Anterior cruciate ligament reconstruction
Anterior cruciate ligament reconstruction (ACL reconstruction) is a surgical tissue graft replacement of the anterior cruciate ligament, located in the knee, to restore its function after an injury.[1] The torn ligament can either be removed from the knee (most common), or preserved (where the graft is passed inside the preserved ruptured native ligament) before reconstruction an arthroscopic procedure. ACL repair is also a surgical option. This involves repairing the ACL by re-attaching it, instead of performing a reconstruction. Theoretical advantages of repair include faster recovery[2] and a lack of donor site morbidity, but randomised controlled trials and long-term data regarding re-rupture rates using contemporary surgical techniques are lacking.
| Anterior cruciate ligament reconstruction | |
|---|---|
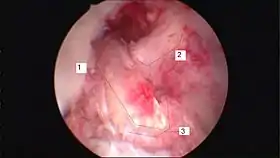 Arthroscopic anterior cruciate ligament (ACL) reconstruction (right knee). The tendon of the semitendinosus muscle was prelevated, folded and used as an autograft (1). It appears through the remnant of the injured original ACL (3). The autograft then courses upwardly and backwardly in front of the posterior cruciate ligament (2). | |
| Other names | ACL reconstruction |
| ICD-9-CM | 81.45 |
| MedlinePlus | 007208 |
Background
The Anterior Cruciate Ligament is the ligament that keeps the knee stable.[3] Anterior Cruciate Ligament damage is a very common injury, especially among athletes. Anterior Cruciate Ligament Reconstruction (ACL) surgery is a common intervention. 1 in every 3,000 American suffers from a ruptured ACL and between 100,000 and 300,000 reconstruction surgeries will be performed each year in the United States.[4][5] Around $500 million health care dollar will come from ACL injuries. ACL injuries can be categorized into groups- contact and non-contact based on the nature of the injury[6] Contact injuries occur when a person or object come into contact with the knee causing the ligament to tear. However, non-contact tears typically occur during the following movements: decelerating, cutting, or landing from a jump. ACL injury is 4-6 times higher in females than in males. An increased Q angle and hormonal differences are a few examples of the gender disparity in ACL tear rates.[7]
Types of grafts

Graft options for ACL reconstruction include:
- Autografts (employing bone or tissue harvested from the patient's body).
- Allografts (using bone or tissue from another body, either a cadaver or a live donor).
- Bridge-enhanced ACL repair (using a bio-engineered bridging scaffold injected with the patient's own blood).
- Synthetic tissue for ACL reconstruction has also been developed, but little data exists on its strength and reliability.
Autograft
An accessory hamstring or part of the patellar ligament are the most common donor tissues used in autografts. While originally less commonly utilized, the quadriceps tendon has become a more popular graft.[8][9]
Because the tissue used in an autograft is the patient's own, the risk of rejection is minimal. The retear rate in young, active individuals has been shown to be lower when using autograft as compared to allograft.[8]
Hamstring tendon

Hamstring autografts are made with the semitendinosus tendon, either alone or accompanied by the gracilis tendon for a stronger graft. The semitendinosus is an accessory hamstring (the primary hamstrings are left intact), and the gracilis is not a hamstring, but an accessory adductor (the primary adductors are left intact as well). The two tendons are commonly combined and referred to as a four-strand hamstring graft, made by a long piece (about 25 cm) removed from each tendon. The tendon segments are folded and braided together to form a tendon of quadruple thickness for the graft. The braided segment is threaded through the heads of the tibia and femur, and its ends are fixed with screws on the opposite sides of the two bones.
Unlike the patellar ligament, the hamstring tendon's fixation to the bone can be affected by motion after surgery. Therefore, a brace is often used to immobilize the knee for one to two weeks. Evidence suggests that the hamstring tendon graft does as well, or nearly as well, as the patellar ligament graft in the long term.[10] Common problems during recovery include strengthening of the quadriceps, IT-band, and calf muscles.
