Phacoemulsification
Phacoemulsification is a modern cataract surgery method in which the eye's internal lens is emulsified with an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are replaced with irrigation of balanced salt solution to maintain the anterior chamber.
| Phacoemulsification | |
|---|---|
 Phacoemulsification: Cataract surgery, by a temporal approach, using a phacoemulsification probe (in right hand) and "chopper"(in left hand), being done under operating microscope at a United States Navy medical center | |
| ICD-9-CM | 13.41 |
| MeSH | D018918 |
Etymology
The term originated from phaco- (Greek phako-, comb. form of phakós, lentil; see lens) + emulsification.[1]
Preparation and precautions
Proper anesthesia is essential for ocular surgery. Topical anesthesia is most commonly employed, typically by the instillation of a local anesthetic such as tetracaine or lidocaine. Alternatively, lidocaine and/or longer-acting bupivacaine anesthestic may be injected into the area surrounding (peribulbar block) or behind (retrobulbar block) the eye muscle cone to more fully immobilize the extraocular muscles and minimize pain sensation. A facial nerve block using lidocaine and bupivacaine may occasionally be performed to reduce lid squeezing. General anesthesia is recommended for children, traumatic eye injuries with cataract, for very apprehensive or uncooperative patients and animals. Cardiovascular monitoring is preferable in local anesthesia and is mandatory in the setting of general anesthesia. Proper sterile precautions are taken to prepare the area for surgery, including use of antiseptics like povidone-iodine. Sterile drapes, gowns and gloves are employed. A plastic sheet with a receptacle helps collect the fluids during phacoemulsification. An eye speculum is inserted to keep the eyelids open.
Surgical technique
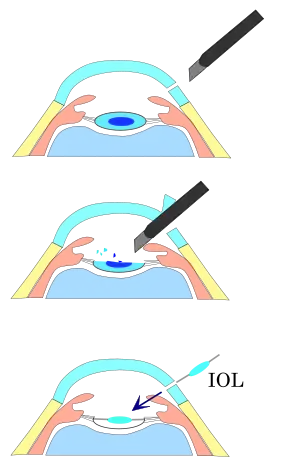
Before the phacoemulsification can be performed, one or more incisions are made in the eye to allow the introduction of surgical instruments. The surgeon then removes the anterior face of the capsule that contains the lens inside the eye. Phacoemulsification surgery involves the use of a machine with microprocessor-controlled fluid dynamics. These can be based on peristaltic or a venturi type of pump.
The phaco probe is an ultrasonic handpiece with a titanium or steel needle. The tip of the needle vibrates at ultrasonic frequency to sculpt and emulsify the cataract while the pump aspirates particles through the tip. In some techniques, a second fine steel instrument called a "chopper" is used from a side port to help with chopping the nucleus into smaller pieces. The cataract is usually broken into two or four pieces and each piece is emulsified and aspirated out with suction. The nucleus emulsification makes it easier to aspirate the particles. After removing all hard central lens nucleus with phacoemulsification, the softer outer lens cortex is removed with suction only.
An irrigation-aspiration probe or a bimanual system is used to aspirate out the remaining peripheral cortical matter, while leaving the posterior capsule intact. As with other cataract extraction procedures, an intraocular lens implant (IOL), is placed into the remaining lens capsule. For implanting a poly(methyl methacrylate) (PMMA) IOL, the incision has to be enlarged. For implanting a foldable IOL, the incision does not have to be enlarged. The foldable IOL, made of silicone or acrylic of appropriate power is folded either using a holder/folder, or a proprietary insertion device provided along with the IOL.
It is then inserted and placed in the posterior chamber in the capsular bag (in-the-bag implantation). Sometimes, a ciliary sulcus implantation may be required because of posterior capsular tears or because of zonular dialysis.[2] Because a smaller incision is required, few or no stitches are needed and the patient's recovery time is usually shorter when using a foldable IOL.[3][4]
History
Charles Kelman and Anton Banko introduced phacoemulsification in 1967.[5] Kelman had the idea to use ultrasonic vibrations after being inspired by his dentist's ultrasonic probe and collaborated with Banko who designed the first phacoemulsifier.
Research
Use of ultrasound in phacoemulsification can cause effects such as corneal edema, and macular edema after surgery. However, in some cases, use of ultrasound energy does not generate macular edema. The cause of macular edema in phacoemulsification is intraocular pressure fluctuation during surgery. Intraocular fluctuation can create micro bubbles and generate micro emboli in macular vessels that can cause micro ischemia in the retinal nerve fiber layer (RNFL).[6]
A Cochrane Review seeking to determine whether glaucoma surgery combined with cataract surgery via phacoemulsification has any advantages over cataract surgery (via phacoemulsification) alone, found that eyes that underwent combined (glaucoma and phacoemulsification) surgery had a significantly lower intraocular pressure (-1.62 mmHg) compared to eyes that underwent phacoemulsification cataract surgery alone.[7] The authors note that this finding is not conclusive, as the studies examined had many differences and poor reporting outcomes.[7]
A Cochrane Review of 16 trials seeking to compare the effectiveness of laser-assisted cataract surgery with standard ultrasound phacoemulsification found uncertain evidence suggesting benefits of one procedure over the other.[8] A meta-analysis of more than 14500 eyes and 37 studies found no significant differences between the two techniques in terms of visual or refractive outcomes or overall complications.[9]
In a Cochrane Review, clinical trials comparing NSAIDs versus corticosteroids in the treatment of postoperative eye inflammation were uncertain, but there was some evidence suggesting patients treated with NSAIDs were less likely to develop cystoid macular edema.[10]
Recent Advances
Recent advances in phacoemulsification technology involve combining the ultrasonic and I/A irrigation sleeve into a single disposable handpiece. This design reduces manufacturing costs, eliminates the risk of infection and provides better surgical outcomes[11][12]
References
- phacoemulsification Dictionary.com, LLC.
- Phacoemulsification
- Surgery Encyclopedia - Phacoemulsification for cataracts
- Surgery Encyclopedia - Extracapsular cataract extraction
- https://patents.google.com/patent/US3589363A
- Pardianto G (2015). "Recent awareness and consideration of intraocular pressure fluctuation during eye surgery". Journal of Cataract and Refractive Surgery. 41 (3): 695. doi:10.1016/j.jcrs.2015.01.009. PMID 25804599.
- Zhang ML, Hirunyachote P, Jampel H (2015). "Combined surgery versus cataract surgery alone for eyes with cataract and glaucoma". Cochrane Database Syst Rev. 7 (7): CD008671. doi:10.1002/14651858.CD008671.pub3. PMC 4730948. PMID 26171900.
- Day AC, Gore DM, Bunce C, Evans JR (2016). "Laser-assisted cataract surgery versus standard ultrasound phacoemulsification cataract surgery". Cochrane Database Syst Rev. 7: CD010735. doi:10.1002/14651858.CD010735.pub2. PMC 6458014. PMID 27387849.
- Popovic M, Campos-Möller X, Schlenker MB, Ahmed II (2016). "Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery: A Meta-Analysis of 14 567 Eyes". Ophthalmology. 123 (10): 2113–26. doi:10.1016/j.ophtha.2016.07.005. PMID 27538796.
- Juthani VV, Clearfield E, Chuck RS (2017). "Non-steroidal anti-inflammatory drugs versus corticosteroids for controlling inflammation after uncomplicated cataract surgery". Cochrane Database Syst Rev. 7: CD010516. doi:10.1002/14651858.CD010516.pub2. PMC 5580934. PMID 28670710.
- http://www.surgicaldesign.com/thefutureofphaco.php
- http://phaco.com