Thymic stromal lymphopoietin
Thymic stromal lymphopoietin (TSLP) is a protein belonging to the cytokine family. It is known to play an important role in the maturation of T cell populations through activation of antigen presenting cells.
TSLP is produced mainly by non-hematopoietic cells such as fibroblasts, epithelial cells and different types of stromal or stromal-like cells. These cells are located in regions where TSLP activity is required.
Gene ontology
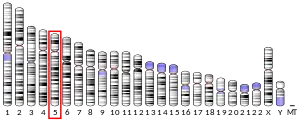
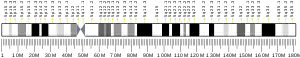
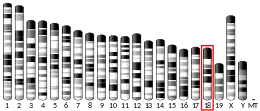
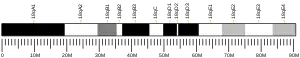
TSLP production has been observed in various species, including humans and mice. In humans TSLP is encoded by the TSLP gene.[5][6] Alternative splicing of this gene results in two transcript variants.[6]
Function
It mainly impacts myeloid cells and induces the release of T cell-attracting chemokines from monocytes and enhances the maturation of myeloid (CD11c+) dendritic cells.[7] TSLP has also been shown to activate the maturation of a specific subset of dendritic cells located within the epidermis, called Langerhans cells.[8] Within the thymus TSLP activation of both myeloid and plasmacytoid (CD123+) dendritic cells results in the production of regulatory T cells.[9][10]
Signaling
TSLP signals through a heterodimeric receptor complex composed of the thymic stromal lymphopoietin receptor CRLF2 and the IL-7R alpha chain. After binding STAT5 phosphorylation is induced, resulting in the expression of upstream transcription factors.[11]
Disease
TSLP expression is linked to many disease states including asthma,[12] inflammatory arthritis,[13] atopic dermatitis,[8] eczema, eosinophilic esophagitis and other allergic states.[14][15] The factors inducing the activation of TSLP release are not clearly defined.
Asthma
Expression of TSLP is enhanced under asthma-like conditions (aka Airway HyperResponsiveness or AHR model in the mouse), conditioning APCs in order to orient the differentiation of T cells coming into the lungs towards a TH2 profile (T helper 2 pathway). The TH2 cells then release factors promoting an inflammatory reaction following the repeated contact with a specific antigen in the airways .
Atopic dermatitis
TSLP-activated Langerhans cells of the epidermis induce the production of pro-inflammatory cytokines like TNF-alpha by T cells potentially causing atopic dermatitis.[8] It is thought that understanding the mechanism of TSLP production and those potential substances that block the production, one may be able to prevent or treat conditions of asthma and/or eczema.[16]
Inhibition
The TSLP signaling axis is an attractive therapeutic target. Amgen's Tezepelumab, a monoclonal antibody which blocks TSLP, is currently in phase III clinical trials for the treatment of asthma.[17] Fusion proteins consisting of TSLPR and IL-7Rα which can trap TSLP with excellent affinity have also been designed. [18] Additional approaches towards TSLP/TSLPR inhibition include peptides derived from the TSLP:TSLPR interface,[19] natural products [20] and computational fragment-based screening.[21]
References
- GRCh38: Ensembl release 89: ENSG00000145777 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000024379 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Quentmeier H, Drexler HG, Fleckenstein D, Zaborski M, Armstrong A, Sims JE, Lyman SD (August 2001). "Cloning of human thymic stromal lymphopoietin (TSLP) and signaling mechanisms leading to proliferation". Leukemia. 15 (8): 1286–92. doi:10.1038/sj.leu.2402175. PMID 11480573.
- "Entrez Gene: TSLP thymic stromal lymphopoietin".
- Reche PA, Soumelis V, Gorman DM, Clifford T, Travis M, Zurawski SM, et al. (July 2001). "Human thymic stromal lymphopoietin preferentially stimulates myeloid cells". Journal of Immunology. 167 (1): 336–43. doi:10.4049/jimmunol.167.1.336. PMID 11418668.
- Ebner S, Nguyen VA, Forstner M, Wang YH, Wolfram D, Liu YJ, Romani N (April 2007). "Thymic stromal lymphopoietin converts human epidermal Langerhans cells into antigen-presenting cells that induce proallergic T cells". The Journal of Allergy and Clinical Immunology. 119 (4): 982–90. doi:10.1016/j.jaci.2007.01.003. PMID 17320941.
- Watanabe N, Wang YH, Lee HK, Ito T, Wang YH, Cao W, Liu YJ (August 2005). "Hassall's corpuscles instruct dendritic cells to induce CD4+CD25+ regulatory T cells in human thymus". Nature. 436 (7054): 1181–5. doi:10.1038/nature03886. PMID 16121185. S2CID 4387582.
- Hanabuchi S, Ito T, Park WR, Watanabe N, Shaw JL, Roman E, et al. (March 2010). "Thymic stromal lymphopoietin-activated plasmacytoid dendritic cells induce the generation of FOXP3+ regulatory T cells in human thymus". Journal of Immunology. 184 (6): 2999–3007. doi:10.4049/jimmunol.0804106. PMC 3325785. PMID 20173030.
- Isaksen DE, Baumann H, Trobridge PA, Farr AG, Levin SD, Ziegler SF (December 1999). "Requirement for stat5 in thymic stromal lymphopoietin-mediated signal transduction". Journal of Immunology. 163 (11): 5971–7. PMID 10570284.
- Ying S, O'Connor B, Ratoff J, Meng Q, Mallett K, Cousins D, et al. (June 2005). "Thymic stromal lymphopoietin expression is increased in asthmatic airways and correlates with expression of Th2-attracting chemokines and disease severity". Journal of Immunology. 174 (12): 8183–90. doi:10.4049/jimmunol.174.12.8183. PMID 15944327.
