Exhaled nitric oxide
In medicine, exhaled nitric oxide (eNO) can be measured in a breath test for asthma or other conditions characterized by airway inflammation. Nitric oxide (NO) is a gaseous molecule produced by certain cell types in an inflammatory response. The fraction of exhaled NO (FENO) is a promising biomarker for the diagnosis, follow-up and as a guide to therapy in adults and children with asthma. The breath test has recently become available in many well-equipped hospitals in developed countries, although its exact role remains unclear.
Biology
In humans, nitric oxide is produced from L-arginine by three enzymes called nitric oxide synthases (NOS): inducible (iNOS), endothelial (eNOS), and neuronal (nNOS). The latter two are constantly active in endothelial cells and neurons respectively, whereas iNOS' action can be induced in states like inflammation (for example, by cytokines). In inflammation, several cells use iNOS to produce NO, including eosinophils. As such, eNO (also known as FeNO "fractional exhaled nitric oxide") has been dubbed an inflammometer.[1]
Although iNOS is thought to be the main contributor to exhaled NO in asthmatics,[2][3] studies in mice also point to a role for nNOS.[4][5]
It was initially thought that exhaled NO derived mostly from the sinuses, which contain high levels of NO. It has subsequently been shown that the lower airways contribute most of the exhaled NO, and that contamination from the sinuses is minimal.
Medical use
Asthma
Patients with asthma have higher eNO levels than other people. Their levels also rise together with other clinical and laboratory parameters of asthma (for example, the amount of eosinophils in their sputum). In conditions that trigger inflammation such as upper respiratory tract infections or the inhalation of allergens or plicatic acid, eNO levels rise.[6][7] The eNO levels also tend to vary according to the results of lung function test results such as the degree of bronchial hyperresponsiveness. Furthermore, drugs used to treat asthma (such as inhaled glucocorticoids or leukotriene receptor antagonists) also reduce eNO levels.
Clinical trials have looked at whether tailoring asthma therapy based on eNO values is better than conventional care, in which therapy is gauged by symptoms and the results of lung function tests.[8][9][10] To date, the results in both adults and children have been modest and this technique can not be universally recommended.[11][12] It has also been noted that factors other than inflammation can increase eNO levels, for example airway acidity.[13][14]
The fraction of eNO has been found to be a better test to identify asthmatics than basic lung function testing (for airway obstruction). Its specificity is comparable to bronchial challenge testing, although less sensitive.[15][16] This means that a positive eNO test might be useful to rule in a diagnosis of asthma; however, a negative test might not be as useful to rule it out.[17]
Other conditions
The role for eNO in other conditions is even less well established compared to asthma.
Since asthma can be a cause of chronic coughing (it may even be the sole manifestation, such as in cough-variant asthma), studies have looked at whether eNO can be used in the diagnosis of chronic cough.[18][19][20][21]
Exhaled NO is minimally increased in chronic obstructive pulmonary disease, but levels may rise in sudden worsenings of the disease (acute exacerbations) or disease progression. Early findings indicate a possible role for eNO in predicting the response to inhaled glucocorticoids and the degree of airway obstruction reversibility.
Children with cystic fibrosis have been found to have low eNO levels. In subjects with bronchiectasis (a state of localized, irreversible dilatation of part of the bronchial tree) not due to cystic fibrosis, high levels have been found. Sarcoidosis could also feature increased eNO. Low levels have been found in primary ciliary dyskinesia, bronchopulmonary dysplasia, and pulmonary arterial hypertension. In the latter condition, inhaled NO is used as a diagnostic test of the response of the pulmonary arteries to vasodilators (agents that relax the blood vessels).
eNO has also been associated with wheeze, rhinitis and nasal allergy in primary school children.[22]
Exposure to air pollution has been associated with decreased,[23] and increased eNO levels.[24][25][26]
Measurement techniques

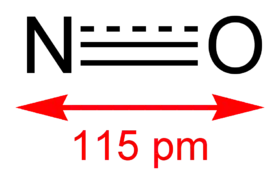
The most widely used technique to measure eNO is with a chemical reaction that produces light; this is called a chemiluminescence reaction. The NO in the breath sample reacts with ozone to form nitrogen dioxide in an excited state. When this returns to its ground state, it emits light in quantities that are proportional to the amount of exhaled NO.

