of Diseases. Retrieved 9 June 2017.
- Thomson G (1 June 2016). "Van Morrison – 10 of the best". The Guardian.
- "Tuberculosis Throughout History: The Arts" (PDF). United States Agency for International Development (USAID). Retrieved 12 June 2017.
- Corliss R (22 December 2008). "Top 10 Worst Christmas Movies". Time.
'If you don't cry when Bing Crosby tells Ingrid Bergman she has tuberculosis', Joseph McBride wrote in 1973, 'I never want to meet you, and that's that.'
- "Public–Private Partnership Announces Immediate 40 Percent Cost Reduction for Rapid TB Test" (PDF). World Health Organization (WHO). 6 August 2012. Archived (PDF) from the original on 29 October 2013.
- Lawn SD, Nicol MP (September 2011). "Xpert® MTB/RIF assay: development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistance". Future Microbiology. 6 (9): 1067–82. doi:10.2217/fmb.11.84. PMC 3252681. PMID 21958145.
- "WHO says Cepheid rapid test will transform TB care". Reuters. 8 December 2010. Archived from the original on 11 December 2010.
- STOPTB (5 April 2013). "The Stop TB Partnership, which operates through a secretariat hosted by the World Health Organization (WHO) in Geneva, Switzerland" (PDF). Archived (PDF) from the original on 24 January 2014.
- Lienhardt C, Espinal M, Pai M, Maher D, Raviglione MC (November 2011). "What research is needed to stop TB? Introducing the TB Research Movement". PLOS Medicine. 8 (11): e1001135. doi:10.1371/journal.pmed.1001135. PMC 3226454. PMID 22140369.
- Bhargava A, Pinto L, Pai M (2011). "Mismanagement of tuberculosis in India: Causes, consequences, and the way forward" (PDF). Hypothesis. 9 (1): e7. Archived from the original on 14 March 2016.CS1 maint: unfit URL (link)
- Amdekar Y (July 2009). "Changes in the management of tuberculosis". Indian Journal of Pediatrics. 76 (7): 739–42. doi:10.1007/s12098-009-0164-4. PMID 19693453. S2CID 41788291.
- Fox GJ, Dobler CC, Marks GB (September 2011). "Active case finding in contacts of people with tuberculosis". The Cochrane Database of Systematic Reviews (9): CD008477. doi:10.1002/14651858.CD008477.pub2. PMC 6532613. PMID 21901723.
- Mhimbira FA, Cuevas LE, Dacombe R, Mkopi A, Sinclair D, et al. (Cochrane Infectious Diseases Group) (November 2017). "Interventions to increase tuberculosis case detection at primary healthcare or community-level services". The Cochrane Database of Systematic Reviews. 11: CD011432. doi:10.1002/14651858.CD011432.pub2. PMC 5721626. PMID 29182800.
- Braganza Menezes D, Menezes B, Dedicoat M, et al. (Cochrane Infectious Diseases Group) (August 2019). "Contact tracing strategies in household and congregate environments to identify cases of tuberculosis in low- and moderate-incidence populations". The Cochrane Database of Systematic Reviews. 8: CD013077. doi:10.1002/14651858.CD013077.pub2. PMC 6713498. PMID 31461540.
- Courtwright A, Turner AN (July–August 2010). "Tuberculosis and stigmatization: pathways and interventions". Public Health Reports. 125 Suppl 4 (4_suppl): 34–42. doi:10.1177/00333549101250S407. PMC 2882973. PMID 20626191.
- Mason PH, Roy A, Spillane J, Singh P (March 2016). "Social, Historical and Cultural Dimensions of Tuberculosis". Journal of Biosocial Science. 48 (2): 206–32. doi:10.1017/S0021932015000115. PMID 25997539.
- Martín Montañés C, Gicquel B (March 2011). "New tuberculosis vaccines". Enfermedades Infecciosas y Microbiologia Clinica. 29 Suppl 1: 57–62. doi:10.1016/S0213-005X(11)70019-2. PMID 21420568.
- Zhu B, Dockrell HM, Ottenhoff TH, Evans TG, Zhang Y (April 2018). "Tuberculosis vaccines: Opportunities and challenges". Respirology. 23 (4): 359–368. doi:10.1111/resp.13245. PMID 29341430.
- Ibanga HB, Brookes RH, Hill PC, Owiafe PK, Fletcher HA, Lienhardt C, et al. (August 2006). "Early clinical trials with a new tuberculosis vaccine, MVA85A, in tuberculosis-endemic countries: issues in study design". The Lancet. Infectious Diseases. 6 (8): 522–8. doi:10.1016/S1473-3099(06)70552-7. PMID 16870530.
- Kaufmann SH (October 2010). "Future vaccination strategies against tuberculosis: thinking outside the box". Immunity. 33 (4): 567–77. doi:10.1016/j.immuni.2010.09.015. PMID 21029966.
- Webber D, Kremer M (2001). "Stimulating Industrial R&D for Neglected Infectious Diseases: Economic Perspectives" (PDF). Bulletin of the World Health Organization. 79 (8): 693–801. Archived (PDF) from the original on 26 September 2007.
- Barder O, Kremer M, Williams H (2006). "Advance Market Commitments: A Policy to Stimulate Investment in Vaccines for Neglected Diseases". The Economists' Voice. 3 (3). doi:10.2202/1553-3832.1144. S2CID 154454583. Archived from the original on 5 November 2006.
