Vertebral artery
The vertebral arteries are major arteries of the neck. Typically, the vertebral arteries originate from the subclavian arteries. Each vessel courses superiorly along each side of the neck, merging within the skull to form the single, midline basilar artery. As the supplying component of the vertebrobasilar vascular system, the vertebral arteries supply blood to the upper spinal cord, brainstem, cerebellum, and posterior part of brain.[1]
| Vertebral artery | |
|---|---|
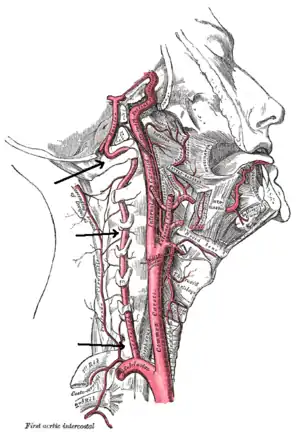 Arteries of the neck. The vertebral arteries arise from the subclavian arteries and join to form the basilar artery | |
| Details | |
| Source | Subclavian artery |
| Branches | Basilar artery Posterior spinal artery Anterior spinal artery Posterior inferior cerebellar artery |
| Vein | Vertebral vein |
| Identifiers | |
| Latin | Arteria vertebralis |
| MeSH | D014711 |
| TA98 | A12.2.08.002 |
| TA2 | 4538 |
| FMA | 3956 |
| Anatomical terminology | |
Structure
The vertebral arteries usually arise from the posterosuperior aspect of the central subclavian arteries on each side of the body,[2] then enter deep to the transverse process at the level of the 6th cervical vertebrae (C6),[1] or occasionally (in 7.5% of cases) at the level of C7. They then proceed superiorly, in the transverse foramen of each cervical vertebra.[1] Once they have passed through the transverse foramen of C1 (also known as the atlas), the vertebral arteries travel across the posterior arch of C1 and through the suboccipital triangle before entering the foramen magnum.[1]
Nunziante Ippolito, a Neapolitan physician, identified the "angle of Nunziante Ippolito" to find the vertebral artery, between the anterior scalene muscle and the longus colli muscle.[3]
Inside the skull, the two vertebral arteries join to form the basilar artery at the base of the pons. The basilar artery is the main blood supply to the brainstem and connects to the Circle of Willis to potentially supply the rest of the brain if there is compromise to one of the carotids. At each cervical level, the vertebral artery sends branches to the surrounding musculature via the anterior spinal arteries.
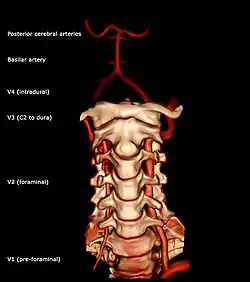
The vertebral artery may be divided into four parts:
- The first (preforaminal) part runs upward and backward between the Longus colli and the Scalenus anterior. In front of it are the internal jugular and vertebral veins, and it is crossed by the inferior thyroid artery; the left vertebral is crossed by the thoracic duct also. Behind it are the transverse process of the seventh cervical vertebra, the sympathetic trunk and its inferior cervical ganglion
- The second (foraminal) part runs upward through the transverse foramina of the C6 to C2 vertebrae, and is surrounded by branches from the inferior cervical sympathetic ganglion and by a plexus of veins which unite to form the vertebral vein at the lower part of the neck. It is situated in front of the trunks of the cervical nerves, and pursues an almost vertical course as far as the transverse process of the axis.
- The third (extradural or atlantic) part issues from the C2 foramen transversarium on the medial side of the Rectus capitis lateralis. It is further subdivided into the vertical part V3v passing vertically upwards, crossing the C2 root and entering the foramen transversarium of C1, and the horizontal part V3h, curving medially and posteriorly behind the superior articular process of the atlas, the anterior ramus of the first cervical nerve being on its medial side; it then lies in the groove on the upper surface of the posterior arch of the atlas, and enters the vertebral canal by passing beneath the posterior atlantoöccipital membrane. This part of the artery is covered by the Semispinalis capitis and is contained in the suboccipital triangle—a triangular space bounded by the Rectus capitis posterior major, the Obliquus superior, and the Obliquus inferior. The first cervical or suboccipital nerve lies between the artery and the posterior arch of the atlas.
- The fourth (intradural or intracranial) part pierces the dura mater and inclines medialward to the front of the medulla oblongata; it is placed between the hypoglossal nerve and the anterior root of the first cervical nerve and beneath the first digitation of the ligamentum denticulatum. At the lower border of the pons it unites with the vessel of the opposite side to form the basilar artery.