The main surgical wound is over the upper proximal tibia, which prevents the typical pain experienced when kneeling after surgery. The wound is typically smaller than that of a patellar ligament graft, and so causes less post-operative pain. Another option first described in 2004, a minimally invasive technique for harvesting from the back of the knee, is faster, produces a significantly smaller wound, avoids the complications of graft harvesting from the anterior incision, and decreases the risk of nerve injury.[11]
There is some controversy as to how well a hamstring tendon regenerates after the harvesting. Most studies suggest that the tendon can be regenerated at least partially, though it will still be weaker than the original tendon.[12][13]
Advantages of hamstring grafts include their high "load to failure" strength, the stiffness of the graft, and the low postoperative morbidity. The natural ACL can withstand a load of up to 2,160 newtons. With a hamstring graft, this number doubles, decreasing the risk of re-injury. The stiffness of a hamstring graft—quadruple that of the natural ACL (Bartlett, Clatworthy and Ngugen, 2001)—also reduces the risk of re-injury.
Patellar tendon

The patellar tendon connects the patella (kneecap) to the tibia (shin). The graft is normally taken from the injured knee, but in some circumstances, such as a second operation, the other knee may be used. The middle third of the tendon is used, with bone fragments removed on each end. The graft is then threaded through holes drilled in the tibia and femur, and screwed into place. It is slightly larger than a hamstring graft.
Disadvantages compared with a hamstring graft include:
- Increased wound pain
- Increased scar formation
- Risk of fracturing the patella during harvesting of the graft
- Increased risk of tendinitis.
- Increased pain levels, even years after surgery, with activities that require kneeling.[14]
Some or all of these disadvantages may be attributable to post-operative patellar tendon shortening.[15]
The rehabilitation after the surgery is different for each knee. The beginning rehab for the ACL graft knee is focused on reducing swelling, gaining full range of motion, and stimulating the leg muscles. The goal for the graft donor need is to immediately start high repetition strength training exercises.[16]
Allograft
The patellar ligament, tibialis anterior tendon, or Achilles tendon may be recovered from a cadaver and used in ACL reconstruction. The Achilles tendon, because of its large size, must be shaved to fit within the joint cavity.
Type
Typically, age and lifestyle help determine the type of graft used for ACL reconstruction.[14] The biggest factors in knee stability are correct graft placement by the surgeon and treatment of other menisco-ligament injuries in the knee, rather than type of graft. Bone-patellar tendon-bone grafts have resulted fewer failures and more stability on KT-1000 arthrometer testing.[17][18]
Site
No ideal graft site for ACL reconstruction exists. Surgeons have historically regarded patellar tendon grafts as the "gold standard" for knee stability.[14]
Hamstring grafts historically had problems with fixation slippage and stretching out over time. Modern fixation methods avoid graft slippage and produce similarly stable outcomes with easier rehabilitation, less anterior knee pain and less joint stiffness.
Although there is less experience with the use of tibialis anterior grafts, preliminary data has shown no difference in short-term subjective outcomes between tibialis anterior allografts and patellar tendon allografts.[19]
The quadriceps tendon, while historically reserved for revision reconstructions, has enjoyed a renewed focus as a versatile and durable graft for primary reconstructions. Use of the quadriceps tendon usually does not result in the same degree of anterior knee pain postoperatively, and quadriceps tendon harvest produces a reliably thick, robust graft. The quadriceps tendon has approximately 20% greater collagen per cross-sectional area than the patellar tendon, and a greater diameter of usable soft tissue is available.
