Exercise-induced bronchoconstriction
Exercise-induced asthma, or E.I.A., occurs when the airways narrow as a result of exercise. The preferred term for this condition is exercise-induced bronchoconstriction (EIB); exercise does not cause asthma, but is frequently an asthma trigger.[1]
| Exercise-induced asthma | |
|---|---|
| Other names | EIA |
| Specialty | Pulmonology |
It might be expected that people with E.I.B. would present with shortness of breath, and/or an elevated respiratory rate and wheezing, consistent with an asthma attack. However, many will present with decreased stamina, or difficulty in recovering from exertion compared to team members, or paroxysmal coughing from an irritable airway.[2] Similarly, examination may reveal wheezing and prolonged expiratory phase, or may be quite normal. Consequently, a potential for under-diagnosis exists. Measurement of airflow, such as peak expiratory flow rates, which can be done inexpensively on the track or sideline, may prove helpful. In athletes, symptoms of bronchospasm such as chest discomfort, breathlessness, and fatigue are often falsely attributed to the individual being “out of shape”, having asthma, or possessing a hyperreactive airway rather than E.I.B. [3]
Cause
While the potential triggering events for E.I.B. are well recognized, the underlying pathogenesis is poorly understood.[4] It usually occurs after at least several minutes of vigorous, aerobic activity, which increases oxygen demand to the point where breathing through the nose (nasal breathing) must be supplemented by mouth breathing. The resultant inhalation of air that has not been warmed and humidified by the nasal passages seems to generate increased blood flow to the linings of the bronchial tree, resulting in edema. Constriction of these small airways then follows, worsening the degree of obstruction to airflow. There is increasing evidence that the smooth muscle that lines the airways becomes progressively more sensitive to changes that occur as a result of injury to the airways from dehydration. The chemical mediators that provoke the muscle spasm appear to arise from mast cells.[4]
Diagnosis
Exercise-induced bronchoconstriction can be difficult to diagnose clinically given the lack of specific symptoms[2] and frequent misinterpretation as manifestations of vigorous exercise. There are many mimics that present with similar symptoms, such as vocal cord dysfunction, cardiac arrhythmias, cardiomyopathies, and gastroesophageal reflux disease. It is also important to distinguish those who have asthma with exercise worsening, and who consequently will have abnormal testing at rest, from true exercise-induced bronchoconstriction, where there will be normal baseline results. Because of the wide differential diagnosis of exertional respiratory complaints, the diagnosis of exercise-induced bronchoconstriction based on history and self-reported symptoms alone has been shown to be inaccurate [5][6] and will result in an incorrect diagnosis more than 50% of the time.[7] An important and often over-looked differential diagnosis is exercise-induced laryngeal obstruction EILO. The latter can co-exist with EIB and is best differentiated using objective testing and continuous laryngoscopy during exercise (CLE) testing.
Spirometry
Objective testing should begin with spirometry at rest. In true exercise-induced bronchoconstriction, the results should be within normal limits. Should resting values be abnormal, then asthma, or some other chronic lung condition, is present. There is, of course, no reason why asthma and exercise-induced bronchoconstriction should not co-exist but the distinction is important because without successful treatment of underlying asthma, treatment of an exercise component will likely be unsuccessful. If baseline testing is normal, some form of exercise or pharmacologic stress will be required, either on the sideline or practice venue, or in the laboratory.[8]
Exercise testing
Treadmill or ergometer-based testing in lung function laboratories are effective methods for diagnosing exercise-induced bronchoconstriction, but may result in false negatives if the exercise stimulus is not intense enough.
Field-exercise challenge
Field-exercise challenge tests that involve the athlete performing the sport in which they are normally involved and assessing FEV1 after exercise are helpful if abnormal but have been shown to be less sensitive than eucapnic voluntary hyperventilation.[9]
Eucapnic voluntary hyperventilation challenge
The International Olympic Committee recommends the eucapnic voluntary hyperventilation (EVH) challenge as the test to document exercise-induced asthma in Olympic athletes.[10] In the EVH challenge, the patient voluntarily, without exercising, rapidly breathes dry air enriched with 5% CO
2 for six minutes. The presence of the enriched CO
2 compensates for the CO
2 losses in the expired air, not matched by metabolic production, that occurs during hyperventilation, and so maintains CO
2 levels at normal.[11]
Medication challenge
Medication challenge tests, such as the methacholine challenge test, have a lower sensitivity for detection of exercise-induced bronchoconstriction in athletes and are also not a recommended first-line approach in the evaluation of exercise-induced asthma.[12]
Mannitol inhalation[13][14] has been recently approved for use in the United States.
A relatively recent review of the literature has concluded that there is currently insufficient available evidence to conclude that either mannitol inhalation or eucapnic voluntary hyperventilation are suitable alternatives to exercise challenge testing to detect exercise-induced bronchoconstriction and that additional research is required.[15]
Treatment
Lifestyle
The best treatment is avoidance of conditions predisposing to attacks, when possible. In athletes who wish to continue their sport or do so in adverse conditions, preventive measures include altered training techniques and medications.
