Corticotropic cell
Corticotropes (or corticotrophs) are basophilic cells in the anterior pituitary that produce pro-opiomelanocortin (POMC) which undergoes cleavage to adrenocorticotropin (ACTH), β-lipotropin (β-LPH), and melanocyte-stimulating hormone (MSH).[1] These cells are stimulated by corticotropin releasing hormone (CRH) and make up 15–20% of the cells in the anterior pituitary.[2] The release of ACTH from the corticotropic cells is controlled by CRH, which is formed in the cell bodies of parvocellular neurosecretory cells within the paraventricular nucleus of the hypothalamus and passes to the corticotropes in the anterior pituitary via the hypophyseal portal system. Adrenocorticotropin hormone stimulates the adrenal cortex to release glucocorticoids and plays an important role in the stress response.[3]
| Corticotropic cell | |
|---|---|
| Details | |
| Location | Anterior pituitary |
| Function | Production of melanocyte-stimulating hormone, adrenocorticotropic hormone (ACTH) and lipotropin |
| Identifiers | |
| TH | H3.08.02.2.00009 |
| Anatomical terms of microanatomy | |
Function
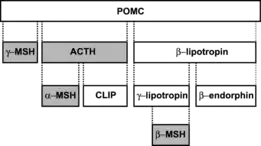
The primary function of the corticotropic cells is to produce the prohormone POMC in response to the release of CRH from the hypothalamus. POMC is cleaved into several peptide hormones via enzyme activity. In addition to synthesis in the corticotropes, POMC is also synthesized in melanotroph cells, the arcuate nucleus of the hypothalamus, and melanocytes.[4] POMC undergoes differential cleavage into various peptide hormones depending on the cell it is synthesized in; it also varies based on species. POMC in the corticotropes of humans is proteolytically cleaved by proprotein convertases into ACTH and β-lipotropin.[5] In rats, however, the ACTH is further cleaved into α-MSH and CLIP in the corticotrope.[4] These peptide hormones are stored within vesicles in the corticotropic cells and are released in response to CRH stimulation from the hypothalamus. These vesicles then leave the anterior pituitary and travel throughout the body via the bloodstream to reach their target tissues.[6]
| Hormone(s) | Main Targets | Effects |
|---|---|---|
| ACTH | Adrenal cortex | Glucocorticoid synthesis |
| α-MSH, β-MSH, γ-MSH | Skin Cells (Melanocytes), Brain, Exocrine Glands | Pigmentation of hair and skin, satiety, weight homeostasis[6] |
| CLIP | Pancreas | Insulin secretagogue, stimulates insulin release[7] |
| β-lipotropin, γ-lipotropin | Adipose Tissue | Lipolysis, fatty acid mobilization[8] |
| β-endorphin | Peripheral Nervous System | Pain management[9] |
Role in the Hypothalamic–pituitary–adrenal Axis
Stimulation
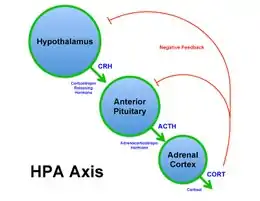
Corticotropic cells serve an important role within the feedback loop of the hypothalamic–pituitary–adrenal (HPA) axis and the stress response. Corticotropes produce and release ACTH, a 39 amino acid peptide hormone, in response to corticotropic releasing hormone (CRH) release from the hypothalamus. CRH is a 41-amino-acid peptide hormone that is secreted by the parvocellular neurosecretory cells, which are found within the paraventricular nucleus of the hypothalamus.[10]
Stimuli for the release of CRH from the hypothalamus include:
- Forskolin[11]
- Interleukin-6[11]
- Pituitary adenylate cyclase-activating peptide (PACAP)[11]
- Stress or trauma
- Circadian rhythms[6]
Forskolin and PACAP regulate the synthesis of CRH in the hypothalamus by binding to G protein-coupled receptors and stimulating and increase in cAMP within the cells via the action of adenylate cyclase. This activates the protein kinase A pathway, which results in the binding of cAMP response element binding protein (CREB) onto the CRH promoter region and induces transcription of CRH. This process is repressed by glucocorticoids; this inhibitory feedback helps maintain homeostasis of the stress response.[11]
Once released by the hypothalamus, CRH travels through the hypophyseal portal system to the anterior pituitary, where it binds to G protein-coupled receptors on the corticotropic cell membrane and stimulates cAMP production. The effects of CRH on pituitary corticotropes are potentiated by vasopressin (AVP); AVP is a weak inducer of ACTH production on its own, but has a strong synergistic effect on ACTH production when CRH is also bound to the receptor.[12] These signaling hormones act via signal transduction, causing the synthesis of POMC and eventual cleavage to ACTH and β-lipotropin. These peptide hormones are then released into the bloodstream, where they circulate and act on target tissues.