- Koyama K, Ozawa T, Hatsushika K, Ando T, Takano S, Wako M, et al. (May 2007). "A possible role for TSLP in inflammatory arthritis". Biochemical and Biophysical Research Communications. 357 (1): 99–104. doi:10.1016/j.bbrc.2007.03.081. PMID 17416344.
- Soumelis V, Liu YJ (February 2004). "Human thymic stromal lymphopoietin: a novel epithelial cell-derived cytokine and a potential key player in the induction of allergic inflammation". Springer Seminars in Immunopathology. 25 (3–4): 325–33. doi:10.1007/s00281-003-0152-0. PMID 14999427. S2CID 9713181.
- Soumelis V, Reche PA, Kanzler H, Yuan W, Edward G, Homey B, et al. (July 2002). "Human epithelial cells trigger dendritic cell mediated allergic inflammation by producing TSLP" (PDF). Nature Immunology. 3 (7): 673–80. doi:10.1038/ni805. PMID 12055625. S2CID 9648786.
- Demehri S, Morimoto M, Holtzman MJ, Kopan R (May 2009). "Skin-derived TSLP triggers progression from epidermal-barrier defects to asthma". PLOS Biology. 7 (5): e1000067. doi:10.1371/journal.pbio.1000067. PMC 2700555. PMID 19557146. Lay summary – BBC News.
- "Studies found for: Tezepelumab". ClinicalTrials.Gov. National Library of Medicine, National Institutes of Health, U.S. Department of Health and Human Services.
- Verstraete K, Peelman F, Braun H, Lopez J, Van Rompaey D, Dansercoer A, et al. (April 2017). "Structure and antagonism of the receptor complex mediated by human TSLP in allergy and asthma". Nature Communications. 8: 14937. doi:10.1038/ncomms14937. PMC 5382266. PMID 28368013.
- Park S, Park Y, Son SH, Lee K, Jung YW, Lee KY, et al. (October 2017). "Synthesis and biological evaluation of peptide-derived TSLP inhibitors". Bioorganic & Medicinal Chemistry Letters. 27 (20): 4710–4713. doi:10.1016/j.bmcl.2017.09.010. PMID 28927768.
- Park BB, Choi JW, Park D, Choi D, Paek J, Kim HJ, et al. (June 2019). "Structure-Activity Relationships of Baicalein and its Analogs as Novel TSLP Inhibitors". Scientific Reports. 9 (1): 8762. doi:10.1038/s41598-019-44853-5. PMC 6584507. PMID 31217492.
- Van Rompaey D, Verstraete K, Peelman F, Savvides SN, Augustyns K, Van Der Veken P, De Winter H (December 2017). "Virtual screening for inhibitors of the human TSLP:TSLPR interaction". Scientific Reports. 7 (1): 17211. doi:10.1038/s41598-017-17620-7. PMC 5722893. PMID 29222519.
Further reading
- Ziegler SF, Liu YJ (July 2006). "Thymic stromal lymphopoietin in normal and pathogenic T cell development and function". Nature Immunology. 7 (7): 709–14. doi:10.1038/ni1360. PMID 16785889. S2CID 26635282.
- Liu YJ (August 2007). "Thymic stromal lymphopoietin and OX40 ligand pathway in the initiation of dendritic cell-mediated allergic inflammation". The Journal of Allergy and Clinical Immunology. 120 (2): 238–44, quiz 245-6. doi:10.1016/j.jaci.2007.06.004. PMID 17666213.
- Gilliet M, Soumelis V, Watanabe N, Hanabuchi S, Antonenko S, de Waal-Malefyt R, Liu YJ (April 2003). "Human dendritic cells activated by TSLP and CD40L induce proallergic cytotoxic T cells". The Journal of Experimental Medicine. 197 (8): 1059–63. doi:10.1084/jem.20030240. PMC 2193883. PMID 12707303.
- Watanabe N, Hanabuchi S, Marloie-Provost MA, Antonenko S, Liu YJ, Soumelis V (June 2005). "Human TSLP promotes CD40 ligand-induced IL-12 production by myeloid dendritic cells but maintains their Th2 priming potential". Blood. 105 (12): 4749–51. doi:10.1182/blood-2004-09-3622. PMID 15741223.
- Lee HC, Ziegler SF (January 2007). "Inducible expression of the proallergic cytokine thymic stromal lymphopoietin in airway epithelial cells is controlled by NFkappaB". Proceedings of the National Academy of Sciences of the United States of America. 104 (3): 914–9. doi:10.1073/pnas.0607305104. PMC 1783414. PMID 17213320.
- Zhang K, Shan L, Rahman MS, Unruh H, Halayko AJ, Gounni AS (August 2007). "Constitutive and inducible thymic stromal lymphopoietin expression in human airway smooth muscle cells: role in chronic obstructive pulmonary disease". American Journal of Physiology. Lung Cellular and Molecular Physiology. 293 (2): L375-82. doi:10.1152/ajplung.00045.2007. PMID 17513456.
- Rochman I, Watanabe N, Arima K, Liu YJ, Leonard WJ (June 2007). "Cutting edge: direct action of thymic stromal lymphopoietin on activated human CD4+ T cells". Journal of Immunology. 178 (11): 6720–4. doi:10.4049/jimmunol.178.11.6720. PMID 17513717.
- Wang YH, Angkasekwinai P, Lu N, Voo KS, Arima K, Hanabuchi S, et al. (August 2007). "IL-25 augments type 2 immune responses by enhancing the expansion and functions of TSLP-DC-activated Th2 memory cells". The Journal of Experimental Medicine. 204 (8): 1837–47. doi:10.1084/jem.20070406. PMC 2118667. PMID 17635955.