Bridge Enhanced ACL Repair (BEAR Implant)
A new approach to treating ACL tears was developed at Boston Children's Hospital and is currently in clinical trials.[20] The Bridge Enhanced ACL Repair (BEAR) implant is a bio-engineered bridging scaffold that is injected with a small amount of patient's own blood to stimulate healing and reconnection of the ACL. Results from the first-in-human study published in March 2019 in the Orthopedic Journal of Sports Medicine showed the 10 patients who received the BEAR implant had similar clinical, functional and patient-reported outcomes as the 10 patients undergoing autograft ACL reconstruction.[21] Additional clinical studies are underway.[22]
Stem cell treatment
Autologous stem-cell transplantation using mesenchymal stem cells (MSCs) has been used to improve recovery time from ACL surgery, especially for athletes. MSCs are multipotent stem cells, meaning they can differentiate into multiple cell types. In the case of mesenchymal stem cells, these cell types include osteoblasts (bone cells), adipocytes (fat cells), and chondrocytes (cartilage cells). Ligament tissue mainly consists of fibroblasts and extracellular matrix. Ligament cells differ in size, respond to different cues in the cell environment, and express different cell surface markers, limiting the number of clinical treatments for accelerated repair of ACL tissue to MSCs and primary fibroblasts obtained from other ACL tissue. Therefore, most modern stem cell injections use MSCs to promote faster repair of the ACL and allow people such as athletes to return to their previous form faster.
In order for MSCs to differentiate into an ACL, they must be placed in a proper scaffold on which to grow, and must be in a bioreactor that maintains a normal physiological environment for the cells to reproduce and proliferate effectively.[23] The scaffold must have the mechanical properties of a healthy ACL to sustain the ligament while it is in its primary form and maintain normal knee movement. Scaffolds that are used for ACL growth include collagen, silk, gelatin, polylactic acid, and glycosaminoglycans.[24] Mechanical properties of the scaffolds are further enhanced through braiding and twisting of the scaffold materials.
The bioreactor must have similar properties to a knee joint so that when the ACL is inserted into the body, it is not rejected as foreign, which could cause infection. Therefore, it has to have compatible pH levels, oxygen concentration levels, metabolite levels and temperature, in addition to being sterile.[25]
Recovery
Initial physical therapy consists of range of motion (ROM) exercises, often with the guidance of a physical therapist. Range of motion exercises are used to regain the flexibility of the ligament, prevent or break down scar tissue from forming and reduce loss of muscle tone. Range of motion exercise examples include: quadriceps contractions and straight leg raises. In some cases, a continuous passive motion (CPM) device is used immediately after surgery to help with flexibility. The preferred method of preventing muscle loss is isometric exercises that put zero strain on the knee. Knee extension within two weeks is important with many rehab guidelines.
Perturbation training can help improve gait asymmetries of the knee joint.[26][27]
Approximately six weeks is required for the bone to attach to the graft. However, the patient can typically walk on their own and perform simple physical tasks prior to this with caution, relying on the surgical fixation of the graft until true healing (graft attachment to bone) has taken place. At this stage, the first round of physical therapy can begin. This usually consists of careful exercises to regain flexibility and small amounts of strength. One of the more important benchmarks in recovery is the twelve weeks post-surgery period. After this, the patient can typically begin a more aggressive regimen of exercises involving stress on the knee, and increasing resistance. Jogging may be incorporated as well.
After four months, more intense activities such as running are possible without risk. After five months, light ball work may commence as the ligament is nearly regenerated. After six months, the reconstructed ACL is generally at full strength (ligament tissue has fully regrown), and the patient may return to activities involving cutting and twisting if a brace is worn. Recovery varies highly from case to case, and sometimes resumption of stressful activities may take a year or longer.
Risks
If the proper rehabilitation procedure is not followed out post surgery, the ACL becomes less mobile and the bones begin to rub against each other. The abnormal bone movement can also damage the tissue, this damage can lead to osteoarthritis.[28]
Rehabilitation
The recovery process for the ACL is usually broken down into different phases of rehabilitation. Each phase has its own objectives, however is intertwined with other phases since the goals are as progressive as the recovery itself. The rehabilitation process is at the pace of the patient. Timelines are sometimes given to help give an idea of where one can be during rehabilitation. Timelines are not used to discourage or encourage those who aren’t ready to advance their recovery process. Such acts may cause serious injury or re-injury of the ACL.
