Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm (IPMN) is a type of tumor that can occur within the cells of the pancreatic duct. IPMN tumors produce mucus,[1] and this mucus can form pancreatic cysts.[2] Although intraductal papillary mucinous neoplasms are benign tumors, they can progress to pancreatic cancer.[1] As such IPMN is viewed as a precancerous condition.[3] Once an intraductal papillary mucinous neoplasm has been found, the management options include close monitoring and pre-emptive surgery.
| Intraductal papillary mucinous neoplasm | |
|---|---|
| Other names | IPMN |
 | |
| Intraductal papillary mucinous neoplasm in magnetic resonance imaging. | |
| Specialty | Gastroenterology |
| Symptoms | Usually asymptomatic |
| Usual onset | 50-70 years of age |
| Types | Main duct, branch duct or mixed |
| Risk factors | Male gender |
| Differential diagnosis | Mucinous cystic neoplasm |
| Treatment | Imaging surveillance, surgical resection |
Histology
IPMNs are lined with mucin-secreting columnar epithelium.
Diagnosis
In most cases, IPMNs are diagnosed based on clinical and radiographic criteria.[5] If fluid from the cyst is aspirated, the CEA level is typically elevated.[5] Confirmation of the diagnosis with tissue is rarely necessary.[5]
By histopathology, IPMN is characterized on light microscopy by Mucinous epithelial cells,[6] and growth within the pancreatic ducts.[7] Mucin 5AC is a useful immunohistochemistry marker.[8] Characteristic genetic alterations are those of KRAS and GNAS.[8]
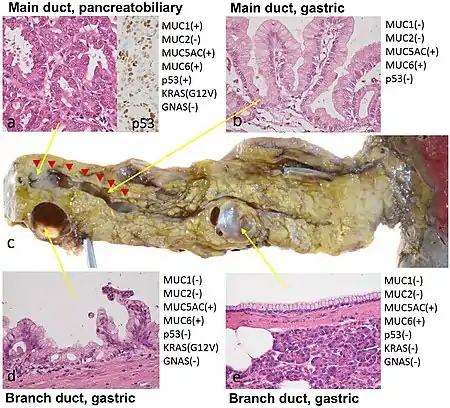
Further subtyping of IPMN can be done as either:[9]
- Gross pathology: Main duct, branch duct, and mixed duct lesions, which determines surgical management. Main duct lesion is the segmental or diffuse dilatation of main pancreatic duct greater than 5 mm without other causes of obstruction. Meanwhile, branch duct lesion is the pancreatic cyst more than 5 mm that communicates with the main duct. The mixed duct lesions fulfills both criteria above.[10]
- By light microscopy and immunohistochemistry:[11] Gastric, intestinal, pancreaticbiliary, and oncocytic.
Treatment
The treatment of choice for main-duct IPMNs is resection due to approximately 50% chance of malignancy. Side-branch IPMNs are occasionally monitored with regular CT or MRIs, but most are eventually resected, with a 30% rate of malignancy in these resected tumors. Indications for surgical resection include obstructive jaundice, an enhancing mural nodule >5 mm, and pancreatic duct dilation (>10 mm).[12]
Surgery can include the removal of the head of the pancreas (a pancreaticoduodenectomy), removal of the body and tail of the pancreas (a distal pancreatectomy), or rarely removal of the entire pancreas (a total pancreatectomy).[13] In selected cases the surgery can be performed using minimally invasive techniques such as laparoscopy[14] or robotic surgery. A study using Surveillance, Epidemiology, and End Results Registry (SEER) data suggested that increased lymph node counts harvested during the surgery were associated with better survival in invasive IPMN patients.[15]
Prognosis
Survival 5 years after resection of an IPMN without malignancy is approximately 80%, 85% with malignancy but no lymph node spread and 0% with malignancy spreading to lymph nodes.[16]
Epidemiology
Side branch IPMNs are the most common pancreatic cysts.[5] IPMNs occur more often in men than women, and often occur in the 6th and 7th decade of life.
History
In 1982, IPMN was reported as a "mucin-producing tumor" by Kazuhiko Ohashi of the Japanese Foundation for Cancer Research.
References
- "Intraductal Papillary Mucinous Neoplasms of the Pancreas". Johns Hopkins University. Retrieved 7 September 2009.
- Campbell, NM; Katz, SS; Escalon, JG; Do, RK (March 2015). "Imaging patterns of intraductal papillary mucinous neoplasms of the pancreas: an illustrated discussion of the International Consensus Guidelines for the Management of IPMN". Abdominal Imaging. 40 (3): 663–77. doi:10.1007/s00261-014-0236-4. PMID 25219664. S2CID 10097983.
- "Precancerous conditions of the pancreas - Canadian Cancer Society". www.cancer.ca. Retrieved 5 November 2017.
