Respiratory failure
Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide or both cannot be kept at normal levels. A drop in the oxygen carried in blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be either acute or chronic. The definition of respiratory failure in clinical trials usually includes increased respiratory rate, abnormal blood gases (hypoxemia, hypercapnia, or both), and evidence of increased work of breathing. Respiratory failure causes an altered mental status due to ischemia in the brain.[1]
| Respiratory failure | |
|---|---|
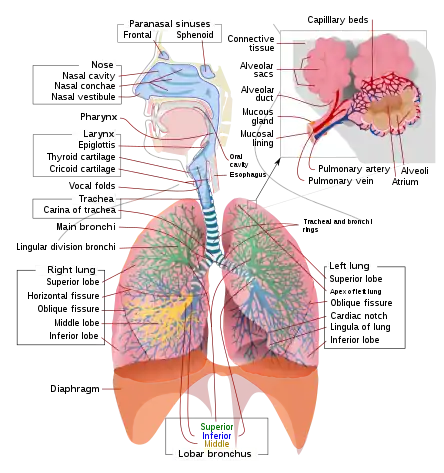 | |
| Respiratory system | |
| Specialty | Pulmonology, Intensive care medicine |
The normal partial pressure reference values are: oxygen Pa O2 more than 80 mmHg (11 kPa), and carbon dioxide Pa CO2 less than 45 mmHg (6.0 kPa). [2]
Cause
Several types of conditions can potentially result in respiratory failure:
- Conditions which reduce the flow of air into and out of the lungs, including physical obstruction by foreign bodies or masses, and reduced breathing ability due to drugs or changes to the chest.
- Conditions that impair the lungs' blood supply. These include thromboembolic conditions and conditions that reduce the output of the right heart, such as right heart failure and some myocardial infarctions.
- Conditions which limit the ability of the lung tissue to exchange oxygen and carbon dioxide between the blood and the air within the lungs. Any disease which can damage the lung tissue can fit into this category. The most common causes are (in no particular order) infections, interstitial lung disease, and pulmonary oedema.
Diagnosis
Type 1
Type 1 respiratory failure is defined as a low level of oxygen in the blood (hypoxemia) with either a normal (normocapnia) or low (hypocapnia) level of carbon dioxide (PaCO2) but not an increased level (hypercapnia). It is typically caused by a ventilation/perfusion (V/Q) mismatch; the volume of air flowing in and out of the lungs is not matched with the flow of blood to the lungs. The basic defect in type 1 respiratory failure is failure of oxygenation characterized by:
PaO2 decreased (< 60 mmHg (8.0 kPa)) PaCO2 normal or decreased (<50 mmHg (6.7 kPa)) PA-aO2 increased
This type of respiratory failure is caused by conditions that affect oxygenation such as:
- Low ambient oxygen (e.g. at high altitude)
- Ventilation-perfusion mismatch (parts of the lung receive oxygen but not enough blood to absorb it, e.g. pulmonary embolism)
- Alveolar hypoventilation (decreased minute volume due to reduced respiratory muscle activity, e.g. in acute neuromuscular disease); this form can also cause type 2 respiratory failure if severe
- Diffusion problem (oxygen cannot enter the capillaries due to parenchymal disease, e.g. in pneumonia or ARDS)
- Shunt (oxygenated blood mixes with non-oxygenated blood from the venous system, e.g. right to left shunt)
Type 2
Hypoxemia (PaO2 <8kPa or normal) with hypercapnia (PaCO2 >6.0kPa).
The basic defect in type 2 respiratory failure is characterized by:
PaO2 decreased (< 60 mmHg (8.0 kPa))or normal PaCO2 increased (> 50 mmHg (6.7 kPa)) PA-aO2 normal pH <7.35
Type 2 respiratory failure is caused by inadequate alveolar ventilation; both oxygen and carbon dioxide are affected. Defined as the buildup of carbon dioxide levels (PaCO2) that has been generated by the body but cannot be eliminated. The underlying causes include:
- Increased airways resistance (chronic obstructive pulmonary disease, asthma, suffocation)
- Reduced breathing effort (drug effects, brain stem lesion, extreme obesity)
- A decrease in the area of the lung available for gas exchange (such as in chronic bronchitis)
- Neuromuscular problems (Guillain–Barré syndrome,[3] motor neuron disease)
- Deformed (kyphoscoliosis), rigid (ankylosing spondylitis), or flail chest.[3]
Treatment
Treatment of the underlying cause is required, if possible. This may involve medication such as bronchodilators (for airways disease), antibiotics (for infections), glucocorticoids (for numerous causes), diuretics (for pulmonary edema), amongst others. Respiratory failure resulting from an overdose of opioids may be treated with the antidote naloxone. In contrast, most benzodiazepine overdose does not benefit from its antidote, flumazenil.[7] Respiratory therapy/respiratory physiotherapy may be beneficial in some causes of respiratory failure.
