Suicidal ideation
Suicidal ideation (or suicidal thoughts) is thinking about, considering, or planning suicide.[1] It is not a diagnosis, but is a symptom of some mental disorders and can also occur in response to adverse events without the presence of a mental disorder.[2]
| Suicidal ideation | |
|---|---|
| Other names | Suicidal thoughts, Suicidal ideas |
 | |
| Sappho (1897) by Ernst Stückelberg | |
| Specialty | Psychiatry, psychology |
On suicide risk scales, the range of suicidal ideation varies from fleeting thoughts to detailed planning. Passive suicidal ideation is thinking about not wanting to live or imagining being dead.[3][4] Active suicidal ideation is thinking about different ways to die or forming a plan to die.[3][4]
Most people who have suicidal thoughts do not go on to make suicide attempts, but suicidal thoughts are considered a risk factor.[5] During 2008–09, an estimated 8.3 million adults aged 18 and over in the United States, or 3.7% of the adult U.S. population, reported having suicidal thoughts in the previous year. An estimated 2.2 million in the U.S. reported having made suicide plans in 2014.[6] Suicidal thoughts are also common among teenagers.[7]
Suicidal ideation is generally associated with depression and other mood disorders; however, it seems to have associations with many other mental disorders, life events, and family events, all of which may increase the risk of suicidal ideation. Mental health researchers indicate that healthcare systems should provide treatment for individuals with suicidal ideation, regardless of diagnosis, because of the risk for suicidal acts and repeated problems associated with suicidal thoughts.[8][9] There are a number of treatment options for people who experience suicidal ideation.
Terminology
Another term for suicidal ideation is suicidal thoughts.[5]
When someone who has not shown a history of suicidal ideation experiences a sudden and pronounced thought of performing an act which would necessarily lead to their own death, psychologists call this an intrusive thought. A commonly experienced example of this is the high place phenomenon,[10] also referred to as the call of the void.[11] The urge to jump is called "mountain fever" in Brian Biggs' book Dear Julia.[12]
Euphemisms related to mortal contemplation include internal struggle,[13] voluntary death,[14] and eating one's gun.[15]
Signs and symptoms
The US Centers for Disease Control and Prevention (CDC) defines suicidal ideation "as thinking about, considering, or planning suicide."[1] The DSM-5 defines it as "thoughts about self-harm, with deliberate consideration or planning of possible techniques of causing one's own death." The ICD-11 describes suicidal ideation as "thoughts, ideas, or ruminations about the possibility of ending one's life, ranging from thinking that one would be better off dead to formulation of elaborate plans."[16] Suicidal ideation is a symptom for many mental disorders and can occur in response to adverse life events without the presence of a mental disorder.[2]
Risk factors
The risk factors for suicidal ideation can be divided into three categories: psychiatric disorders, life events, and family history.
Psychiatric disorders
There are several psychiatric disorders that appear to be comorbid with suicidal ideation or considerably increase the risk of suicidal ideation.[17] For example, many individuals with borderline personality disorder exhibit recurrent suicidal behavior and suicidal thoughts. One study found that 73% of patients with borderline personality disorder have attempted suicide, with the average patient having 3.4 attempts.[18] The following list includes the disorders that have been shown to be the strongest predictors of suicidal ideation. These are not the only disorders that can increase risk of suicidal ideation. The disorders in which risk is increased the greatest include:[19]
- Anxiety disorders
- Autism spectrum disorder
- Major depressive disorder[20]:162
- Dysthymia
- Bipolar disorder
- Attention deficit hyperactivity disorder (ADHD)
- Post-traumatic stress disorder (PTSD) and complex post-traumatic stress disorder (C-PTSD)[20]:278
- Personality disorders
- Psychosis (detachment from reality)
- Paranoia
- Schizophrenia[20]:104
- Substance use disorders,[21][22] inhalant use disorder[20]:538
- Body dysmorphic disorder[20]:245
- Nightmare disorder[20]:405
- Gender dysphoria[20]:454
- Conduct disorder[20]:473
- Specific learning disorder[20]:70
Medication side effects
Some medications, such as selective serotonin re-uptake inhibitors (SSRIs), can have suicidal ideation as a side effect. Moreover, these drugs' intended effects, can themselves have unintended consequence of an increased individual risk and collective rate of suicidal behavior: Among the set of persons taking the medication, a subset feel bad enough to want to attempt suicide (or to desire the perceived results of suicide) but are inhibited by depression-induced symptoms, such as lack of energy and motivation, from following through with an attempt. Among this subset, a "sub-subset" may find that the medication alleviates their physiological symptoms (such as lack of energy) and secondary psychological symptoms (e.g., lack of motivation) before or at lower doses than it alleviates their primary psychological symptom of depressed mood. Among this group of persons, the desire for suicide or its effects persists even as major obstacles to suicidal action are removed, with the effect that the incidences of suicide attempt and of completed suicide increase.[23]