- Department of Economic and Social Affairs (2009). Achieving the global public health agenda: dialogues at the Economic and Social Council. New York: United Nations. p. 103. ISBN 978-92-1-104596-3. Archived from the original on 6 September 2015.
- Jong EC, Zuckerman JN (2010). Travelers' vaccines (2nd ed.). Shelton, CT: People's Medical Publishing House. p. 319. ISBN 978-1-60795-045-5. Archived from the original on 6 September 2015.
- Bill and Melinda Gates Foundation Announcement (12 February 2004). "Gates Foundation Commits $82.9 Million to Develop New Tuberculosis Vaccines". Archived from the original on 10 October 2009.
- Nightingale K (19 September 2007). "Gates foundation gives US$280 million to fight TB". Archived from the original on 1 December 2008.
- Zumla A, Hafner R, Lienhardt C, Hoelscher M, Nunn A (March 2012). "Advancing the development of tuberculosis therapy". Nature Reviews. Drug Discovery. 11 (3): 171–2. doi:10.1038/nrd3694. PMID 22378254. S2CID 7232434.
- "J&J Sirturo Wins FDA Approval to Treat Drug-Resistant TB". Bloomberg News. 31 December 2012. Archived from the original on 4 January 2013. Retrieved 1 January 2013.
- Avorn J (April 2013). "Approval of a tuberculosis drug based on a paradoxical surrogate measure". JAMA. 309 (13): 1349–50. doi:10.1001/jama.2013.623. PMID 23430122.
- US Food and Drug Administration. "Briefing Package: NDA 204–384: Sirturo" (PDF). Archived (PDF) from the original on 4 January 2014.
- Zuckerman D, Yttri J (January 2013). "Antibiotics: When science and wishful thinking collide". Health Affairs. Archived from the original on 10 February 2013.
- Critchley JA, Orton LC, Pearson F (November 2014). "Adjunctive steroid therapy for managing pulmonary tuberculosis". The Cochrane Database of Systematic Reviews (11): CD011370. doi:10.1002/14651858.CD011370. PMC 6532561. PMID 25387839.
- Shivaprasad HL, Palmieri C (January 2012). "Pathology of mycobacteriosis in birds". The Veterinary Clinics of North America. Exotic Animal Practice. 15 (1): 41–55, v–vi. doi:10.1016/j.cvex.2011.11.004. PMID 22244112.
- Reavill DR, Schmidt RE (January 2012). "Mycobacterial lesions in fish, amphibians, reptiles, rodents, lagomorphs, and ferrets with reference to animal models". The Veterinary Clinics of North America. Exotic Animal Practice. 15 (1): 25–40, v. doi:10.1016/j.cvex.2011.10.001. PMID 22244111.
- Mitchell MA (January 2012). "Mycobacterial infections in reptiles". The Veterinary Clinics of North America. Exotic Animal Practice. 15 (1): 101–11, vii. doi:10.1016/j.cvex.2011.10.002. PMID 22244116.
- Wobeser, Gary A. (2006). Essentials of disease in wild animals (1st ed.). Ames, IO [u.a.]: Blackwell Publishing. p. 170. ISBN 978-0-8138-0589-4. Archived from the original on 6 September 2015.
- Ryan TJ, Livingstone PG, Ramsey DS, de Lisle GW, Nugent G, Collins DM, et al. (February 2006). "Advances in understanding disease epidemiology and implications for control and eradication of tuberculosis in livestock: the experience from New Zealand". Veterinary Microbiology. 112 (2–4): 211–19. doi:10.1016/j.vetmic.2005.11.025. PMID 16330161.
- White PC, Böhm M, Marion G, Hutchings MR (September 2008). "Control of bovine tuberculosis in British livestock: there is no 'silver bullet'". Trends in Microbiology. 16 (9): 420–7. CiteSeerX 10.1.1.566.5547. doi:10.1016/j.tim.2008.06.005. PMID 18706814.
- Ward AI, Judge J, Delahay RJ (January 2010). "Farm husbandry and badger behaviour: opportunities to manage badger to cattle transmission of Mycobacterium bovis?". Preventive Veterinary Medicine. 93 (1): 2–10. doi:10.1016/j.prevetmed.2009.09.014. PMID 19846226.
- Holt N (24 March 2015). "The Infected Elephant in the Room". Slate. Archived from the original on 14 April 2016. Retrieved 5 April 2016.
- Mikota SK. "A Brief History of TB in Elephants" (PDF). Animal and Plant Health Inspection Service (APHIS). Archived (PDF) from the original on 6 October 2016. Retrieved 5 April 2016.
External links
- Tuberculosis at Curlie
- "Tuberculosis (TB)". Centers for Disease Control and Prevention (CDC). 24 October 2018.
- "Tuberculosis (TB)". London: Health Protection Agency. Archived from the original on 5 July 2007.
- WHO global 2016 TB report (infographic)
- WHO tuberculosis country profiles
- Tuberculosis Among African Americans, 1990-11-01, In Black America; KUT Radio, American Archive of Public Broadcasting (WGBH and the Library of Congress)
| Classification | |
|---|---|
| External resources |

%252C_OWID.svg.png.webp)