Some take advantage of the refractory period by precipitating an attack by "warming up," and then timing competition such that it occurs during the refractory period. Step-wise training works in a similar fashion. Warm up occurs in stages of increasing intensity, using the refractory period generated by each stage to reach a full workload.[16]
Medication
The treatment of EIB has been extensively studied in asthmatic subjects over the last 30 years, but not so in EIB. Thus, it is not known whether athletes with EIB or ‘sports asthma’ respond similarly to subjects with classical allergic or nonallergic asthma. However, there is no evidence supporting different treatment for EIB in asthmatic athletes and nonathletes.[17]
The most common medication used is a beta agonist taken about 20 minutes before exercise.[17] Some physicians prescribe inhaled anti-inflammatory mists such as corticosteroids or leukotriene antagonists, and mast cell stabilizers have also proven effective.[17] A randomized crossover study compared oral montelukast with inhaled salmeterol, both given two hours before exercise. Both drugs had similar benefit but montelukast lasted 24 hours.[18]
Three randomized double-blind cross-over trials have examined the effect of vitamin C on EIB.[19] Pooling the results of the three vitamin C trials indicates an average 48% reduction in the FEV1 decline caused by exercise (Figure). The systematic review concluded that "given the safety and low cost of vitamin C, and the positive findings for vitamin C administration in the three EIB studies, it seems reasonable for physically active people to test vitamin C when they have respiratory symptoms such as cough associated with exercise."[19] It should be acknowledged that the total number of subjects involved in all three trials was only 40.
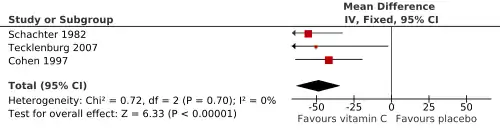
Figure: This forest plot shows the effect of vitamin C (0.5–2 g/day) on post-exercise decline in FEV1 in three studies with asthmatic participants. Constructed from data in Fig. 4 of Hemilä (2013).[19] The three horizontal lines indicate the three studies, and the diamond shape at the bottom indicates the pooled effect of vitamin C: decrease in the post-exercise decline in FEV1 by 48% (95%CI: 33 to 64%).
In May 2013, the American Thoracic Society issued the first treatment guidelines for EIB.[20]
Prognosis
As evidenced by many professional athletes who have overcome EIB using some combination of accepted treatments, the prognosis is usually very good. Olympic swimmers Tom Dolan, Amy Van Dyken, and Nancy Hogshead, Olympic track star Jackie Joyner-Kersee, baseball Hall of Famer Catfish Hunter, and American football player Jerome Bettis are among the many who have done so. Tour de France winner Chris Froome reported that he suffers from the condition, after being spotted using a nasal inhaler during race.[21] Other athletes with EIB include racing cyclist Simon Yates, distance runner Paula Radcliffe[22] and cross-country skier Marit Bjørgen.[23] Research by sports scientist John Dickinson found that 70 percent of UK-based members of the British swimming team had some form of asthma, as did a third of Team Sky cyclists, compared to a national asthma rate of eight to ten percent,[22] whilst a study by the United States Olympic Committee in 2000 found that half of cross-country skiers had EIB.[23]
References
- Khan, DA (Jan–Feb 2012). "Exercise-induced bronchoconstriction: burden and prevalence". Allergy and Asthma Proceedings. 33 (1): 1–6. doi:10.2500/aap.2012.33.3507. PMID 22370526.
- Parsons JP, Cosmar D, Phillips G, Kaeding C, Best TM, Mastronarde JG (March 2012). "Screening for exercise-induced bronchoconstriction in college athletes". J Asthma. 49 (2): 153–7. doi:10.3109/02770903.2011.652329. PMC 3832203. PMID 22276571.
- Parsons JP, Mastronarde JG (24 December 2015). "Exercise-Induced Bronchoconstriction in Athletes". Chest. 128 (6): 3966-3974. doi:10.1016/S0012-3692(15)49641-2. Retrieved 28 November 2020.
- Anderson SD, Kippelen P (March 2005). "Exercise-induced bronchoconstriction: Pathogenesis". Current Allergy and Asthma Reports. 5 (2): 116–22. doi:10.1007/s11882-005-0084-y. PMID 15683611.
- Hallstrand TS, Curtis JR, Koepsell TD, et al. (September 2002). "Effectiveness of screening examinations to detect unrecognized exercise-induced bronchoconstriction". J. Pediatr. 141 (3): 343–8. doi:10.1067/mpd.2002.125729. PMID 12219053.
- Rundell KW, Im J, Mayers LB, Wilber RL, Szmedra L, Schmitz HR (February 2001). "Self-reported symptoms and exercise-induced asthma in the elite athlete". Med Sci Sports Exerc. 33 (2): 208–13. doi:10.1097/00005768-200102000-00006. PMID 11224807.
- Parsons JP, Kaeding C, Phillips G, Jarjoura D, Wadley G, Mastronarde JG (September 2007). "Prevalence of exercise-induced bronchospasm in a cohort of varsity college athletes". Med Sci Sports Exerc. 39 (9): 1487–92. doi:10.1249/mss.0b013e3180986e45. PMID 17805078.
