Spermatocele
Spermatocele is a fluid-filled cyst that develops at the head of the epididymis. The fluid is usually a clear or milky white color that may contain sperm.[3] It can vary in size from several millimeters to many centimeters. Small spermatoceles are relatively common, occurring in an estimated 30 percent of all men.[4] They are generally not painful. However, some people may experience discomfort such as a dull pain in the scrotum from larger spermatoceles.[5] They are not cancerous, nor do they cause an increased risk of testicular cancer. Additionally, unlike varicoceles, they do not reduce fertility.[5]
| Spermatocele | |
|---|---|
 | |
| Ultrasound of a testicle (grey) and a spermatocele (black). | |
| Pronunciation | |
| Specialty | Urology |
Causes
Spermatoceles can originate as diverticulum from the tubules found in the head of the epididymis. Sperm accumulation gradually causes the diverticulum to increase in size, causing a spermatocele. In many instances they appear to occur spontaneously without any preceding instances of injury.[4]
Scarring of any part of the epididymis can cause it to become obstructed and in turn form a spermatocele.[3]
Diagnosis
Spermatoceles can be discovered as incidental scrotal masses found on physical examination by a physician or by self-inspection of the scrotum and testicles.[5]

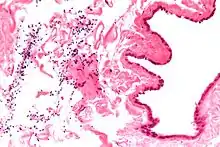
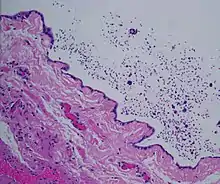
Finding a painless, cystic mass at the head of the epididymis that is clearly separate from the testicle can indicate a spermatocele. Shining a light through the mass through a process known as transillumination can also help differentiate between a fluid-filled cyst and a tumor, which would not allow as much light to pass.[6] If uncertainty exists, ultrasonography of the scrotum can confirm the presence of a spermatocele.[5]
Treatment
Small cysts as well as asymptomatic larger cysts are better left alone and carefully observed. However, treatment can be considered if the cysts are causing discomfort/pain, enlarging in size, or per patient request. There are a few different treatment options, ranging in levels of invasiveness.[5]
Certain drugs can be taken by mouth to decrease spermatocele-related symptoms such as pain and/or swelling. Aspiration and sclerotherapy are treatments that remove fluid from the spermatocele and seal the spermatocele sac closed from further fluid build-up, respectively.[5] Due to a higher risk of epididymis damage, fertility problems, and further recurrences, these procedures are not recommended and not commonly used.
The last option is to surgically remove the spermatocele entirely with a spermatocelectomy.[5] This standard procedure can be performed in an outpatient setting with the use of local or general anesthesia. Depending on the spermatocele, parts of the epididymis may also be removed. After surgical removal, it is possible that the pain will persist. There is also still a risk for recurrence and fertility problems.[6]
References
- Entry "spermatocele" in Merriam-Webster Online Dictionary.
- OED 2nd edition, 1989.
- "Spermatocele - Symptoms and causes". Mayo Clinic. Retrieved 2020-07-28.
- "Spermatocele: Symptoms, Causes, Treatments". Cleveland Clinic. Retrieved 2020-07-28.
- "Spermatoceles: Symptoms, Diagnosis & Treatment - Urology Care Foundation". www.urologyhealth.org. Retrieved 2020-07-28.
- "Spermatocele - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Retrieved 2020-07-28.
External links
| Classification |
|---|