Phase 1
This phase begins immediately post surgery while the patient is still on crutches and in cast, which they're projected to be using for seven to ten days During this phase the patient will begin seeing a physical therapist that will discuss the main goals of rehabilitation. Some of these goals include: reducing pain and inflammation, increasing range of motion, strengthen surrounding muscles, and begin weight bearing exercises. Extension deficit is a frequent issue after surgery and is often related to arthrogenic muscle inhibition.[29] Specific exercises and cryotherapy are proven to be effective in addressing arthrogenic muscle inhibition.[30] If the patient used a patellar tendon graft for their reconstructed ACL, therapist will also work on mobilizing the patellar tendon to keep it from shortening.
Some equipment that can be used and exercises that can be performed are:
- Use of Cryo-cuff
- - provides cold compression
- Isometric Contraction of Quads
- Quad Sets
- - stand against wall, push extended knee against rolled towel
- - progress to straight leg raised to 30deg.
- Wall Slides
- - To increase knee flexion
- Assisted Knee Flexion
- Towel Squeeze
- - Sit in chair, squeeze rolled towel between knees for 5 seconds. Relax & repeat.
- VMO Strengthening Exercise
- Supported Bilateral Calf-Raises
- walk without crutches
- Swimming (Freestyle front crawl)
This particular swimming technique encompasses all the muscles in the knee and will increase not only mobility but also the strength of the surrounding muscles, which include the quadriceps, hamstrings, gastrocnemius, tibialis anterior (shin muscle), abductor hallucis, abductor digiti minimi, and flexor digitorum brevis (foot muscles).
Phase 2
Many of the goals from phase I will be continued to the following phases until they have been reached. Some of these goals are reducing pain, swelling, and increasing the knee's range of motion is still crucial during this phase. Physical therapist may begin to incorporate core exercises as well as light weight exercises to strengthen the surrounding muscles and hips. Some examples of these exercises include the usage of resistance/stretch bands, stationary biking, and elliptical. During this phase the patient may begin performing more strenuous exercises such as half-squatting and partial lunges.
Some exercises that can be performed are:
- Mini squats
- - Progress to full squats → single-leg half squat
- Mini Lunges
- - Progress to full lunges
- Leg Press
- - Double-leg → single
- Step-ups
- Bridges
- - Double-leg → single
- - Floor → Swiss ball
- Hip Abduction w/ Theraband
- Hip Extension w/ Theraband
- Wobble board
- - Assisted → un-assisted → eyes closed (assisted → unassisted)
- Stork Stand
- - Assisted → un-assisted → eyes closed (assisted → unassisted) → unstable surface
- Static Proprioceptive hold/ball throwing
- Functional Exercises that can be performed at this time include:
- - Walking
- - Bike
- - Roman Chair
Phase 3
Patients will continue to work on decreasing pain/swelling and building up their strength. Lateral movement, jogging in a straight line, single-leg squats and exercises will start to be incorporated as patient begins to regain confidence in the knee. Building strength in the hips with lateral stepping as well as step-ups and step-downs will still be a strong focus in this phase.
Some exercises that can be performed are:
- Continue exercises from Phase 2, progress as necessary
- Jump & Land drills
- - Jump from block & stick landing
- - Double-leg landing → single-leg
- Plyometric Drills
- - Jumping over blocks, sideways & forward
- - Hopping up & down steps/stairs
Phase 4
By this time the range of motion should be greater than 110 degrees flexed and the patient's bodily mechanics like walking and light jogging should be back to normal (before operation). Single leg exercises will be continued as well as balancing activities to strengthen the core and lower body. Stamina and endurance should be improved for exercises such as: biking, jogging, and step-ups/downs. If by this time the patient does not have 110 degrees of flexion in the knee, they are advised to see their therapist or surgeon. There's a chance that the knee could need another operation to increase the elasticity of the ligament.
The goal of this phase is a return to activity, however it requires an ability to perform some functional performance tests such as:
- Agility Tests
- Illinois Agility Test
- Zig Zag Agility Test
- These tests are used to test the ability of the knee to withstand cutting and planting maneuvers.