The subject can exhale directly into a measurement device ('online' technique), or into a reservoir that can afterwards be connected to the analyser ('offline' technique).[27] With the former technique, the early and later NO in the breath sample can be analysed separately. The test requires little coordination from the subject, and children older than 4 can be tested successfully.[28][29]
The National Institute of Clinical Excellence (NICE) in the UK have published guidance on available measuring devices: https://www.nice.org.uk/guidance/dg12
Reference range
The upper normal level of eNO in different studies ranges from 20 to 30 parts per billion. However, several major features influence the reference values. Men have higher eNO values than women. Smoking notoriously lowers eNO values, and even former smoking status can influence results. The levels are higher in people with an atopic constitution (a tendency towards allergies).[30] The fraction of eNO is also flow-dependent (higher at lower flow rates and vice versa), so measurements are normally measured at 50 ml/s. Age or height could also considerably confound eNO values in children.[28] The magnitude of these effects lies in the order of 10%, so even single cut-off values might be useful.[17]
History
Until the 1980s, nitric oxide, a product of fossil fuel combustion, was thought only to play a role the detrimental effects of air pollution on the respiratory tract.[17] In 1987, experiments with coronary arteries showed that nitric oxide was the long sought endothelium-derived relaxing factor. After scientists realised that NO played a biological role, its role as a cell signalling molecule and neurotransmitter became clear from abundant studies.[31]
NO was first detected in exhaled breath samples in 1991.[32] In 1992, NO was voted molecule of the year by the scientific journal Science.[33] In 1993, researchers from the Karolinska Institute in Sweden were the first to report increased eNO in asthmatics.[34]
Today, NO is not only used in breath tests but also as a therapeutic agent for conditions such as pulmonary arterial hypertension and possibly for the acute respiratory distress syndrome.
Footnotes
- Pijnenburg MW, De Jongste JC (February 2008). "Exhaled nitric oxide in childhood asthma: a review". Clinical and Experimental Allergy. 38 (2): 246–59. doi:10.1111/j.1365-2222.2007.02897.x. PMID 18076708.
- Lane C, Knight D, Burgess S, Franklin P, Horak F, Legg J, et al. (September 2004). "Epithelial inducible nitric oxide synthase activity is the major determinant of nitric oxide concentration in exhaled breath". Thorax. 59 (9): 757–60. doi:10.1136/thx.2003.014894. PMC 1747143. PMID 15333851.
- Brindicci C, Ito K, Barnes PJ, Kharitonov SA (August 2007). "Effect of an inducible nitric oxide synthase inhibitor on differential flow-exhaled nitric oxide in asthmatic patients and healthy volunteers". Chest. 132 (2): 581–8. doi:10.1378/chest.06-3046. PMID 17550932. Archived from the original on 2013-04-14.
- De Sanctis GT, MacLean JA, Hamada K, Mehta S, Scott JA, Jiao A, et al. (May 1999). "Contribution of nitric oxide synthases 1, 2, and 3 to airway hyperresponsiveness and inflammation in a murine model of asthma". The Journal of Experimental Medicine. 189 (10): 1621–30. doi:10.1084/jem.189.10.1621. PMC 2193630. PMID 10330441.
- De Sanctis GT, Mehta S, Kobzik L, Yandava C, Jiao A, Huang PL, Drazen JM (October 1997). "Contribution of type I NOS to expired gas NO and bronchial responsiveness in mice". The American Journal of Physiology. 273 (4): L883-8. doi:10.1152/ajplung.1997.273.4.L883. PMID 9357865.
- Vahlkvist S, Sinding M, Skamstrup K, Bisgaard H (June 2006). "Daily home measurements of exhaled nitric oxide in asthmatic children during natural birch pollen exposure". The Journal of Allergy and Clinical Immunology. 117 (6): 1272–6. doi:10.1016/j.jaci.2006.03.018. PMID 16750986.
- Obata H, Dittrick M, Chan H, Chan-Yeung M (March 1999). "Sputum eosinophils and exhaled nitric oxide during late asthmatic reaction in patients with western red cedar asthma". The European Respiratory Journal. 13 (3): 489–95. doi:10.1183/09031936.99.13348999. PMID 10232414.
- Smith AD, Cowan JO, Brassett KP, Herbison GP, Taylor DR (May 2005). "Use of exhaled nitric oxide measurements to guide treatment in chronic asthma". The New England Journal of Medicine. 352 (21): 2163–73. doi:10.1056/NEJMoa043596. PMID 15914548. S2CID 42351261.