Life events
Life events are strong predictors of increased risk for suicidal ideation. Furthermore, life events can also lead to or be comorbid with the previous listed psychiatric disorders and predict suicidal ideation through those means. Life events that adults and children face can be dissimilar and for this reason, the list of events that increase risk can vary in adults and children. The life events that have been shown to increase risk most significantly are[24]
- Alcohol abuse
- Studies have shown that individuals who binge drink, rather than drink socially, tend to have higher rates of suicidal ideation[25]
- Certain studies associate those who experience suicidal ideation with higher alcohol consumption[26]
- Not only do some studies show that solitary binge drinking can increase suicidal ideation, but there is a positive feedback relationship causing those who have more suicidal ideation to have more drinks per day in a solitary environment[25]
- Minoritized gender expression and/or sexuality[27]
- Unemployment[26]
- Chronic illness or pain
- Death of family members or friends
- End of a relationship or being rejected by a romantic interest
- Major change in life standard (e.g. relocation abroad)
- Other studies have found that tobacco use is correlated with depression and suicidal ideation[28]
- Unplanned pregnancy
- Bullying, including cyberbullying[29][30] and workplace bullying[31]
- Previous suicide attempts
- Having previously attempted suicide is one of the strongest indicators of future suicidal ideation or suicide attempts[25]
- Military experience
- Military personnel who show symptoms of PTSD, major depressive disorder, alcohol use disorder, and generalized anxiety disorder show higher levels of suicidal ideation[32]
- Community violence[33]
- Undesired changes in body weight[34]
- Women: increased BMI increases chance of suicidal ideation
- Men: severe decrease in BMI increases chance of suicidal ideation
- In general, the obese population has increased odds of suicidal ideation in relation to individuals that are of average-weight
- Exposure and attention to suicide related images or words[35]
Family history
- Parents with a history of depression
- Valenstein et al. studied 340 adult offspring whose parents had depression in the past. They found that 7% of the offspring had suicidal ideation in the previous month alone
- Abuse[33]
- Childhood: physical, emotional and sexual abuse[36]
- Adolescence: physical, emotional and sexual abuse
- Family violence
- Childhood residential instability
- Certain studies associate those who experience suicidal ideation with family disruption.[26]
Relationships with parents and friends
According to a study conducted by Ruth X. Liu of San Diego State University, a significant connection was found between the parent–child relationships of adolescents in early, middle and late adolescence and their likelihood of suicidal ideation. The study consisted of measuring relationships between mothers and daughters, fathers and sons, mothers and sons, and fathers and daughters. The relationships between fathers and sons during early and middle adolescence show an inverse relationship to suicidal ideation. Closeness with the father in late adolescence is "significantly related to suicidal ideation".[37] Liu goes on to explain the relationship found between closeness with the opposite sex parent and the child's risk of suicidal thoughts. It was found that boys are better protected from suicidal ideation if they are close to their mothers through early and late adolescence; whereas girls are better protected by having a close relationship with their father during middle adolescence.
An article published in 2010 by Zappulla and Pace found that suicidal ideation in adolescent boys is exacerbated by detachment from the parents when depression is already present in the child. Lifetime prevalence estimates of suicidal ideation among nonclinical populations of adolescents generally range from 60% and in many cases its severity increases the risk of completed suicide.[38]
Prevention
Early detection and treatment are the best ways to prevent suicidal ideation and suicide attempts. If signs, symptoms, or risk factors are detected early then the individual might seek treatment and help before attempting to take their own life. In a study of individuals who did commit suicide, 91% of them likely suffered from one or more mental illnesses. However, only 35% of those individuals were treated or being treated for a mental illness.[39] This emphasizes the importance of early detection; if a mental illness is detected, it can be treated and controlled to help prevent suicide attempts. Another study investigated strictly suicidal ideation in adolescents. This study found that depression symptoms in adolescents early as 9th grade is a predictor of suicidal ideation. Most people with long-term suicidal ideation do not seek professional help.