Function
ACTH released from the corticotropes binds to G protein-coupled receptors in the adrenal cortex, where it stimulates the production of glucocorticoids (primarily cortisol).[13] ACTH binds to the melanocortin 2 receptor and, through signal transduction, increases levels of cholesterol esterase, the transport of cholesterol across the mitochondrial membrane, cholesterol binding to P450SCC and, an increase in pregnenolone synthesis.[6] It also serves as a secondary stimulus for the synthesis of mineralocorticoids such as aldosterone, which serve an important role in regulating the salt balance of the blood.[14] Glucocorticoids released by the adrenal cortex inhibit production of CRH and ACTH, forming a negative feedback loop.[6]
Inhibition of ACTH production
Corticotropes contain glucocorticoid receptors (GRs) and corticosteroid-binding globulin (CBG, or transcortin). GR is a nuclear receptor that inhibits transcription of ACTH via a negative glucocorticoid recognition element (GRE) that binds cortisol on POMC DNA, but generally transcortin binds glucocorticoids (including cortisol, cortisone, deoxycortisone, and aldosterone) with high affinity and prevents this inhibition.[15] Tonic inhibition of corticotropes requires high concentrations of glucocorticoids, exceeding CBG capacity. This causes ACTH secretion to be vulnerable to inhibition in patients taking glucocorticoids for medical purposes such as treatment of autoimmune disease or as an anti-transplant-rejection medication.[16]
Associated diseases
Cushing's Disease
Corticotropic cells can have detrimental effects on the body if they express too much or too little ACTH. One such example is Cushing's disease, which can result from overproduction of ACTH in the corticotropes due to pituitary tumors known as corticotroph adenomas; this is the cause for roughly two-thirds of those diagnosed with Cushing's disease.[17] It is also possible that this disease can result from production of ACTH in a non-pituitary tumor, known as ectopic production, or the adrenal glands can overproduce cortisol due to an adrenal tumor.[18] This overproduction of ACTH causes an increase in cortisol levels due to increased glucocorticoid synthesis in the adrenal cortex resulting in several associated symptoms.
Symptoms of Cushing's disease include:
- Fatty deposits in the neck or back
- Stretch marks (striae)[19]
- Fatigue[19]
- Osteoporosis[19]
- Weakened immune system[19]
- Hypertension[19]
Addison's Disease
Corticotropic cells can also be the cause of Addison's disease in some instances. Addison's disease is characterized adrenal insufficiency, which is defined as the underproduction of glucocorticoids by the adrenal cortex. If the corticotropes underproduce ACTH this can result in secondary adrenal insufficiency, causing the adrenal glands to underproduce cortisol. This can be caused by tumors of the anterior pituitary or hypothalamus, inflammation, or surgery.[20] This ultimately results in the underproduction of cortisol, which has many detrimental symptoms.
Symptoms of Addison's disease include:
- Weight loss[21]
- Hypoglycemia[21]
- Hypotension[21]
- Irritability[21]
See also
References
- "Endocrine System - The Pituitary". science.jrank.org.
- Yeung CM, Chan CB, Leung PS, Cheng CH (2006). "Cells of the anterior pituitary". The International Journal of Biochemistry & Cell Biology. 38 (9): 1441–9. doi:10.1016/j.biocel.2006.02.012. PMID 16621669.
- Cole LA, Kramer PR (2016). Human physiology, biochemistry and basic medicine. Amsterdam. pp. 69–77. ISBN 9780128037171. OCLC 924207881.
- Rousseau K, Kauser S, Pritchard LE, Warhurst A, Oliver RL, Slominski A, Wei ET, Thody AJ, Tobin DJ, White A (June 2007). "Proopiomelanocortin (POMC), the ACTH/melanocortin precursor, is secreted by human epidermal keratinocytes and melanocytes and stimulates melanogenesis". FASEB Journal. 21 (8): 1844–56. doi:10.1096/fj.06-7398com. PMC 2253185. PMID 17317724.