Triangle
Triangle of the vertebral artery is a region within the root of the neck and has following boundaries:[4]
- Medial border of anterior scalene muscle (lateral)
- Lateral border of longus colli muscle (medial)
- Carotid tubercle (apex)
- First part of subclavian artery (base)
The vertebral artery runs from base to apex (prior to entering the transverse foramen of 6th cervical vertebra).
The carotid tubercle separates the vertebral artery which passes directly behind it from the common carotid artery which lies directly in front of it. The ideal site for palpating the carotid pulse is to gently press the common carotid artery against the carotid tubercle.[5]
Variation
There is commonly variations in the course and size of the vertebral arteries. For example, differences in size between left and right vertebral arteries may range from a slight asymmetry to marked hypoplasia of one side, with studies estimating a prevalence of unilateral vertebral artery hypoplasia between 2% to 25%.[6] In 3-15% of the population, a bony bridge called the arcuate foramen covers the groove for the vertebral artery on vertebra C1. Rarely, the vertebral arteries enter the subarachnoid space at C1-C2 (3%) or C2-C3 (only three cases have been reported) vertebral levels instead of the atlanto-occipital level.[7]
Function
As the supplying component of the vertebrobasilar vascular system, the vertebral arteries supply blood to the upper spinal cord, brainstem, cerebellum, and posterior part of brain.[1]
Clinical significance
As the supplying component of the vertebrobasilar vascular system, the vertebral arteries supply blood to the upper spinal cord, brainstem, cerebellum, and posterior part of brain.[1] A stroke of the arteries may result in a posterior circulation stroke.
Additional images
 The arteries of the base of the brain.
The arteries of the base of the brain.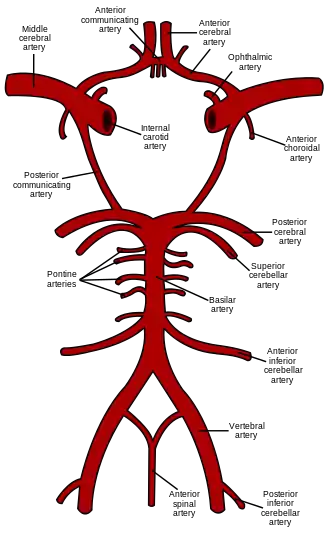 Diagram of the arterial circulation at the base of the brain.
Diagram of the arterial circulation at the base of the brain. Relationship of the vertebral artery to the suboccipital muscles.
Relationship of the vertebral artery to the suboccipital muscles.
References
- Standing S, Borely NR, Collins P, Crossman AR, Gatzoulis MA, Healy GC, et al. (2008). Gray's Anatomy: The Anatomical Basis of Clinical Practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
- Yuan SM (February 2016). "Aberrant Origin of Vertebral Artery and its Clinical Implications". Brazilian Journal of Cardiovascular Surgery. 31 (1): 52–9. doi:10.5935/1678-9741.20150071. PMC 5062690. PMID 27074275.
- "Ippolito, Nunziante". Trecanni.
- Campero, A.; Rubino, P. A.; Rhoton, L. Jr. (2011). Pathology and surgery around the vertebral artery. Paris: Springer. p. 29. ISBN 978-2-287-89787-0.
- Tubbs RS, Salter EG, Wellons JC, Blount JP, Oakes WJ (April 2005). "The triangle of the vertebral artery". Neurosurgery. 56 (suppl. 4): 252–5. doi:10.1227/01.neu.0000156797.07395.15. PMID 15794821.
- Park JH, Kim JM, Roh JK (September 2007). "Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory". Journal of Neurology, Neurosurgery, and Psychiatry. 78 (9): 954–8. doi:10.1136/jnnp.2006.105767. PMC 2117863. PMID 17098838.
- Moon, Jong Un; Kim, Myoung Soo (September 1, 2019). "C3 segmental vertebral artery diagnosed by computed tomography angiography". Surgical and Radiologic Anatomy. 41 (9): 1075–1078. doi:10.1007/s00276-019-02193-z. ISSN 1279-8517. PMID 30762086.
External links
| Wikimedia Commons has media related to Vertebral artery. |
- Anatomy photo:28:09-0201 at the SUNY Downstate Medical Center
- http://neuroangio.org/anatomy-and-variants/vertebral-artery/
- MedEd at Loyola Neuro/neurovasc/navigation/vert.htm
- Atlas image: n3a8p1 at the University of Michigan Health System
- lesson5 at The Anatomy Lesson by Wesley Norman (Georgetown University) (vertebralcolumnfromleftweb)
- "Anatomy diagram: 13048.000-1". Roche Lexicon - illustrated navigator. Elsevier. Archived from the original on January 1, 2014.
- "Anatomy diagram: 13048.000-3". Roche Lexicon - illustrated navigator. Elsevier. Archived from the original on January 1, 2014.