The previously mentioned studies point out the difficulty that mental health professionals have in motivating individuals to seek and continue treatment. Ways to increase the number of individuals who seek treatment may include:
- Increasing the availability of therapy treatment in early stage
- Increasing the public's knowledge on when psychiatric help may be beneficial to them
- Those who have adverse life conditions seem to have just as much risk of suicide as those with mental illness[39]
A study conducted by researchers in Australia set out to determine a course of early detection for suicidal ideation in teens stating that "risks associated with suicidality require an immediate focus on diminishing self-harming cognitions so as to ensure safety before attending to the underlying etiology of the behavior". A Psychological Distress scale known as the K10 was administered monthly to a random sample of individuals. According to the results among the 9.9% of individuals who reported "psychological distress (all categories)" 5.1% of the same participants reported suicidal ideation. Participants who scored "very high" on the Psychological Distress scale "were 77 times more likely to report suicidal ideation than those in the low category".[40]
In a one-year study conducted in Finland, 41% of the patients who later committed suicide saw a health care professional, most seeing a psychiatrist. Of those, only 22% discussed suicidal intent on their last office visit. In most of the cases, the office visit took place within a week of the suicide, and most of the victims had a diagnosed depressive disorder.[41]
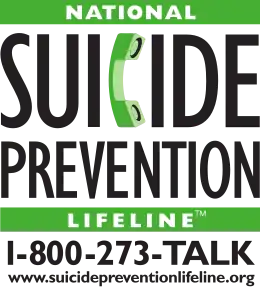
There are many centers where one can receive aid in the fight against suicidal ideation and suicide. Hemelrijk et al. (2012) found evidence that assisting people with suicidal ideation via the internet versus more direct forms such as phone conversations has a greater effect.
Assessment
Assessment seeks to understand an individual by integrating information from multiple sources such as clinical interviews; medical exams and physiological measures; standardized psychometric tests and questionnaires; structured diagnostic interviews; review of records; and collateral interviews.[42]
Interviews
Psychologists, psychiatrists, and other mental health professionals conduct clinical interviews to ascertain the nature of a patient or client's difficulties, including any signs or symptoms of illness the person might exhibit. Clinical interviews are "unstructured" in the sense that each clinician develops a particular approach to asking questions, without necessarily following a predefined format. Structured (or semi-structured) interviews prescribe the questions, their order of presentation, "probes" (queries) if a patient's response is not clear or specific enough, and a method to rate the frequency and intensity of symptoms.[43]
Standardized psychometric measures
- Beck Scale for Suicide Ideation
- Nurses' Global Assessment of Suicide Risk
- Suicidal Affect–Behavior–Cognition Scale (SABCS)[44]
- Columbia Suicide Severity Rating Scale
Treatment
Treatment of suicidal ideation can be problematic due to the fact that several medications have actually been linked to increasing or causing suicidal ideation in patients. Therefore, several alternative means of treating suicidal ideation are often used. The main treatments include: therapy, hospitalization, outpatient treatment, and medication or other modalities.[5]
Therapy
In psychotherapy a person explores the issues that make them feel suicidal and learns skills to help manage emotions more effectively.[5][45]
Hospitalization
Hospitalization allows the patient to be in a secure, supervised environment to prevent the suicidal ideation from turning into suicide attempts. In most cases, individuals have the freedom to choose which treatment they see fit for themselves. However, there are several circumstances in which individuals can be hospitalized involuntarily. These circumstances are:
- If an individual poses danger to self or others
- If an individual is unable to care for oneself
Hospitalization may also be a treatment option if an individual:
Outpatient treatment
Outpatient treatment allows individuals to remain at their place of residence and receive treatment when needed or on a scheduled basis. Being at home may improve quality of life for some patients, because they will have access to their personal belongings, and be able to come and go freely. Before allowing patients the freedom that comes with outpatient treatment, physicians evaluate several factors of the patient. These factors include the patient's level of social support, impulse control and quality of judgment. After the patient passes the evaluation, they are often asked to consent to a "no-harm contract". This is a contract formulated by the physician and the family of the patient. Within the contract, the patient agrees not to harm themself, to continue their visits with the physician, and to contact the physician in times of need.[5] There is some debate as to whether "no-harm" contracts are effective. These patients are then checked on routinely to assure they are maintaining their contract and avoiding dangerous activities (drinking alcohol, driving fast, and not wearing a seat belt, etc.).