- Carlsen KH, Anderson SD, Bjermer L, et al. (April 2008). "Exercise-induced asthma, respiratory and allergic disorders in elite athletes: epidemiology, mechanisms and diagnosis: Part I of the report from the Joint Task Force of the European Respiratory Society (ERS) and the European Academy of Allergy and Clinical Immunology (EAACI) in cooperation with GA2LEN". Allergy. 63 (4): 387–403. doi:10.1111/j.1398-9995.2008.01662.x. PMID 18315727.
- Mannix ET, Manfredi F, Farber MO (1999). "A comparison of two challenge tests for identifying exercise-induced bronchospasm in figure skaters". Chest. 115 (3): 649–53. doi:10.1378/chest.115.3.649. PMID 10084470. S2CID 2599863.
- Douglas B. McKeag; James L. Moeller; American College of Sports Medicine (3 July 2007). ACSM's Primary Care Sports Medicine. Lippincott Williams & Wilkins. p. 167. ISBN 978-0-7817-7028-6. Retrieved 21 April 2012.
- Rosenthal, Richard. "Eucapnic Voluntary Hyperventilation (EVH) A Test for the Presence of Asthma". Archived from the original on 2014-05-31. Retrieved 2014-05-30.
- Weiler JM, Bonini S, Coifman R, Craig T, Delgado L, Capão-Filipe M, et al. (2007). "American Academy of Allergy, Asthma & Immunology Work Group report: exercise-induced asthma". J Allergy Clin Immunol. 119 (6): 1349–58. doi:10.1016/j.jaci.2007.02.041. PMID 17433829.
- Brannan JD, Koskela H, Anderson SD, Chew N (1998). "Responsiveness to mannitol in asthmatic subjects with exercise- and hyperventilation-induced asthma". Am J Respir Crit Care Med. 158 (4): 1120–6. doi:10.1164/ajrccm.158.4.9802087. PMID 9769270.
- Muñoz PA, Gómez FP, Manrique HA, Roca J, Barberà JA, Young IH, et al. (2008). "Pulmonary gas exchange response to exercise- and mannitol-induced bronchoconstriction in mild asthma". J Appl Physiol. 105 (5): 1477–85. doi:10.1152/japplphysiol.00108.2008. PMID 18756011. S2CID 17712937.
- Stickland MK, Rowe BH, Spooner CH, Vandermeer B, Dryden DM (September 2011). "Accuracy of eucapnic hyperpnea or mannitol to diagnose exercise-induced bronchoconstriction: a systematic review". Ann Allergy Asthma Immunol. 107 (3): 229–34. doi:10.1016/j.anai.2011.06.013. PMID 21875541.
- Stickland MK, Rowe BH, Spooner CH, Vandermeer B, Dryden DM (March 2012). "Effect of warm-up exercise on exercise-induced bronchoconstriction". Med Sci Sports Exerc. 44 (3): 383–91. doi:10.1249/MSS.0b013e31822fb73a. PMID 21811185. S2CID 343413.
- Carlsen KH, Anderson SD, Bjermer L, et al. (April 2008). "Treatment of exercise-induced asthma, respiratory and allergic disorders in sports and the relationship to doping: Part II of the report from the Joint Task Force of European Respiratory Society (ERS) and European Academy of Allergy and Clinical Immunology (EAACI) in cooperation with GA2LEN". Allergy. 63 (4): 492–505. doi:10.1111/j.1398-9995.2008.01663.x. PMID 18394123.
- Philip G, Pearlman DS, Villarán C, et al. (2007). "Single-dose montelukast or salmeterol as protection against exercise-induced bronchoconstriction". Chest. 132 (3): 875–83. doi:10.1378/chest.07-0550. PMID 17573489.
- Hemilä, H (7 June 2013). "Vitamin C may alleviate exercise-induced bronchoconstriction: a meta-analysis". BMJ Open. 3 (6): e002416. doi:10.1136/bmjopen-2012-002416. PMC 3686214. PMID 23794586.

- Parsons JP, Hallstrand TS, Mastronarde JG, et al. (May 2013). "An official American Thoracic Society clinical practice guideline: exercise-induced bronchoconstriction". Am. J. Respir. Crit. Care Med. 187 (9): 1016–27. doi:10.1164/rccm.201303-0437ST. PMID 23634861. S2CID 32941118.
- "Froome surprised at controversy over in-race inhaler use".
- Walker, Peter (29 April 2016). "Why do so many elite athletes have asthma?". theguardian.com. Retrieved 29 April 2016.
- Gardner, Amanda (17 February 2010). "For Olympians and weekend warriors, winter sports can trigger asthma". cnn.com. Retrieved 29 April 2016.
External links
- "Tips to Remember: Exercise-induced asthma". American Academy of Allergy, Asthma, and Immunology. Retrieved 2007-04-12.
- Fact sheet: Exercise-induced asthma
| Classification | |
|---|---|
| External resources |