Common bile duct
The common bile duct, sometimes abbreviated CBD,[2] is a duct in the gastrointestinal tract of organisms that have a gallbladder. It is formed by the union of the common hepatic duct and the cystic duct (from the gallbladder). It is later joined by the pancreatic duct to form the ampulla of Vater. There, the two ducts are surrounded by the muscular sphincter of Oddi.
| Common bile duct | |
|---|---|
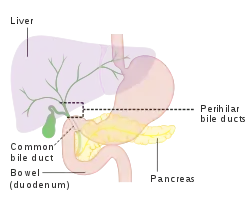 Diagram of the biliary tree showing the common bile duct | |
| Details | |
| Part of | Biliary tract |
| Identifiers | |
| Latin | ductus choledochus |
| Acronym(s) | CBD |
| MeSH | D003135 |
| TA98 | A05.8.02.013 |
| TA2 | 3103 |
| FMA | 14667 |
| Anatomical terminology | |
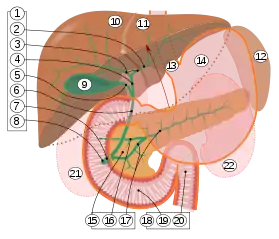
9. Gallbladder, 10–11. Right and left lobes of liver. 12. Spleen.
13. Esophagus. 14. Stomach. 15. Pancreas: 16. Accessory pancreatic duct, 17. Pancreatic duct.
18. Small intestine: 19. Duodenum, 20. Jejunum
21–22. Right and left kidneys.
The front border of the liver has been lifted up (brown arrow).[1]
When the sphincter of Oddi is closed, newly synthesized bile from the liver is forced into storage in the gallbladder. When open, the stored and concentrated bile exits into the duodenum. This conduction of bile is the main function of the common bile duct. The hormone cholecystokinin, when stimulated by a fatty meal, promotes bile secretion by increased production of hepatic bile, contraction of the gallbladder, and relaxation of the sphincter of Oddi.
Clinical significance
Several problems can arise within the common bile duct. A diameter of more than 8 mm is regarded as abnormal dilatation and is a sign of cholestasis.[3]
| Normal | ≤ 8 mm |
| Mild dilatation | 8 – 12 mm |
| Moderate dilatation | 12 – 16 mm |
| Severe dilatation | 16 – 20 mm |
| Extremely severe dilatation | >20 mm |
It normally gets slightly dilated after cholecystectomy, with upper limit (95% prediction interval) being about 10 mm after a few months.[5]
On abdominal ultrasonography, the common bile duct is generally seen most readily in the perihilar area (the border area between the common hepatic duct and the CBD, by the hilum of the liver). The absence of Doppler signal distinguishes it from the portal vein and hepatic artery.
 Borderline of a dilated perihilar bile duct, measuring 8 mm.
Borderline of a dilated perihilar bile duct, measuring 8 mm. Dilatation of CBD due to Ampullary tumor.
Dilatation of CBD due to Ampullary tumor.
If clogged by a gallstone, a condition called choledocholithiasis can result.[6] In this clogged state, the duct is especially vulnerable to an infection called ascending cholangitis. One form of treatment is a cholecystenterostomy. Very rare deformities of the common bile duct are cystic dilations (4 cm), choledochoceles (cystic dilation of the ampula of Vater (3–8 cm)), and biliary atresia.
History
Blockage of the common bile duct and related jaundice has been documented since at least since the time of Erasistratus.[7]
Additional images
 The gall-bladder and bile ducts laid open.
The gall-bladder and bile ducts laid open.
References
- Standring S, Borley NR, eds. (2008). Gray's anatomy : the anatomical basis of clinical practice. Brown JL, Moore LA (40th ed.). London: Churchill Livingstone. pp. 1163, 1177, 1185–6. ISBN 978-0-8089-2371-8.
- Agabegi, Steven S.; Agabegi, Elizabeth D. (23 August 2012). Step-Up to Medicine. Lippincott Williams & Wilkins. p. 136. ISBN 9781609133603.
- Hoeffel, Christine; Azizi, Louisa; Lewin, Maité; Laurent, Valérie; Aubé, Christophe; Arrivé, Lionel; Tubiana, Jean-Michel (2006). "Normal and Pathologic Features of the Postoperative Biliary Tract at 3D MR Cholangiopancreatography and MR Imaging". RadioGraphics. 26 (6): 1603–1620. doi:10.1148/rg.266055730. ISSN 0271-5333. PMID 17102039.
- Yunfu Lv, Wan Yee Lau, Haiying Wu, Shunwu Chang, NingLiu, Yejuan Li, Jie Deng (2015). "Etiological Causes of Intrahepatic and Extrahepatic Bile Duct Dilatation" (PDF). International Journal of New Technology and Research (IJNTR). 1 (8).CS1 maint: multiple names: authors list (link)
- Feng, B; Song, Q (1995). "Does the common bile duct dilate after cholecystectomy? Sonographic evaluation in 234 patients". American Journal of Roentgenology. 165 (4): 859–861. doi:10.2214/ajr.165.4.7676981. ISSN 0361-803X. PMID 7676981.
- Humes, H. David (2001). Kelley's Essentials of Internal Medicine. Lippincott Williams & Wilkins. p. 229. ISBN 978-0781719377.
- Bateson, edited by Malcolm C. (1986). Gallstone Disease and its Management. Dordrecht: Springer Netherlands. p. Epidemiology (chapter). ISBN 9400941730.CS1 maint: extra text: authors list (link)
- Miederer, S.; Lindstaedt, H.; Siedek, M.; Franken, Th. (1978). "Endoskopische transpapilläre Spaltung einer Choledochocele" [Endoscopic transpapillary Splitting of a choledochocele]. Deutsche Medizinische Wochenschrift (in German). 103 (5): 216–219. doi:10.1055/s-0028-1104409. PMID 631041.
External links
- Anatomy figure: 38:06-08 at Human Anatomy Online, SUNY Downstate Medical Center - "The gallbladder and extrahepatic bile ducts."
- Anatomy image:8336 at the SUNY Downstate Medical Center
- Anatomy image:7957 at the SUNY Downstate Medical Center
- liver at The Anatomy Lesson by Wesley Norman (Georgetown University) (biliarysystem)