- Day R, Squire L (2009). Encyclopedia of Neuroscience. Amsterdam: Elsevier. pp. 1139–1141. ISBN 978-0080450469. OCLC 237029015.
- Nussey SS, Whitehead SA (2001-06-15). Endocrinology. CRC Press. doi:10.1201/b15306. ISBN 9780429205958.
- Marshall JB, Kapcala LP, Manning LD, McCullough AJ (November 1984). "Effect of corticotropin-like intermediate lobe peptide on pancreatic exocrine function in isolated rat pancreatic lobules". The Journal of Clinical Investigation. 74 (5): 1886–9. doi:10.1172/JCI111608. PMC 425369. PMID 6209301.
- Blanco G, Blanco A (2017). Medical biochemistry. London, United Kingdom. pp. 573–644. ISBN 9780128035870. OCLC 985609626.
- Sprouse-Blum AS, Smith G, Sugai D, Parsa FD (March 2010). "Understanding endorphins and their importance in pain management". Hawaii Medical Journal. 69 (3): 70–1. PMC 3104618. PMID 20397507.
- Takahashi A (2016). "Adrenocorticotropic Hormone". Handbook of Hormones. Elsevier. pp. 118–e16A–2. doi:10.1016/B978-0-12-801028-0.00135-5. ISBN 9780128010280.
- Kageyama K, Suda T (2010-07-07). Vitamins and Hormones. London. pp. 301–317. ISBN 9780123815323. OCLC 688618093.
- Salata RA, Jarrett DB, Verbalis JG, Robinson AG (March 1988). "Vasopressin stimulation of adrenocorticotropin hormone (ACTH) in humans. In vivo bioassay of corticotropin-releasing factor (CRF) which provides evidence for CRF mediation of the diurnal rhythm of ACTH". The Journal of Clinical Investigation. 81 (3): 766–74. doi:10.1172/JCI113382. PMC 442524. PMID 2830315.
- Soto-Rivera CL, Majzoub JA (2017), "Adrenocorticotrophin", The Pituitary, Elsevier, pp. 47–83, doi:10.1016/B978-0-12-804169-7.00003-9, ISBN 9780128041697
- Arai K, Chrousos GP (January 1995). "Syndromes of glucocorticoid and mineralocorticoid resistance". Steroids. 60 (1): 173–9. doi:10.1016/0039-128x(94)00007-y. PMID 7792808. S2CID 45225758.
- Bittar E, Bittar N (1997). Molecular and cellular endocrinology. Greenwich, Conn.: JAI Press. ISBN 9781559388153. OCLC 162130720.
- Pecoraro N, Dallman MF (2009). "Hypothalamic–Pituitary–Adrenal (HPA) Axis". Encyclopedia of Neuroscience. Elsevier. pp. 65–74. doi:10.1016/b978-008045046-9.00474-5. ISBN 9780080450469.
- Tanase CP, Ogrezeanu I, Badiu C (2012), "Pituitary Tumor Classification", Molecular Pathology of Pituitary Adenomas, Elsevier, pp. 1–18, doi:10.1016/b978-0-12-415830-6.00001-9, ISBN 9780124158306
- Bertagna X, Guignat L, Groussin L, Bertherat J (October 2009). "Cushing's disease". Best Practice & Research. Clinical Endocrinology & Metabolism. 23 (5): 607–23. doi:10.1016/j.beem.2009.06.001. PMID 19945026.
- Barthel A, Willenberg HS, Gruber M, Bornstein SR (2016). Adrenal Insufficiency. Endocrinology: Adult and Pediatric. Elsevier. pp. 1763–1774.e4. doi:10.1016/b978-0-323-18907-1.00102-5. ISBN 9780323189071.
- Barthel A, Willenberg HS, Gruber M, Bornstei SR (2016). Adrenal Insufficiency. Endocrinology: Adult and Pediatric. Elsevier. pp. 1763–1774.e4. doi:10.1016/b978-0-323-18907-1.00102-5. ISBN 9780323189071.
- Levy MJ, Howlett TA (2014), "Hypothalamic, pituitary and adrenal disorders", Clinical Biochemistry: Metabolic and Clinical Aspects, Elsevier, pp. 349–372, doi:10.1016/b978-0-7020-5140-1.00018-3, ISBN 9780702051401