- Shaw DE, Berry MA, Thomas M, Green RH, Brightling CE, Wardlaw AJ, Pavord ID (August 2007). "The use of exhaled nitric oxide to guide asthma management: a randomized controlled trial". American Journal of Respiratory and Critical Care Medicine. 176 (3): 231–7. doi:10.1164/rccm.200610-1427OC. PMID 17496226. S2CID 22186959.
- Szefler SJ, Mitchell H, Sorkness CA, Gergen PJ, O'Connor GT, Morgan WJ, et al. (September 2008). "Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults: a randomised controlled trial". Lancet. 372 (9643): 1065–72. doi:10.1016/S0140-6736(08)61448-8. PMC 2610850. PMID 18805335.
- Petsky HL, Kew KM, Turner C, Chang AB (September 2016). Cochrane Airways Group (ed.). "Exhaled nitric oxide levels to guide treatment for adults with asthma". The Cochrane Database of Systematic Reviews. 9: CD011440. doi:10.1002/14651858.CD011440.pub2. PMC 6457753. PMID 27580628.
- Petsky HL, Kew KM, Chang AB (November 2016). Cochrane Airways Group (ed.). "Exhaled nitric oxide levels to guide treatment for children with asthma". The Cochrane Database of Systematic Reviews. 11: CD011439. doi:10.1002/14651858.CD011439.pub2. PMC 6432844. PMID 27825189.
- Hunt JF, Fang K, Malik R, Snyder A, Malhotra N, Platts-Mills TA, Gaston B (March 2000). "Endogenous airway acidification. Implications for asthma pathophysiology". American Journal of Respiratory and Critical Care Medicine. 161 (3 Pt 1): 694–9. doi:10.1164/ajrccm.161.3.9911005. PMID 10712309.
- Shin HW, Shelley DA, Henderson EM, Fitzpatrick A, Gaston B, George SC (March 2007). "Airway nitric oxide release is reduced after PBS inhalation in asthma". Journal of Applied Physiology. 102 (3): 1028–33. doi:10.1152/japplphysiol.01012.2006. PMID 17110506. S2CID 16813706.
- Malmberg LP, Pelkonen AS, Haahtela T, Turpeinen M (June 2003). "Exhaled nitric oxide rather than lung function distinguishes preschool children with probable asthma". Thorax. 58 (6): 494–9. doi:10.1136/thorax.58.6.494. PMC 1746693. PMID 12775859.
- Miedinger D, Chhajed PN, Tamm M, Stolz D, Surber C, Leuppi JD (June 2007). "Diagnostic tests for asthma in firefighters". Chest. 131 (6): 1760–7. doi:10.1378/chest.06-2218. PMID 17400683. Archived from the original on 2013-04-14.
- Turner S (February 2008). "Exhaled nitric oxide in the diagnosis and management of asthma". Current Opinion in Allergy and Clinical Immunology. 8 (1): 70–6. doi:10.1097/ACI.0b013e3282f3b4b0. PMID 18188021.
- Fujimura M, Ohkura N, Abo M, Furusho S, Waseda Y, Ichikawa Y, Hara J (May 2008). "Exhaled nitric oxide levels in patients with atopic cough and cough variant asthma". Respirology. 13 (3): 359–64. doi:10.1111/j.1440-1843.2008.01273.x. hdl:2297/9771. PMID 18399857.
- Oh MJ, Lee JY, Lee BJ, Choi DC (November 2008). "Exhaled nitric oxide measurement is useful for the exclusion of nonasthmatic eosinophilic bronchitis in patients with chronic cough". Chest. 134 (5): 990–995. doi:10.1378/chest.07-2541. PMID 18583518. Archived from the original on 2013-04-15.
- Sato S, Saito J, Sato Y, Ishii T, Xintao W, Tanino Y, et al. (October 2008). "Clinical usefulness of fractional exhaled nitric oxide for diagnosing prolonged cough". Respiratory Medicine. 102 (10): 1452–9. doi:10.1016/j.rmed.2008.04.018. PMID 18614345.
- Hahn PY, Morgenthaler TY, Lim KG (November 2007). "Use of exhaled nitric oxide in predicting response to inhaled corticosteroids for chronic cough". Mayo Clinic Proceedings. 82 (11): 1350–5. doi:10.4065/82.11.1350. PMID 17976354. Archived from the original on 2007-07-01.