Medication
Prescribing medication to treat suicidal ideation can be difficult. One reason for this is that many medications lift patients' energy levels before lifting their mood. This puts them at greater risk of following through with attempting suicide. Additionally, if a person has a comorbid psychiatric disorder, it may be difficult to find a medication that addresses both the psychiatric disorder and suicidal ideation.
Antidepressants may be effective.[5] Often, SSRIs are used instead of TCAs as the latter typically have greater harm in overdose.[5]
Antidepressants have been shown to be a very effective means of treating suicidal ideation. One correlational study compared mortality rates due to suicide to the use of SSRI antidepressants within certain counties. The counties which had higher SSRI use had a significantly lower number of deaths caused by suicide.[46] Additionally, an experimental study followed depressed patients for one year. During the first six months of that year, the patients were examined for suicidal behavior including suicidal ideation. The patients were then prescribed antidepressants for the six months following the first six observatory months. During the six months of treatment, experimenters found suicide ideation reduced from 47% of patients down to 14% of patients.[47] Thus, it appears from current research that antidepressants have a helpful effect on the reduction of suicidal ideation.
Although research is largely in favor of the use of antidepressants for the treatment of suicidal ideation, in some cases antidepressants are claimed to be the cause of suicidal ideation. Upon the start of using antidepressants, many clinicians will note that sometimes the sudden onset of suicidal ideation may accompany treatment. This has caused the Food and Drug Administration (FDA) to issue a warning stating that sometimes the use of antidepressants may actually increase the thoughts of suicidal ideation.[46] Medical studies have found antidepressants help treat cases of suicidal ideation and work especially well with psychological therapy.[48] Lithium reduces the risk of suicide in people with mood disorders.[49] Tentative evidence finds clozapine in people with schizophrenia reduces the risk of suicide.[50]
References
- Klonsky, E. David; May, Alexis M.; Saffer, Boaz Y. (2016-03-28). "Suicide, Suicide Attempts, and Suicidal Ideation". Annual Review of Clinical Psychology. 12 (1): 307–330. doi:10.1146/annurev-clinpsy-021815-093204. ISSN 1548-5943. PMID 26772209.
- Barry, Lisa C. Passive Suicidal Ideation in Older Adults: Implications for Suicide Prevention, American Journal of Geriatric Psychiatry 27, no. 12 (December 2019): 1411 ("... growing evidence points toward a subgroup of individuals who endorse passive SI [suicidal ideation] in later life outside the context of clinical depression.")
- Falcone, Tatiana; Timmons-Mitchell, Jane (2018-05-18). "Mood Disorders and Suicide". Suicide Prevention: A Practical Guide for the Practitioner. Springer. p. 38. ISBN 978-3-319-74391-2.
- Kumar, Updesh (2017-10-26). "Suicidal Ideation in Adolescents–A Transcultural Analysis". Handbook of Suicidal Behaviour. Springer. p. 269. ISBN 978-981-10-4816-6.
- Gliatto, MF; Rai, AK (March 1999). "Evaluation and Treatment of Patients with Suicidal Ideation". American Family Physician. 59 (6): 1500–6. PMID 10193592. Archived from the original on 2006-09-25. Retrieved 2007-01-08.

- Crosby, Alex; Beth, Han (October 2011). "Suicidal Thoughts and Behaviors Among Adults Aged ≥18 Years --- United States, 2008-2009". Morbidity and Mortality Weekly Report (MMWR). 60 (13). Archived from the original on 2015-01-07. Retrieved 2015-01-08.
- Uddin, R; Burton, NW; Maple, M; Khan, SR; Khan, A (2019). "Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study" (PDF). The Lancet Child & Adolescent Health. 3 (4): 223–233. doi:10.1016/S2352-4642(18)30403-6. hdl:10072/387579. PMID 30878117. Archived (PDF) from the original on 2020-02-18. Retrieved 2019-11-29.
