Vaginal cancer
Vaginal cancer is a malignant tumor that forms in the tissues of the vagina. Primary tumors are most usually squamous cell carcinomas. Primary tumors are rare, and more usually vaginal cancer occurs as a secondary tumor. Vaginal cancer occurs more often in women over age 50, but can occur at any age, even in infancy. It often can be cured if found and treated in early stages. Surgery alone or surgery combined with pelvic radiation is typically used to treat vaginal cancer. Children can be diagnosed with advanced vaginal cancer. They are treated by surgery, radiation therapy, and chemotherapy. Vaginal cancer in children may recur. Gene therapy to treat vaginal cancer is currently in clinical trials.[1]
| Vaginal cancer | |
|---|---|
| Specialty | Oncology |
Description
Carcinoma of the vagina occurs in less than 2% of women with pelvic malignant tumors. Squamous carcinoma is the most common type of vaginal cancer. The human papilloma virus (HPV) is strongly associated with vaginal cancer. Vaginal cancer occurs most often in the upper third of the vagina (51%), 30% are found in the lower third, and 19% in the middle third. Vaginal cancer can present as an elevated lesion growing out from the epithelial surface or an ulcer-like, shallow depression. Definitive diagnosis is determined by biopsy.[2]
Signs and symptoms
Most vaginal cancers do not cause signs or symptoms early on. When vaginal cancer does cause symptoms, they may include:
- Vaginal discharge or abnormal bleeding
- Unusually heavy flow of blood
- Bleeding after menopause
- Bleeding between periods; or any other
- Bleeding that is longer than normal
- Blood in the stool or urine
- Frequent or urgent need to urinate
- Feeling constipated[3]
- pain during sexual intercourse
- a lump or growth in the vagina that can be felt[4]
Enlarged pelvic lymph nodes can sometimes be palpated[5]
Risk factors
- Prenatal exposure to diethylstilbestrol
- Infection with human papillomavirus (HPV) type 16
- Infection with human immunodeficiency virus (HIV) type 1[6][7]
- Previous history of cervical cancer
- Smoking
- Chronic vulvar itching or burning[3]
Types
There are two primary types of vaginal cancer: squamous-cell carcinoma and adenocarcinoma.[8]
- Squamous-cell carcinoma of the vagina arises from the squamous cells (epithelium) that line the vagina. This is the most common type of vaginal cancer. It is found most often in women aged 60 or older.
- Vaginal adenocarcinoma arises from the glandular (secretory) cells in the lining of the vagina. Adenocarcinoma is more likely to spread to the lungs and lymph nodes.
- Clear cell adenocarcinoma occurs in a small percentage of women (termed "DES-Daughters") born between 1938 and 1973 (later outside the United States) that were exposed to the drug diethylstilbestrol (DES) in utero. DES was prescribed to 5 to 10 million mothers period to prevent possible miscarriages and premature births.[9] Typically, women develop DES-related adenocarcinoma before age 30, but increasing evidence suggests possible effects or cancers (including other forms of vaginal glandular tumors) at a later age. DES-exposure in women is also linked to various infertility and pregnancy complications. Daughters exposed to DES in utero may also have an increased risk of moderate/severe cervical squamous cell dysplasia and an increased risk of breast cancer.[9] Approximately one in 1,000 (0.1%) DES Daughters will be diagnosed with clear cell adenocarcinoma. The risk is virtually non-existent among premenopausal women not exposed to DES.[10]
- Vaginal germ cell tumors (primarily teratoma and endodermal sinus tumor) are rare. They are found most often in infants and children.
- Sarcoma botryoides, a rhabdomyosarcoma also is found most often in infants and children.
- Vaginal melanoma, a melanoma that appears in the vagina.