- Single Leg Step-Down Tests
- These tests can be used to identify any hip and core musculature weaknesses before cleared for return-to-play.
- Single Leg Step-Down Tests
- Standing Vertical Jump
- The patient jumps straight in the air from a standing start and lands on two feet as stable as possible.
- Heiden Hop Test
- The patient jumps as far as possible with the uninjured leg and lands on the injured leg. A patient's ability to stick the landing is indicative of good knee function.
- Isokinetic Testing
- This is used to evaluate muscle strength.
- The individual should have at least 90% quadricep strength of the uninjured leg.
- They should also have equal hamstring strength to their uninjured leg as well.
Phase 5
This is the last phase of the recovery rehabilitation. Phase V includes returning to sports after being cleared by therapist or surgeon. In order for this to happen the patient must have full range of motion, continue maintaining strength and endurance, and be able to increase proprioception with agility drills. Patient is still to be aware that going down hill or down stairs while the knee is aggravated may cause further injury like a meniscus tear.
Cost of procedure
The cost of an ACL reconstruction surgery will vary due to a few different reasons such as where a patient lives, which graft is used, if the meniscus is also torn, and the coverage of the patient's insurance. A study has shown in 2016 that metropolitan areas, of at least one million residents, located on the western coast of the United States of America and areas like Minnesota, Indiana, and Michigan were more expensive than the East and South East coast of the United States.[31] Another study, conducted by Baylor University, found that ACL reconstruction procedures using the bone-patella tendon-bone technique took 2.5 hours longer than using a hamstring graft. The operation room costs and hospital charges for that amount of extra time came to about $1,580 more expensive.[32] This also applies to having a torn meniscus during the procedure. Fixing the torn cartilage will increase the procedure time, increasing cost. Insurance plays the biggest role in cost for an ACL reconstruction since that it will be covering majority of the costs. The coverage of a patient's plan, deductibles, and insurance company will determine how much he or she will pay in copays.[33]
Despite the complexity of the procedure and numerous doctor's visits involved, 80–90% of patients who have had the surgery said they had favorable results.[34]
References
- "Anterior Cruciate Ligament (ACL) Injuries". www.webmd.com. Retrieved 25 April 2016.
- Praz, Cesar; Kandhari, Vikram Kishor; Saithna, Adnan; Sonnery-Cottet, Bertrand (March 2019). "ACL rupture in the immediate build-up to the Olympic Games: return to elite alpine ski competition 5 months after injury and ACL repair". BMJ Case Reports. 12 (3): e227735. doi:10.1136/bcr-2018-227735. ISSN 1757-790X. PMC 6424301. PMID 30878956.
- "Anterior Cruciate Ligament (ACL) Injuries – Topic Overview". WebMD. Retrieved 22 April 2015.
- Baer GS, Harner CD (October 2007). "Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction". Clin Sports Med. 26 (4): 661–81. doi:10.1016/j.csm.2007.06.010. PMID 17920959.
- Cohen SB, Yucha DT, Ciccotti MC, Goldstein DT, Ciccotti MA, Ciccotti MG (September 2009). "Factors affecting patient selection of graft type in anterior cruciate ligament reconstruction". Arthroscopy. 25 (9): 1006–10. doi:10.1016/j.arthro.2009.02.010. PMID 19732639.
- Stats on ACL injuries .
- Anatomy and Gender Disparity of ACL injuries Archived April 2, 2015, at the Wayback Machine
- "ACL Reconstruction Information". Retrieved 11 June 2019.
- Ouabo, Eric Choudja; Gillain, Laurent; Saithna, Adnan; Blanchard, Jacques; Siegrist, Olivier; Sonnery-Cottet, Bertrand (July 2019). "Combined Anatomic Anterior Cruciate and Anterolateral Ligament Reconstruction With Quadriceps Tendon Autograft and Gracilis Allograft Through a Single Femoral Tunnel". Arthroscopy Techniques. 8 (8): e827–e834. doi:10.1016/j.eats.2019.03.021. PMC 6823836. PMID 31700778.
- Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (April 2007). "A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial". Am J Sports Med. 35 (4): 564–74. doi:10.1177/0363546506296042. PMID 17261567. S2CID 73233440.
- Kodkani PS, Govekar DP, Patankar HS (October 2004). "A new technique of graft harvest for anterior cruciate ligament reconstruction with quadruple semitendinosus tendon autograft". Arthroscopy. 20 (8): e101–4. doi:10.1016/j.arthro.2004.07.016. PMID 15483531.
- Okahashi K, Sugimoto K, Iwai M, Oshima M, Samma M, Fujisawa Y, Takakura Y (June 2006). "Regeneration of the hamstring tendons after harvesting for arthroscopic anterior cruciate ligament reconstruction: a histological study in 11 patients". Knee Surg Sports Traumatol Arthrosc. 14 (6): 542–5. doi:10.1007/s00167-006-0068-z. PMID 16525795. S2CID 7147812.
- Gill, Sanjitpal S.; Turner, Maria A.; Battaglia, Todd C.; Leis, Henry T.; Balian, Gary; Miller, Mark D. (July 2004). "Semitendinosus Regrowth: Biochemical, Ultrastructural, and Physiological Characterization of the Regenerate Tendon". The American Journal of Sports Medicine. The American Orthopedic Society for Sports Medicine. 32 (5): 1173–1181. doi:10.1177/0363546503262159. PMID 15262639. S2CID 28512769.
- Kraeutler MJ, Bravman JT, McCarty EC (2013). "Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients". Am J Sports Med. 41 (10): 2439–48. doi:10.1177/0363546513484127. PMID 23585484. S2CID 7445341.
- Marrale J, Morrissey MC, Haddad FS (June 2007). "A literature review of autograft and allograft anterior cruciate ligament reconstruction". Knee Surg Sports Traumatol Arthrosc. 15 (6): 690–704. doi:10.1007/s00167-006-0236-1. PMID 17429611. S2CID 12469855.
- Shelbourne KD, Vanadurongwan B, Gray T (October 2007). "Primary anterior cruciate ligament reconstruction using contralateral patellar tendon autograft". Clin Sports Med. 26 (4): 549–65. doi:10.1016/j.csm.2007.06.008. PMID 17920952.
- Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348-359. doi:10.1177/0363546510383481.
- Li X, Orvets N. Arthroscopic acl reconstruction with bone patellar bone graft using anteromedial technique. J Med Ins. 2016;2016(45). doi:https://doi.org/10.24296/jomi/45]
- O'Brien, DF; Kraeutler MJ; Koyonos L; Flato RR; Ciccotti MG; Cohen SB (2014). "Allograft anterior cruciate ligament reconstruction in patients younger than 30 years: A matched-pair comparison of bone-patellar tendon-bone and tibialis anterior". Am J Orthop. 43 (3): 132–136. PMID 24660179.
- "ACL Program - Bridge-Enhanced ACL Repair (BEAR) Clinical Trial". www.childrenshospital.org. Archived from the original on 20 May 2017. Retrieved 25 April 2016.
- Murray, Martha M.; Kalish, Leslie A.; Fleming, Braden C.; Flutie, Brett; Freiberger, Christina; Henderson, Rachael N.; Perrone, Gabriel S.; Thurber, Laura G.; Proffen, Benedikt L.; Ecklund, Kirsten; Kramer, Dennis E. (2019-03-22). "Bridge-Enhanced Anterior Cruciate Ligament Repair: Two-Year Results of a First-in-Human Study". Orthopaedic Journal of Sports Medicine. 7 (3): 232596711882435. doi:10.1177/2325967118824356. ISSN 2325-9671. PMC 6431773. PMID 30923725.
- "A Comparison of ACL Repair With BEAR Device vs. Autograft Patellar Tendon ACL Reconstruction - Full Text View - ClinicalTrials.gov". clinicaltrials.gov. Retrieved 2019-10-22.
