Immunological memory
Immunological memory is the ability of the immune system to quickly and specifically recognize an antigen that the body has previously encountered and initiate a corresponding immune response. Generally these are secondary, tertiary and other subsequent immune responses to the same antigen. Immunological memory is responsible for the adaptive component of the immune system, special T and B cells — the so-called memory T and B cells. Immunological memory is the basis of vaccination.[1][2]
Development of immunological memory
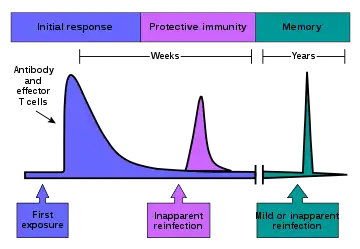
Immunological memory occurs after a primary immune response against the antigen. Immunological memory is thus created by each individual, after a previous initial exposure, to a potentially dangerous agent. The course of secondary immune response is similar to primary immune response. After the memory B cell recognizes the antigen it presents the peptide: MHC II complex to nearby effector T cells. That leads to activation of these cells and rapid proliferation of cells. After the primary immune response has disappeared, the effector cells of the immune response are eliminated.[3] However, there remain antibodies previously created in the body that represent the humoral component of immunological memory and comprise an important defensive mechanism in subsequent infections. In addition to the formed antibodies in the body there remains a small number of memory T and B cells that make up the cellular component of the immunological memory. They stay in the body in a resting state and at the second or next encounter with the same antigen these cells are able to respond immediately and eliminate the antigen. Memory cells have a long life and last up to several decades in the body.[4][2]
Immunity to chickenpox, measles, and some other diseases lasts a lifetime. Immunity to many diseases eventually wears off. The immune system's response to a few diseases, such as dengue, counterproductively makes the next infection worse (antibody-dependent enhancement).[5]
As of 2019, researchers are still trying to find out why some vaccines produce life-long immunity, while the effectiveness of other vaccines drops to zero in less than 30 years (for mumps) or less than six months (for H3N2 influenza).[6]
Memory B cells
Memory B cells are plasma cells that are able to produce antibodies for a long time. Unlike the naive B cells involved in the primary immune response the memory B cell response is slightly different. The memory B cell has already undergone clonal expansion and differentiation and affinity maturation, so it is able to divide multiple times faster and produce antibodies with much higher affinity (especially IgG).[7] In contrast, the naive plasma cell is fully differentiated and can not be further stimulated by antigen to divide or increase antibody production. Memory B cell activity in secondary lymphatic organs is highest during the first 2 weeks after infection. Subsequently, after 2 to 4 weeks its response declines. After the germinal center reaction the memory plasma cells are located in the bone marrow which is the main site of antibody production within the immunological memory.[8]
Memory T cells
Memory T cells can be both CD4+ and CD8+. These memory T cells do not require further antigen stimulation to proliferate; therefore, they do not need a signal via MHC.[9] Memory T cells can be divided into two functionally distinct groups based on the expression of the CCR7 chemokine receptor. This chemokine indicates the direction of migration into secondary lymphatic organs. Those memory T cells that do not express CCR7 (these are CCR7-) have receptors to migrate to the site of inflammation in the tissue and represent an immediate effector cell population. These cells were named memory effector T cells (TEM). After repeated stimulation they produce large amounts of IFN-γ, IL-4 and IL-5. In contrast, CCR7 + memory T cells lack proinflammatory and cytotoxic function but have receptors for lymph node migration. These cells were named central memory T cells (TCM). They effectively stimulate dendritic cells, and after repeated stimulation they are able to differentiate in CCR7- effector memory T cells. Both populations of these memory cells originate from naive T cells and remain in the body for several years after initial immunization.[10]
See also
References
- Travers, Paul, et al. Janeway's immunobiology. Garland Science, 2008.
- Hammarlund, Erika, et al. "Duration of antiviral immunity after smallpox vaccination." Nature medicine 9.9 (2003): 1131.
- Sprent, Jonathan, and Susan R. Webb. "Intrathymic and extrathymic clonal deletion of T cells." Current opinion in immunology 7.2 (1995): 196-205.
- Crotty, Shane, et al. "Cutting edge: long-term B cell memory in humans after smallpox vaccination." The Journal of Immunology 171.10 (2003): 4969-4973.
- Ed Yong. "Immunology Is Where Intuition Goes to Die". 2020. quote: "Immunity lasts a lifetime for some diseases—chickenpox, measles—but eventually wears off for many others." quote: "For some diseases, like dengue, an antibody response to one infection can counterintuitively make the next infection more severe."
- Jon Cohen. "How long do vaccines last?". 2019.
- Travers, Paul, et al. Janeway's immunobiology. Garland Science, 2008
- Slifka, Mark K., Mehrdad Matloubian, and Rafi Ahmed. "Bone marrow is a major site of long-term antibody production after acute viral infection." Journal of Virology 69.3 (1995): 1895-1902.
- Kassiotis, George, et al. "Impairment of immunological memory in the absence of MHC despite survival of memory T cells." Nature immunology 3.3 (2002): 244.
- Sallusto, Federica, et al. "Two subsets of memory T lymphocytes with distinct homing potentials and effector functions." Nature 401.6754 (1999): 708.