Human body temperature
Normal human body-temperature (normothermia, euthermia) is the typical temperature range found in humans. The normal human body temperature range is typically stated as 36.5–37.5 °C (97.7–99.5 °F).[8]
| Temperature classification | ||||||||||||
|
||||||||||||
| Note: The difference between fever and hyperthermia is the underlying mechanism. Different sources have different cut-offs for fever, hyperthermia and hyperpyrexia. | ||||||||||||
Human body temperature varies. It depends on gender, age, time of day, exertion level, health status (such as illness and menstruation), what part of the body the measurement is taken at, state of consciousness (waking, sleeping, sedated), and emotions. Body temperature is kept in normal range by thermoregulation, in which adjustment of temperature is triggered by the central nervous system.
Methods of measurement
Taking a person's temperature is an initial part of a full clinical examination. There are various types of medical thermometers, as well as sites used for measurement, including:
- In the rectum (rectal temperature)
- In the mouth (oral temperature)
- Under the arm (axillary temperature)
- In the ear (tympanic temperature)
- On the skin of the forehead over the temporal artery
- Using heat flux sensors
Variations
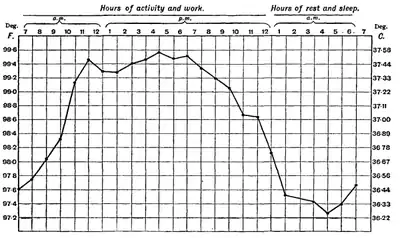
Temperature control (thermoregulation) is part of a homeostatic mechanism that keeps the organism at optimum operating temperature, as the temperature affects the rate of chemical reactions. In humans, the average internal temperature is 37.0 °C (98.6 °F), though it varies around this point by 0.5 to 1 C.[9] However, no person always has exactly the same temperature at every moment of the day. Temperatures cycle regularly up and down through the day, as controlled by the person's circadian rhythm. The lowest temperature occurs about two hours before the person normally wakes up. Additionally, temperatures change according to activities and external factors.[10]
In addition to varying throughout the day, normal body temperature may also differ as much as 0.5 °C (0.9 °F) from one day to the next, so that the highest or lowest temperatures on one day will not always exactly match the highest or lowest temperatures on the next day.
Normal human body temperature varies slightly from person to person and by the time of day. Consequently, each type of measurement has a range of normal temperatures. The range for normal human body temperatures, taken orally, is 36.8±0.5 °C (98.2±0.9 °F).[11] This means that any oral temperature between 36.3 and 37.3 °C (97.3 and 99.1 °F) is likely to be normal.
The normal human body temperature is often stated as 36.5–37.5 °C (97.7–99.5 °F).[8] In adults a review of the literature has found a wider range of 33.2–38.2 °C (91.8–100.8 °F) for normal temperatures, depending on the gender and location measured.[12]
Reported values vary depending on how it is measured: oral (under the tongue): 36.8±0.4 °C (98.2±0.72 °F),[13] internal (rectal, vaginal): 37.0 °C (98.6 °F).[13] A rectal or vaginal measurement taken directly inside the body cavity is typically slightly higher than oral measurement, and oral measurement is somewhat higher than skin measurement. Other places, such as under the arm or in the ear, produce different typical temperatures.[13] While some people think of these averages as representing normal or ideal measurements, a wide range of temperatures has been found in healthy people.[5] The body temperature of a healthy person varies during the day by about 0.5 °C (0.9 °F) with lower temperatures in the morning and higher temperatures in the late afternoon and evening, as the body's needs and activities change.[13] Other circumstances also affect the body's temperature. The core body temperature of an individual tends to have the lowest value in the second half of the sleep cycle; the lowest point, called the nadir, is one of the primary markers for circadian rhythms. The body temperature also changes when a person is hungry, sleepy, sick, or cold.