- Shibata, Hideki; Ohike, Nobuyuki; Norose, Tomoko; Isobe, Tomohide; Suzuki, Reika; Imai, Hideyuki; Shiokawa, Akira; Takimoto, Masafumi; Tabuchi, Akihiro; Takano, Yuichi; Yamamura, Eiichi; Nagahama, Masatsugu; Takeyama, Nobuyuki; Yokomizo, Kazuaki; Mizukami, Hiroki; Tanaka, Jun-ichi; Aoki, Takeshi; Murakami, Masahiko (2017). "A resected case of two branch duct-type intraductal papillary mucinous neoplasms showing different clinical courses after a two-year follow-up". Clinical Journal of Gastroenterology. 10 (3): 274–278. doi:10.1007/s12328-017-0728-1. ISSN 1865-7257. PMC 5429895. PMID 28258561.-
"This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/)" - Elta, GH; Enestvedt, BK; Sauer, BG; Lennon, AM (April 2018). "ACG Clinical Guideline: Diagnosis and Management of Pancreatic Cysts". The American Journal of Gastroenterology. 113 (4): 464–479. doi:10.1038/ajg.2018.14. PMID 29485131. S2CID 3584079.
- Diana Agostini-Vulaj. "Pancreas - Exocrine tumors / carcinomas - Intraductal papillary mucinous neoplasm (IPMN)". Pathology Outlines. Topic Completed: 1 July 2018. Revised: 9 March 2020
- Adsay, Volkan; Mino-Kenudson, Mari; Furukawa, Toru; Basturk, Olca; Zamboni, Giuseppe; Marchegiani, Giovanni; Bassi, Claudio; Salvia, Roberto; Malleo, Giuseppe; Paiella, Salvatore; Wolfgang, Christopher L.; Matthaei, Hanno; Offerhaus, G. Johan; Adham, Mustapha; Bruno, Marco J.; Reid, Michelle D.; Krasinskas, Alyssa; Klöppel, Günter; Ohike, Nobuyuki; Tajiri, Takuma; Jang, Kee-Taek; Roa, Juan Carlos; Allen, Peter; Castillo, Carlos Fernández-del; Jang, Jin-Young; Klimstra, David S.; Hruban, Ralph H. (2016). "Pathologic Evaluation and Reporting of Intraductal Papillary Mucinous Neoplasms of the Pancreas and Other Tumoral Intraepithelial Neoplasms of Pancreatobiliary Tract". Annals of Surgery. 263 (1): 162–177. doi:10.1097/SLA.0000000000001173. ISSN 0003-4932. PMC 4568174. PMID 25775066.
- Pishvaian MJ, Brody JR (2017). "Therapeutic Implications of Molecular Subtyping for Pancreatic Cancer". Oncology (Williston Park). 31 (3): 159–66, 168. PMID 28299752.
- Salvia, Roberto (2010). "Differences between main-duct and branch-duct intraductal papillary mucinous neoplasms of the pancreas". World Journal of Gastrointestinal Surgery. 2 (10): 342–6. doi:10.4240/wjgs.v2.i10.342. ISSN 1948-9366. PMC 2999210. PMID 21160841.
- Aronsson, Linus; Andersson, Roland; Ansari, Daniel (2017-08-03). "Intraductal papillary mucinous neoplasm of the pancreas – epidemiology, risk factors, diagnosis, and management". Scandinavian Journal of Gastroenterology. 52 (8): 803–815. doi:10.1080/00365521.2017.1318948. ISSN 0036-5521. PMID 28446039. S2CID 13772106.
- Ishida, Masaharu; Egawa, Shinichi; Aoki, Takeshi; Sakata, Naoaki; Mikami, Yukio; Motoi, Fuyuhiko; Abe, Tadayoshi; Fukuyama, Shoji; Sunamura, Makoto; Unno, Michiaki; Moriya, Takuya; Horii, Akira; Furukawa, Toru (2007). "Characteristic Clinicopathological Features of the Types of Intraductal Papillary-Mucinous Neoplasms of the Pancreas". Pancreas. 35 (4): 348–352. doi:10.1097/mpa.0b013e31806da090. ISSN 0885-3177. PMID 18090241. S2CID 22028911.
- Tanaka, M; Fernández-Del Castillo, C; Kamisawa, T; Jang, JY; Levy, P; Ohtsuka, T; Salvia, R; Shimizu, Y; Tada, M; Wolfgang, CL (October 2017). "Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas". Pancreatology. 17 (5): 738–753. doi:10.1016/j.pan.2017.07.007. PMID 28735806.
- "Pancreatic Surgery". Johns Hopkins University. Retrieved 7 September 2009.
- "Laproscopic Pancreatic Surgery". Johns Hopkins University. Retrieved 7 September 2009.
- Wu, WM (Sep 2014). "An increased total resected lymph node count benefits survival following pancreas invasive intraductal papillary mucinous neoplasms resection: an analysis using the surveillance, epidemiology, and end result registry database". PLOS ONE. 9 (9): e107962. Bibcode:2014PLoSO...9j7962W. doi:10.1371/journal.pone.0107962. PMC 4179272. PMID 25264746.
- Sohn, Taylor (June 2004). "Intraductal Papillary Mucinous Neoplasms of the Pancreas". Annals of Surgery. 239 (6): 788–799. doi:10.1097/01.sla.0000128306.90650.aa. PMC 1356287. PMID 15166958.