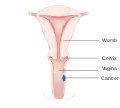 Stage 1 vaginal cancer
Stage 1 vaginal cancer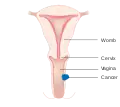 Stage 2 vaginal cancer
Stage 2 vaginal cancer Stage 3 vaginal cancer
Stage 3 vaginal cancer Stage 4A vaginal cancer
Stage 4A vaginal cancer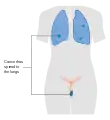 Stage 4B vaginal cancer
Stage 4B vaginal cancer
Diagnosis
Several tests are used to diagnose vaginal cancer, including:
- Physical exam and history
- Pelvic exam
- Pap smear
- Biopsy
- Colposcopy
Recommendations for women with vaginal cancer is not to have routine surveillance imaging to monitor the cancer unless they have new symptoms or rising tumor markers.[11] Imaging without these indications is discouraged because it is unlikely to detect a recurrence or improve survival, and because it has its own costs and side effects.[11] MRI provides visualization of the extent of vaginal cancer.[12]
Management
Historically, the combination of external-beam radiation therapy (EBRT) has been the most common treatment for vaginal cancer. In early stages of vaginal cancer, surgery also has some benefit. This management and treatment is less effective for those with advanced stages of cancer but works well in early stages with high rates of cure. Advanced vaginal cancer only has a 5-year survival rates of 52.2%, 42.5% and 20.5% for patients with stage II, III and IVa disease. Newer treatments for advanced stages of ovarian have been developed. These utilize concurrent carboplatin plus paclitaxel, EBRT and high-dose-rate interstitial brachytherapy (HDR-ISBT).[5]
When the chance of surgical removal of all cancerous tissue is very low or when the surgery has a chance of damaging the bladder, vagina or bowel, radiation therapy is used. When a tumor is less than 4 cm in diameter, radiation therapy provides excellent results. In these instances, the 5-year survival rate is greater than 80%.[5] Treatments are individualized due to the rarity of vaginal cancer studies.[13]
 A local surgery to remove vaginal cancer
A local surgery to remove vaginal cancer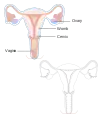 A radical hysterectomy to treat vaginal cancer without reconstruction
A radical hysterectomy to treat vaginal cancer without reconstruction A radical hysterectomy for vaginal cancer with reconstruction of the vagina using other tissues
A radical hysterectomy for vaginal cancer with reconstruction of the vagina using other tissues
Epidemiology
Cancer of the vagina is rare and is only 2% of all gynecological cancers and less than 0.5% of all cancers in women.[5] Estimated new cases in the United States in 2017 are 4,810. Deaths from vaginal during the same time were 1,240.[8] It is more common in older women.[14]
In the UK, 254 cases of Vaginal cancer were identified in 2014. Deaths from vaginal cancer in this period were 110.[15] Out of those with vaginal cancer, 53% are related to HPV infection.[6]
References
- "Unusual Cancers of Childhood Treatment". National Cancer Institute. 1980-01-01. Retrieved 2018-03-09.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Shobeiri, S. Abbas; Rostaminia, Ghazaleh; White, Dena; Quiroz, Lieschen H.; Nihira, Mikio A. (2013-08-01). "Evaluation of Vaginal Cysts and Masses by 3-Dimensional Endovaginal and Endoanal Sonography". Journal of Ultrasound in Medicine. 32 (8): 1499–1507. doi:10.7863/ultra.32.8.1499. ISSN 1550-9613. PMID 23887963.
- "Vaginal and Vulvar Cancer" (PDF). Centers for Disease Control and Prevention. December 2016. Retrieved 18 December 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Symptoms | Vaginal cancer | Cancer Research UK". www.cancerresearchuk.org. 10 September 2015. Retrieved 2017-12-19.
- Mabuchi, Seiji; Kawano, Mahiru; Isohashi, Fumiaki; Kuroda, Hiromasa; Sasano, Tomoyuki; Kimura, Tadashi (2015-01-01). "First two cases of primary carcinoma of the vagina successfully treated with concurrent weekly carboplatin plus paclitaxel, external beam radiotherapy and high-dose-rate interstitial brachytherapy: A case report and published work review". Journal of Obstetrics and Gynaecology Research. 41 (1): 156–161. doi:10.1111/jog.12492. ISSN 1447-0756.
- "Vaginal cancer risk factors". Cancer Research UK. 2015-05-15. Retrieved 2017-12-13.
- "List of Classifications by cancer sites with sufficient or limited evidence in humans, Volumes 1 to 120 a". World Health Organization, International Agency for Research on Cancer. 2017. Retrieved 13 December 2017.
- "Vaginal Cancer Treatment". National Institutes of Health, National Cancer Institute. 9 February 2017. Retrieved 2017-12-13.
- "About DES". Centers for Disease Control and Prevention. Retrieved 2017-12-13.
- "Known Health Effects for DES Daughters". Centers for Disease Control and Prevention. Retrieved 2017-12-13.
- Society of Gynecologic Oncology (February 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, Society of Gynecologic Oncology, retrieved 19 February 2013
- Halperin, Edward C.; Brady, Luther W.; Perez, Carlos A.; Wazer, David E. (2013-05-06). Perez and Brady's principles and practice of radiation oncology. Halperin, Edward C.,, Brady, Luther W., 1925-, Wazer, David E.,, Perez, Carlos A., 1934- (Sixth ed.). Philadelphia. p. 1412. ISBN 9781451116489. OCLC 849739571.
- Damast, Shari; Takiar, Vinita; McCarthy, Shirley; Higgins, Susan A. (2016). "Treatment of early stage vaginal cancer with EBRT and MRI-based intracavitary brachytherapy: A retrospective case review". Gynecologic Oncology Reports. 17: 89–92. doi:10.1016/j.gore.2016.08.002. PMC 4975702. PMID 27536721.
- "Vaginal cancer | Vaginal cancer | Cancer Research UK". www.cancerresearchuk.org. Retrieved 2017-12-19.
- "Vaginal cancer statistics". Cancer Research UK. 2015-05-14. Retrieved 2017-12-13.
External links
| Classification | |
|---|---|
| External resources |