Natural rhythms
Body temperature normally fluctuates over the day following circadian rhythms, with the lowest levels around 4 a.m. and the highest in the late afternoon, between 4:00 and 6:00 p.m. (assuming the person sleeps at night and stays awake during the day).[11][13] Therefore, an oral temperature of 37.3 °C (99.1 °F) would, strictly speaking, be a normal, healthy temperature in the afternoon but not in the early morning.[13] An individual's body temperature typically changes by about 0.5 °C (0.9 °F) between its highest and lowest points each day.[13]
Body temperature is sensitive to many hormones, so women have a temperature rhythm that varies with the menstrual cycle, called a circamensal rhythm.[10] A woman's basal body temperature rises sharply after ovulation, as estrogen production decreases and progesterone increases. Fertility awareness programs use this change to identify when a woman has ovulated in order to achieve or avoid pregnancy. During the luteal phase of the menstrual cycle, both the lowest and the average temperatures are slightly higher than during other parts of the cycle. However, the amount that the temperature rises during each day is slightly lower than typical, so the highest temperature of the day is not very much higher than usual.[14] Hormonal contraceptives both suppress the circamensal rhythm and raise the typical body temperature by about 0.6 °C (1.1 °F).[10]
Temperature also varies with the change of seasons during each year. This pattern is called a circannual rhythm.[14] Studies of seasonal variations have produced inconsistent results. People living in different climates may have different seasonal patterns.
Increased physical fitness increases the amount of daily variation in temperature.[14]
With increased age, both average body temperature and the amount of daily variability in the body temperature tend to decrease.[14] Elderly patients may have a decreased ability to generate body heat during a fever, so even a somewhat elevated temperature can indicate a serious underlying cause in geriatrics. One study suggested that the average body temperature has also decreased since the 1850s.[15] The study's authors believe the most likely explanation for the change is a reduction in inflammation at the population level due to decreased chronic infections and improved hygiene.[16]
Measurement methods
| Method | Women | Men |
|---|---|---|
| Oral | 33.2–38.1 °C (91.8–100.6 °F) | 35.7–37.7 °C (96.3–99.9 °F) |
| Rectal | 36.8–37.1 °C (98.2–98.8 °F) | 36.7–37.5 °C (98.1–99.5 °F) |
| Tympanic | 35.7–37.8 °C (96.3–100.0 °F) | 35.5–37.8 °C (95.9–100.0 °F) |
Different methods used for measuring temperature produce different results. The temperature reading depends on which part of the body is being measured. The typical daytime temperatures among healthy adults are as follows:
- Temperature in the anus (rectum/rectal), vagina, or in the ear (tympanic) is about 37.5 °C (99.5 °F)[18]
- Temperature in the mouth (oral) is about 36.8 °C (98.2 °F)[11]
- Temperature under the arm (axillary) is about 36.5 °C (97.7 °F)[18]
Generally, oral, rectal, gut, and core body temperatures, although slightly different, are well-correlated.
Oral temperatures are influenced by drinking, chewing, smoking, and breathing with the mouth open. Mouth breathing, cold drinks or food, reduce oral temperatures; hot drinks, hot food, chewing, and smoking raise oral temperatures.[10]
Each measurement method also has different normal ranges depending on sex.[17]
Infrared thermometer
As of 2016 reviews of infrared thermometers have found them to be of variable accuracy.[19] This includes tympanic infrared thermometers in children.[20]
Variations due to outside factors
Many outside factors affect the measured temperature as well. "Normal" values are generally given for an otherwise healthy, non-fasting adult, dressed comfortably, indoors, in a room that is kept at a normal room temperature, 22.7 to 24.4 °C (73 to 76 °F), during the morning, but not shortly after arising from sleep. Furthermore, for oral temperatures, the subject must not have eaten, drunk, or smoked anything in at least the previous fifteen to twenty minutes, as the temperature of the food, drink, or smoke can dramatically affect the reading.