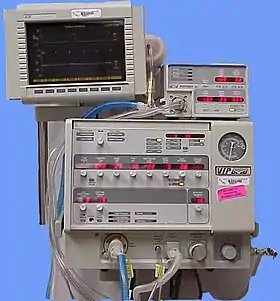
Type 1 respiratory failure may require oxygen therapy to achieve adequate oxygen saturations.[8] Lack of response to oxygen may be an indication for other modalities such as heated humidified high-flow therapy, continuous positive airway pressure or (if severe) endotracheal intubation and mechanical ventilation.
Type 2 respiratory failure often requires non-invasive ventilation (NIV), unless medical therapy can improve the situation.[9] Mechanical ventilation is sometimes indicated immediately, or otherwise if NIV fails.[9] Respiratory stimulants such as doxapram are now rarely used.[10]
There is tentative evidence that in those with respiratory failure identified before arrival in hospital, continuous positive airway pressure can be useful when started before conveying to hospital.[11]
References
- Tulaimat, A; Patel, A; Wisniewski, M; Gueret, R (August 2016). "The validity and reliability of the clinical assessment of increased work of breathing in acutely ill patients". Journal of Critical Care. 34: 111–5. doi:10.1016/j.jcrc.2016.04.013. PMID 27288621.
- "Respiratory Failure".
- Burt, Christiana C.; Arrowsmith, Joseph E. (1 November 2009). "Respiratory failure". Surgery (Oxford). 27 (11): 475–479. doi:10.1016/j.mpsur.2009.09.007.
- https://www.thoracic.org/professionals/clinical-resources/critical-care/clinical-education/mechanical-ventilation/respiratory-failure-mechanical-ventilation.pdf
- https://www.physio-pedia.com/Respiratory_Failure
- https://www.mcgill.ca/criticalcare/teaching/files/acute
- Sivilotti, Marco L.A. (March 2016). "Flumazenil, naloxone and the 'coma cocktail'". British Journal of Clinical Pharmacology. 81 (3): 428–436. doi:10.1111/bcp.12731. PMC 4767210. PMID 26469689.
- O'Driscoll, B R; Howard, L S; Earis, J; Mak, V (May 2017). "British Thoracic Society Guideline for oxygen use in adults in healthcare and emergency settings". BMJ Open Respiratory Research. 4 (1): e000170. doi:10.1136/bmjresp-2016-000170. PMC 5531304. PMID 28883921.
- Rochwerg, Bram; Brochard, Laurent; Elliott, Mark W.; Hess, Dean; Hill, Nicholas S.; Nava, Stefano; Navalesi, Paolo; Antonelli, Massimo; Brozek, Jan (August 2017). "Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure". European Respiratory Journal. 50 (2): 1602426. doi:10.1183/13993003.02426-2016. PMID 28860265.
- Greenstone, M.; Lasserson, T. J. (2003). "Doxapram for ventilatory failure due to exacerbations of chronic obstructive pulmonary disease". The Cochrane Database of Systematic Reviews (1): CD000223. doi:10.1002/14651858.CD000223. PMID 12535393.
- Bakke, SA; Botker, MT; Riddervold, IS; Kirkegaard, H; Christensen, EF (22 November 2014). "Continuous positive airway pressure and noninvasive ventilation in prehospital treatment of patients with acute respiratory failure: a systematic review of controlled studies". Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 22 (1): 69. doi:10.1186/s13049-014-0069-8. PMC 4251922. PMID 25416493.
External links
| Classification | |
|---|---|
| External resources |