- Griffin, E.; Kavalidou, K.; Bonner, B.; O'Hagan, D.; Corcoran, P. (2020). "Risk of repetition and subsequent self-harm following presentation to hospital with suicidal ideation: A longitudinal registry study" (PDF). EClinicalMedicine. 23: 100378. doi:10.1016/j.eclinm.2020.100378. ISSN 2589-5370. PMC 7280762. PMID 32529177.
- Kleiman, Evan M. (2020). "Suicidal thinking as a valuable clinical endpoint" (PDF). EClinicalMedicine. 23. doi:10.1016/j.eclinm.2020.100399. ISSN 2589-5370. PMID 32566922.
- Adam, David (2014). "How OCD creates prisoners of the mind". New Scientist. 222 (2966): 36–39. Bibcode:2014NewSc.222...36A. doi:10.1016/s0262-4079(14)60832-0.
- Demont, Marc, and Of Male Friendship. "Gender Studies: Masculinity Studies."
- Biggs, Brian (2000). Dear Julia. Marietta, Georgia: Top Shelf. pp. 40–42. ISBN 1-891830-12-0.
- Brown, Gregory K.; et al. (2005). "The internal struggle between the wish to die and the wish to live: a risk factor for suicide". American Journal of Psychiatry. 162 (10): 1977–1979. doi:10.1176/appi.ajp.162.10.1977. PMID 16199851.
- Miller, Franklin G.; Meier, Diane E. (1998). "Voluntary death: a comparison of terminal dehydration and physician-assisted suicide". Annals of Internal Medicine. 128 (7): 559–562. doi:10.7326/0003-4819-128-7-199804010-00007. PMID 9518401. S2CID 34734585.
- Baker, Thomas E (2009). "Dell P. Hackett and John M. Violanti, Police Suicide: Tactics for Prevention". Journal of Police and Criminal Psychology. 24 (1): 66–67. doi:10.1007/s11896-008-9037-4. S2CID 142153854.
- World Health Organization, ICD-11 for Mortality and Morbidity Statistics, ver. 09/2020, MB26.A Suicidal ideation
- Hemelrijk, E; Van Ballegooijen, W; Donker, T; Van Straten, A; Kerkhof, A (2012). "Internet-based screening for suicidal ideation in common mental disorders". Crisis: The Journal of Crisis Intervention and Suicide Prevention. 33 (4): 215–221. doi:10.1027/0227-5910/a000142. PMID 22713975. S2CID 21192564.
- Soloff, PH; Kevin, GL; Thomas, MK; Kevin, MM; Mann, JJ (1 April 2000). "Characteristics of Suicide Attempts of Patients With Major Depressive Episode and Borderline Personality Disorder: A Comparative Study". American Journal of Psychiatry. 157 (4): 601–608. doi:10.1176/appi.ajp.157.4.601. PMID 10739420. S2CID 27150913.
- Harris, EC; Barraclough, B (1997). "Suicide as an outcome for mental disorders. A meta analysis". The British Journal of Psychiatry. 170 (3): 205–228. doi:10.1192/bjp.170.3.205. PMID 9229027. S2CID 33824780.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington, VA: American Psychiatric Publishing. doi:10.1176/appi.books.9780890425596. hdl:2027.42/138395. ISBN 978-0-89042-559-6.
- Lemon, TI; Shah, RD (2013). "Needle exchanges – a forgotten outpost in suicide and self-harm prevention". Journal of Psychosomatic Research. 74 (6): 551–552. doi:10.1016/j.jpsychores.2013.03.057.
- Lemon, TI (2013). "Suicide ideation in drug users and the role of needles exchanges and their workers". Journal Psych Med. 6 (5): 429. doi:10.1016/j.ajp.2013.07.003. PMID 24011693.
- "The most commonly prescribed type of antidepressant". Mayo Clinic. Retrieved 2020-10-08.
- Fergusson, DM; Woodward, LJ; Horwood, LJ (2000). "Risk factors and life processes associated with the onset of suicidal behavior during adolescence and early adulthood". Psychological Medicine. 30 (1): 23–39. doi:10.1017/s003329179900135x. PMID 10722173.