Temperature is increased after eating or drinking anything with calories. Caloric restriction, as for a weight-loss diet, decreases overall body temperature.[10] Drinking alcohol decreases the amount of daily change, slightly lowering daytime temperatures and noticeably raising nighttime temperatures.[10]
Exercise raises body temperatures. In adults, a noticeable increase usually requires strenuous exercise or exercise sustained over a significant time. Children develop higher temperatures with milder activities, like playing.
Psychological factors also influence body temperature: a very excited person often has an elevated temperature.
Wearing more clothing slows daily temperature change and raises body temperature.[10] Similarly, sleeping with an electric blanket raises the body temperature at night.[10]
Sleep disturbances also affect temperatures. Normally, body temperature drops significantly at a person's normal bedtime and throughout the night. Short-term sleep deprivation produces a higher temperature at night than normal, but long-term sleep deprivation appears to reduce temperatures.[10] Insomnia and poor sleep quality are associated with smaller and later drops in body temperature.[10] Similarly, waking up unusually early, sleeping in, jet lag and changes to shift work schedules may affect body temperature.[10]
Concept
Fever
A temperature setpoint is the level at which the body attempts to maintain its temperature. When the setpoint is raised, the result is a fever. Most fevers are caused by infectious disease and can be lowered, if desired, with antipyretic medications.
An early morning temperature higher than 37.2 °C (99.0 °F) or a late afternoon temperature higher than 37.7 °C (99.9 °F) is normally considered a fever, assuming that the temperature is elevated due to a change in the hypothalamus's setpoint.[13] Lower thresholds are sometimes appropriate for elderly people.[13] The normal daily temperature variation is typically 0.5 °C (0.90 °F), but can be greater among people recovering from a fever.[13]
An organism at optimum temperature is considered afebrile or apyrexic, meaning "without fever". If temperature is raised, but the setpoint is not raised, then the result is hyperthermia.
Hyperthermia
Hyperthermia occurs when the body produces or absorbs more heat than it can dissipate. It is usually caused by prolonged exposure to high temperatures. The heat-regulating mechanisms of the body eventually become overwhelmed and unable to deal effectively with the heat, causing the body temperature to climb uncontrollably. Hyperthermia at or above about 40 °C (104 °F) is a life-threatening medical emergency that requires immediate treatment. Common symptoms include headache, confusion, and fatigue. If sweating has resulted in dehydration, then the affected person may have dry, red skin.
In a medical setting, mild hyperthermia is commonly called heat exhaustion or heat prostration; severe hyperthermia is called heat stroke. Heat stroke may come on suddenly, but it usually follows the untreated milder stages. Treatment involves cooling and rehydrating the body; fever-reducing drugs are useless for this condition. This may be done through moving out of direct sunlight to a cooler and shaded environment, drinking water, removing clothing that might keep heat close to the body, or sitting in front of a fan. Bathing in tepid or cool water, or even just washing the face and other exposed areas of the skin, can be helpful.
With fever, the body's core temperature rises to a higher temperature through the action of the part of the brain that controls the body temperature; with hyperthermia, the body temperature is raised without the influence of the heat control centers.
Hypothermia
In hypothermia, body temperature drops below that required for normal metabolism and bodily functions. In humans, this is usually due to excessive exposure to cold air or water, but it can be deliberately induced as a medical treatment. Symptoms usually appear when the body's core temperature drops by 1–2 °C (1.8–3.6 °F) below normal temperature.
Basal body temperature
Basal body temperature is the lowest temperature attained by the body during rest (usually during sleep). It is generally measured immediately after awakening and before any physical activity has been undertaken, although the temperature measured at that time is somewhat higher than the true basal body temperature. In women, temperature differs at various points in the menstrual cycle, and this can be used in the long term to track ovulation both for the purpose of aiding conception or avoiding pregnancy. This process is called fertility awareness.