- Coutu, DL; et al. (August 2007). "Hierarchical scaffold design for mesenchymal stem cell-based gene therapy of hemophilia B." Current Opinion in Chemical Biology. 11 (4): 394–8. doi:10.1016/j.cbpa.2007.05.034. PMC 2038982. PMID 17656148.
- Farrell E, O'Brien FJ, Doyle P, Fischer J, Yannas I, Harley BA, O'Connell B, Prendergast PJ, Campbell VA, et al. (March 2006). "A collagen-glycosaminoglycan scaffold supports adult rat mesenchymal stem cell differentiation along osteogenic and chondrogenic routes". Tissue Engineering. 12 (3): 459–68. doi:10.1089/ten.2006.12.459. PMID 16579679.
- E.W. Yates; A. Rupani; G.T. Foley; W.S. Khan; S. Cartmell; S.J. Anand (2012). "Ligament Tissue Engineering and Its Potential Role in Anterior Cruciate Ligament Reconstruction". Stem Cells International. 2012: 6. doi:10.1155/2012/438125. PMC 3255293. PMID 22253633.
- Arundale AH, Cummer K, Capin JJ, Zarzycki R, Snyder-Mackler L (October 2017). "Report of the Clinical and Functional Primary Outcomes in Men of the ACL-SPORTS Trial: Similar Outcomes in Men Receiving Secondary Prevention With and Without Perturbation Training 1 and 2 Years After ACL Reconstruction". Clin. Orthop. Relat. Res. 475 (10): 2523–2534. doi:10.1007/s11999-017-5280-2. PMC 5599384. PMID 28224443.
- Capin JJ, Zarzycki R, Arundale A, Cummer K, Snyder-Mackler L (October 2017). "Report of the Primary Outcomes for Gait Mechanics in Men of the ACL-SPORTS Trial: Secondary Prevention With and Without Perturbation Training Does Not Restore Gait Symmetry in Men 1 or 2 Years After ACL Reconstruction". Clin. Orthop. Relat. Res. 475 (10): 2513–2522. doi:10.1007/s11999-017-5279-8. PMC 5599383. PMID 28224442.
- "Anterior Cruciate Ligament (ACL) Injuries - Topic Overview". www.webmd.com. Retrieved 25 April 2016.
- Sonnery-Cottet, Bertrand; Saithna, Adnan; Quelard, Benedicte; Daggett, Matt; Borade, Amrut; Ouanezar, Hervé; Thaunat, Mathieu; Blakeney, William G (March 2019). "Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions". British Journal of Sports Medicine. 53 (5): 289–298. doi:10.1136/bjsports-2017-098401. ISSN 0306-3674. PMC 6579490. PMID 30194224.
- Delaloye, Jean-Romain; Murar, Jozef; Sánchez, Mauricio González; Saithna, Adnan; Ouanezar, Hervé; Thaunat, Mathieu; Vieira, Thais Dutra; Sonnery-Cottet, Bertrand (June 2018). "How to Rapidly Abolish Knee Extension Deficit After Injury or Surgery: A Practice-Changing Video Pearl From the Scientific Anterior Cruciate Ligament Network International (SANTI) Study Group". Arthroscopy Techniques. 7 (6): e601–e605. doi:10.1016/j.eats.2018.02.006. PMC 6019855. PMID 30013901.
- Vanvuren, Christina (2016-11-29). "How much does ACL surgery cost?". Amino Blog: Telling Health Care Stories with Data. Retrieved 2017-05-15.
- Bonsell, Shawn (2017-05-15). "Financial analysis of anterior cruciate ligament reconstruction at Baylor University Medical Center". Proceedings (Baylor University. Medical Center). 13 (4): 327–330. doi:10.1080/08998280.2000.11927697. ISSN 0899-8280. PMC 1312224. PMID 16389334.
- Lewis, Sarah (2016-10-17). "How Much Does ACL Surgery Cost?". Healthgrades Operating Company, Inc. Retrieved 2017-05-15.
- "Anterior Cruciate Ligament (ACL) Surgery". WebMD. Retrieved 25 April 2016.