- Gonzalez, VM (2012). "Association of solitary binge drinking and suicidal behavior among emerging adult college students". Psychology of Addictive Behaviors. 26 (3): 609–614. doi:10.1037/a0026916. PMC 3431456. PMID 22288976.

- Valenstein, H; Cronkite, RC; Moos, RH; Snipes, C; Timko, C (2012). "Suicidal ideation in adult offspring of depressed and matched control parents: Childhood and concurrent predictors". Journal of Mental Health. 21 (5): 459–468. doi:10.3109/09638237.2012.694504. PMID 22978501. S2CID 9842249.
- McDermott, Elizabeth; Hughes, Elizabeth; Rawlings, Victoria (February 2018). "Norms and normalisation: understanding lesbian, gay, bisexual, transgender and queer youth, suicidality and help-seeking". Culture, Health & Sexuality. 20 (2): 156–172. doi:10.1080/13691058.2017.1335435. ISSN 1369-1058. PMID 28641479.
- Dugas, E; Low, NP; Rodriguez, D; Burrows, S; Contreras, G; Chaiton, M; et al. (2012). "Early Predictors of Suicidal Ideation in Young Adults". Canadian Journal of Psychiatry. 57 (7): 429–436. doi:10.1177/070674371205700706. PMID 22762298.
- "Cyberbullying Research Summary – Cyberbullying and Suicide" (PDF). Cyberbullying Research Center. Archived (PDF) from the original on 4 September 2012. Retrieved 3 July 2012.
- "The relationship between bullying, depression and suicidal thoughts/behaviour in Irish adolescents". Department of Health and Children. Archived from the original on 1 September 2014. Retrieved 3 July 2012.
- Hogh, Annie; Gemzøe Mikkelsen, Eva; Hansen, Åse Marie (2010). "Chapter 4: Individual Consequences of Workplace Bullying/Mobbing". In Einarsen, Stale; Hoel, Helge; Zapf, Dieter; Cooper, Cary (eds.). Bullying and Harassment in the Workplace: Developments in Theory, Research, and Practice. Boca Raton, Florida: CRC Press. ISBN 9781439804896. OCLC 1087897728.
- Richardson, JD; St Cyr, KC; McIntyre-Smith, AM; Haslam, D; Elhai, JD; Sareen, J (2012). "Examining the association between psychiatric illness and suicidal ideation in a sample of treatment-seeking Canadian peacekeeping and combat veterans with posttraumatic stress disorder PTSD". Canadian Journal of Psychiatry. 57 (8): 496–504. doi:10.1177/070674371205700808. PMID 22854032.
- Thompson, R; Litrownik, AJ; Isbell, P; Everson, MD; English, DJ; Dubowitz, H; et al. (2012). "Adverse experiences and suicidal ideation in adolescence: Exploring the link using the LONGSCAN samples". Psychology of Violence. 2 (2): 211–225. doi:10.1037/a0027107. PMC 3857611. PMID 24349862.

- Carpenter, KM; Hasin, DS; Allison, DB; Faith, MS (2000). "Relationships between obesity and DSM-IV major depressive disorder, suicidal ideation, and suicide attempts: Results from a general population study". American Journal of Public Health. 90 (2): 251–257. doi:10.2105/ajph.90.2.251. PMC 1446144. PMID 10667187.
- Cha, CB; Najmi, S; Park, JM; Finn, CT; Nock, MK (2010). "Attentional bias toward suicide-related stimuli predicts suicidal behavior". Journal of Abnormal Psychology. 119 (3): 616–622. doi:10.1037/a0019710. PMC 2994414. PMID 20677851.

- Briere, John (1986). "Suicidal thoughts and behaviours in former sexual abuse victims". Canadian Journal of Behavioural Science. 18 (4): 413–423. doi:10.1037/h0079962.
- Liu, Ruth X. (December 2005). "Parent-Youth Closeness and Youth's Suicidal Ideation; The Moderating Effects of Gender, Stages of Adolescence, and Race or Ethnicity". Youth & Society. 37 (2): 160–162. doi:10.1177/0044118X04272290. S2CID 144519020.