Core temperature
Core temperature, also called core body temperature, is the operating temperature of an organism, specifically in deep structures of the body such as the liver, in comparison to temperatures of peripheral tissues. Core temperature is normally maintained within a narrow range so that essential enzymatic reactions can occur. Significant core temperature elevation (hyperthermia) or depression (hypothermia) over more than a brief period of time is incompatible with human life.
Temperature examination in the heart, by means of a catheter, is the traditional gold standard measurement used to estimate core temperature (oral temperature is affected by hot or cold drinks, ambient temperature fluctuations as well as mouth-breathing). Since catheters are highly invasive, the generally accepted alternative for measuring core body temperature is through rectal measurements. Rectal temperature is expected to be approximately 1 Fahrenheit (or 0.55 Celsius) degree higher than an oral temperature taken on the same person at the same time. Ear thermometers measure eardrum temperature from the tympanic membrane using infrared sensors and also aim to measure core body temperature, since the blood supply of this membrane is directly shared with the brain. However, this method of measuring body temperature is not as accurate as rectal measurement and has a low sensitivity for fever, failing to determine three or four out of every ten fever measurements in children.[21] Ear temperature measurement may be acceptable for observing trends in body temperature but is less useful in consistently identifying and diagnosing fever.
Until recently, direct measurement of core body temperature required either an ingestible device or surgical insertion of a probe. Therefore, a variety of indirect methods have commonly been used as the preferred alternative to these more accurate albeit more invasive methods. The rectal or vaginal temperature is generally considered to give the most accurate assessment of core body temperature, particularly in hypothermia. In the early 2000s, ingestible thermistors in capsule form were produced, allowing the temperature inside the digestive tract to be transmitted to an external receiver; one study found that these were comparable in accuracy to rectal temperature measurement.[22] More recently, a new method using heat flux sensors have been developed. Several research papers show that its accuracy is similar to the invasive methods.[23][24][25]
Temperature variation
Hot
- 44 °C (111.2 °F) or more – Almost certainly death will occur; however, people have been known to survive up to 46.5 °C (115.7 °F).[26][27]
- 43 °C (109.4 °F) – Normally death, or there may be serious brain damage, continuous convulsions and shock. Cardio-respiratory collapse will likely occur.
- 42 °C (107.6 °F) – Subject may turn pale or remain flushed and red. They may become comatose, be in severe delirium, vomiting, and convulsions can occur. Blood pressure may be high or low and heart rate will be very fast.
- 41 °C (105.8 °F) – (Medical emergency) – Fainting, vomiting, severe headache, dizziness, confusion, hallucinations, delirium and drowsiness can occur. There may also be palpitations and breathlessness.
- 40 °C (104 °F) – Fainting, dehydration, weakness, vomiting, headache, breathlessness and dizziness may occur as well as profuse sweating. Starts to be life-threatening.
- 39 °C (102.2 °F) – Severe sweating, flushed and red. Fast heart rate and breathlessness. There may be exhaustion accompanying this. Children and people with epilepsy may be very likely to get convulsions at this point.
- 38 °C (100.4 °F) – (Classed as hyperthermia if not caused by a fever) – Feeling hot, sweating, feeling thirsty, feeling very uncomfortable, slightly hungry. If this is caused by fever, there may also be chills.
Normal
- 36.5–37.5 °C (97.7–99.5 °F) is a typically reported range for normal body temperature.[8]
Cold
- 36 °C (96.8 °F) – Feeling cold, mild to moderate shivering. Body temperature may drop this low during sleep. May be a normal body temperature.
- 35 °C (95 °F) – (Hypothermia is less than 35 °C (95 °F)) – Intense shivering, numbness and bluish/grayness of the skin. There is the possibility of heart irritability.
- 34 °C (93.2 °F) – Severe shivering, loss of movement of fingers, blueness, and confusion. Some behavioral changes may take place.
- 33 °C (91.4 °F) – Moderate to severe confusion, sleepiness, depressed reflexes, progressive loss of shivering, slow heartbeat, shallow breathing. Shivering may stop. Subject may be unresponsive to certain stimuli.