- De Prins S, Marcucci F, Sensi L, Van de Mieroop E, Nelen V, Nawrot TS, et al. (September 2014). "Exhaled nitric oxide and nasal tryptase are associated with wheeze, rhinitis and nasal allergy in primary school children". Biomarkers. 19 (6): 481–7. doi:10.3109/1354750x.2014.937362. PMID 25019424.
- Jacobs L, Nawrot TS, de Geus B, Meeusen R, Degraeuwe B, Bernard A, et al. (October 2010). "Subclinical responses in healthy cyclists briefly exposed to traffic-related air pollution: an intervention study". Environmental Health. 9 (64): 64. doi:10.1186/1476-069X-9-64. PMC 2984475. PMID 20973949.
- Van Amsterdam JG, Verlaan BP, Van Loveren H, Elzakker BG, Vos SG, Opperhuizen A, Steerenberg PA (1999). "Air pollution is associated with increased level of exhaled nitric oxide in nonsmoking healthy subjects". Archives of Environmental Health. 54 (5): 331–5. doi:10.1080/00039899909602496. PMID 10501149.
- Adar SD, Adamkiewicz G, Gold DR, Schwartz J, Coull BA, Suh H (April 2007). "Ambient and microenvironmental particles and exhaled nitric oxide before and after a group bus trip". Environmental Health Perspectives. 115 (4): 507–12. doi:10.1289/ehp.9386. PMC 1852653. PMID 17450216.
- Bos I, De Boever P, Vanparijs J, Pattyn N, Panis LI, Meeusen R (March 2013). "Subclinical effects of aerobic training in urban environment". Medicine and Science in Sports and Exercise. 45 (3): 439–47. doi:10.1249/MSS.0b013e31827767fc. hdl:1942/14628. PMID 23073213. S2CID 5067347.
- American Thoracic Society; European Respiratory Society (April 2005). "ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005". American Journal of Respiratory and Critical Care Medicine. 171 (8): 912–30. doi:10.1164/rccm.200406-710ST. PMID 15817806. S2CID 1883790.
- Buchvald F, Baraldi E, Carraro S, Gaston B, De Jongste J, Pijnenburg MW, et al. (June 2005). "Measurements of exhaled nitric oxide in healthy subjects age 4 to 17 years". The Journal of Allergy and Clinical Immunology. 115 (6): 1130–6. doi:10.1016/j.jaci.2005.03.020. PMID 15940124.
- Napier E, Turner SW (August 2005). "Methodological issues related to exhaled nitric oxide measurement in children aged four to six years". Pediatric Pulmonology. 40 (2): 97–104. doi:10.1002/ppul.20249. PMID 15965893.
- Travers J, Marsh S, Aldington S, Williams M, Shirtcliffe P, Pritchard A, et al. (August 2007). "Reference ranges for exhaled nitric oxide derived from a random community survey of adults". American Journal of Respiratory and Critical Care Medicine. 176 (3): 238–42. doi:10.1164/rccm.200609-1346OC. PMID 17478616. S2CID 23531755.
- Turner S (May 2007). "The role of exhaled nitric oxide in the diagnosis, management and treatment of asthma". Mini Reviews in Medicinal Chemistry. 7 (5): 539–42. doi:10.2174/138955707780619635. PMID 17504190.
- Gustafsson LE, Leone AM, Persson MG, Wiklund NP, Moncada S (December 1991). "Endogenous nitric oxide is present in the exhaled air of rabbits, guinea pigs and humans". Biochemical and Biophysical Research Communications. 181 (2): 852–7. doi:10.1016/0006-291X(91)91268-H. PMID 1721811.
- Koshland DE (December 1992). "The molecule of the year". Science. 258 (5090): 1861. doi:10.1126/science.1470903. PMID 1470903.
- Alving K, Weitzberg E, Lundberg JM (October 1993). "Increased amount of nitric oxide in exhaled air of asthmatics". The European Respiratory Journal. 6 (9): 1368–70. PMID 7507065.
Further reading
- Taylor DR, Pijnenburg MW, Smith AD, De Jongste JC (September 2006). "Exhaled nitric oxide measurements: clinical application and interpretation". Thorax. 61 (9): 817–27. doi:10.1136/thx.2005.056093. PMC 2117092. PMID 16936238.