- Zappulla, Carla. "Relations between suicidal ideation, depression, and emotional autonomy from parents in adolescence". Springer Science + Business Media LLC. Retrieved 10 April 2012.
- Cavanagh, JO; Owens, DC; Johnstone, EC (1999). "Life events in suicide and undetermined death in south-east Scotland: a case-control study using the method of psychological autopsy". Social Psychiatry and Psychiatric Epidemiology. 34 (12): 645–650. doi:10.1007/s001270050187. PMID 10703274. S2CID 31350280.
- Chamberlain, P; Goldney, R; Delfabbro, P; Gill, T; Dal Grande, L (2009). "Suicidal Ideation: The Clinical Utility of the K10". Crisis. 1. 30 (1): 39–42. doi:10.1027/0227-5910.30.1.39. PMID 19261567.
- Halgin, Richard P.; Susan Whitbourne (2006). Abnormal psychology: clinical perspectives on psychological disorders. Boston: McGraw-Hill. pp. 267–272. ISBN 978-0-07-322872-3.
- Coaley, Keith, "Introduction: Individual Differences and Psychometrics", chap. 1 in An Introduction to Psychological Assessment and Psychometrics, 2nd ed. (London: Sage, 2014), 1–34. ISBN 978-1-4462-6714-1
- Rogers, Richard. Handbook of Diagnostic and Structured Interviewing. New York: Guilford, 2001.
- Harris, K. M.; Syu, J. J.; Lello, O. D.; Chew, Y. L. E.; Willcox, C. H.; Ho, R. H. M. (2015). "The ABC's of suicide risk assessment: Applying a tripartite approach to individual evaluations". PLOS ONE. 10 (6): 6. Bibcode:2015PLoSO..1027442H. doi:10.1371/journal.pone.0127442. PMC 4452484. PMID 26030590.
- "Suicide and suicidal thoughts - Diagnosis and treatment - Mayo Clinic". Archived from the original on 2016-06-05. Retrieved 2016-06-03.
- Simon, GE (2006). "How can we know whether antidepressants increase suicide risk?". American Journal of Psychiatry. 163 (11): 1861–1863. doi:10.1176/APPI.AJP.163.11.1861. PMID 17074930.
- Mulder, RT; Joyce, P. R.; Frampton, C. M. A.; Luty, S. E. (2008). "Antidepressant treatment is associated with a reduction in suicidal ideation and suicide attempts". Acta Psychiatrica Scandinavica. 118 (12): 116–122. doi:10.1111/j.1600-0447.2008.01179.x. PMID 18384467. S2CID 34987889.
- Zisook, S; Lesser, IM; Lebowitz, B; Rush, AJ; Kallenberg, G; Wisniewski, SR; et al. (2011). "Effect of antidepressant medication treatment on suicidal ideation and behavior in a randomized trial: An exploratory report from the Combining Medications to Enhance Depression Outcomes Study". Journal of Clinical Psychiatry. 72 (10): 1322–1332. doi:10.4088/JCP.10m06724. PMID 22075098. S2CID 20222046.
- Cipriani A, Hawgon K, Stockton S, et al. (27 June 2013). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis". BMJ. 346 (jun27 4): f3646. doi:10.1136/bmj.f3646. PMID 23814104.
- Wagstaff, A; Perry, C (2003). "Clozapine: in prevention of suicide in patients with schizophrenia or schizoaffective disorder". CNS Drugs. 17 (4): 273–80, discussion 281–3. doi:10.2165/00023210-200317040-00004. PMID 12665398.
Further reading
- Beck, AT; Steer, RA; Kovacs, M; Garrison, B (1985). "Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation". Am J Psychiatry. 142 (5): 559–563. CiteSeerX 10.1.1.462.6328. doi:10.1176/ajp.142.5.559. PMID 3985195.
- Uncapher, H (2000–2001). "Cognitive biases and suicidal ideation in elderly psychiatric inpatients". Omega. 42 (1): 21–36. doi:10.2190/6uu8-hk8e-hl0v-q4cu. S2CID 144242247.
- Uncapher, H; Gallagher-Thompson, D; Osgood, NJ (1998). "Hopelessness and suicidal ideation in older adults". The Gerontologist. 38 (1): 62–70. doi:10.1093/geront/38.1.62. PMID 9499654.
External links
| Classification |
|---|