- 32 °C (89.6 °F) – (Medical emergency) – Hallucinations, delirium, complete confusion, extreme sleepiness that is progressively becoming comatose. Shivering is absent (subject may even think they are hot). Reflex may be absent or very slight.
- 31 °C (87.8 °F) – Comatose, very rarely conscious. No or slight reflexes. Very shallow breathing and slow heart rate. Possibility of serious heart rhythm problems.
- 28 °C (82.4 °F) – Severe heart rhythm disturbances are likely and breathing may stop at any time. The person may appear to be dead.
- 24–26 °C (75.2–78.8 °F) or less – Death usually occurs due to irregular heart beat or respiratory arrest; however, some patients have been known to survive with body temperatures as low as 13.7 °C (56.7 °F).[28]
There are non-verbal corporal cues which can hint at an individual experiencing a low body temperature, which can be used for those with dysphasia or for infants.[29] Examples of non-verbal cues of coldness include stillness and being lethargic with regards to kinesiological movement, sneezing, unusual paleness of skin among Caucasians, and, among males, shrinkage, and contraction of the scrotum.[30]
Historical understanding
In the 19th century, most books quoted "blood heat" as 98 °F, until a study published the mean (but not the variance) of a large sample as 36.88 °C (98.38 °F).[31] Subsequently, that mean was widely quoted as "37 °C or 98.4 °F"[32][33] until editors realised 37 °C is equal to 98.6 °F, not 98.4 °F. The 37 °C value was set by German physician Carl Reinhold August Wunderlich in his 1868 book,[34] which put temperature charts into widespread clinical use.[35] Dictionaries and other sources that quoted these averages did add the word "about" to show that there is some variance, but generally did not state how wide the variance is.
References
- Marx J (2006). Rosen's emergency medicine : concepts and clinical practice (6th ed.). Philadelphia: Mosby/Elsevier. p. 2239. ISBN 978-0-323-02845-5. OCLC 58533794.CS1 maint: date and year (link)
- Hutchison JS, Ward RE, Lacroix J, Hébert PC, Barnes MA, Bohn DJ, et al. (June 2008). "Hypothermia therapy after traumatic brain injury in children". The New England Journal of Medicine. 358 (23): 2447–56. doi:10.1056/NEJMoa0706930. PMID 18525042.
- Pryor JA, Prasad AS (2008). Physiotherapy for Respiratory and Cardiac Problems: Adults and Paediatrics. Elsevier Health Sciences. p. 8. ISBN 978-0702039744.
Body temperature is maintained within the range 36.5-37.5 °C. It is lowest in the early morning and highest in the afternoon.
- Axelrod YK, Diringer MN (May 2008). "Temperature management in acute neurologic disorders". Neurologic Clinics. 26 (2): 585–603, xi. doi:10.1016/j.ncl.2008.02.005. PMID 18514828.
- Laupland KB (July 2009). "Fever in the critically ill medical patient". Critical Care Medicine. 37 (7 Suppl): S273-8. doi:10.1097/CCM.0b013e3181aa6117. PMID 19535958.
- Grunau BE, Wiens MO, Brubacher JR (September 2010). "Dantrolene in the treatment of MDMA-related hyperpyrexia: a systematic review". Cjem. 12 (5): 435–42. doi:10.1017/s1481803500012598. PMID 20880437.
Dantrolene may also be associated with improved survival and reduced complications, especially in patients with extreme (≥ 42 °C) or severe (≥ 40 °C) hyperpyrexia
- Sharma HS, ed. (2007). Neurobiology of Hyperthermia (1st ed.). Elsevier. pp. 175–177, 485. ISBN 9780080549996. Retrieved 19 November 2016.
Despite the myriad of complications associated with heat illness, an elevation of core temperature above 41.0 °C (often referred to as fever or hyperpyrexia) is the most widely recognized symptom of this syndrome.
- Hutchison, James S.; et al. (June 2008). "Hypothermia therapy after traumatic brain injury in children". New England Journal of Medicine. 358 (23): 2447–2456. doi:10.1056/NEJMoa0706930. PMID 18525042. S2CID 46833.
We hypothesized that, as compared with normothermia (36.5 to 37.5°C), treatment with hypothermia...
- Britt, L. D.; Barie, Phillip S.; Peitzman, Andrew B.; Jurkovich, Gregory (2012). Acute Care Surgery. Lippincott Williams & Wilkins. p. 707. ISBN 978-1-60831-428-7.
- Kelly, Greg S. (March 2007). "Body temperature variability (Part 2): masking influences of body temperature variability and a review of body temperature variability in disease" (PDF). Alternative Medicine Review. 12 (1): 49–62. PMID 17397267.
- Mackowiak, Philip A.; Wasserman, Steven S.; Levine, Myron M. (1992-09-23). "A critical appraisal of 98.6 degrees F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich". Journal of the American Medical Association. 268 (12): 1578–1580. doi:10.1001/jama.1992.03490120092034. PMID 1302471.
- Sund-Levander, Märtha; Forsberg, Christina; Wahren, Lis Karin (June 2002). "Normal oral, rectal, tympanic and axillary body temperature in adult men and women: a systematic literature review". Scandinavian Journal of Caring Sciences. 16 (2): 122–8. doi:10.1046/j.1471-6712.2002.00069.x. PMID 12000664.
- Longo, Dan L., ed. (2011). Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill. p. 142. ISBN 978-0-07-174889-6. Archived from the original on 2012-04-29. Retrieved 2012-03-16.
- Kelly, Greg S. (December 2006). "Body temperature variability (Part 1): a review of the history of body temperature and its variability due to site selection, biological rhythms, fitness, and aging" (PDF). Alternative Medicine Review. 11 (4): 278–93. PMID 17176167.
- Katz, Brigit (16 January 2020). "Human Body Temperature Is Getting Cooler, Study Finds". Smithsonian. Retrieved 22 January 2020.
- Protsiv, Myroslava; Ley, Catherine; Lankester, Joanna; Hastie, Trevor; Parsonnet, Julie (2020-01-07). Jit, Mark; Franco, Eduardo; Waalen, Jill; Rühli, Frank (eds.). "Decreasing human body temperature in the United States since the Industrial Revolution". eLife. 9: e49555. doi:10.7554/eLife.49555. ISSN 2050-084X. PMC 6946399. PMID 31908267.
- Sund-Levander, Märtha; Forsberg, Christina; Wahren, Lis Karen (2002). "Normal oral, rectal, tympanic and axillary body temperature in adult men and women: a systematic literature review". Scandinavian Journal of Caring Sciences. 16 (2): 122–8. doi:10.1046/j.1471-6712.2002.00069.x. PMID 12000664.
- Wong, Lena (2005). "Temperature of a Healthy Human (Body Temperature)". The Physics Factbook. Retrieved 2007-08-22.
- Kiekkas, P; Stefanopoulos, N; Bakalis, N; Kefaliakos, A; Karanikolas, M (April 2016). "Agreement of infrared temporal artery thermometry with other thermometry methods in adults: systematic review". Journal of Clinical Nursing. 25 (7–8): 894–905. doi:10.1111/jocn.13117. PMID 26994990.
- Zhen, C; Xia, Z; Long, L; Pu, Y (October 2014). "Accuracy of infrared ear thermometry in children: a meta-analysis and systematic review". Clinical Pediatrics. 53 (12): 1158–65. doi:10.1177/0009922814536774. PMID 24879119. S2CID 24982111.
- Dodd, Susanna R.; Lancaster, Gillian A.; Craig, Jean V.; Smyth, Rosalind L.; Williamson, Paula R. (April 2006). "In a systematic review, infrared ear thermometry for fever diagnosis in children finds poor sensitivity". Journal of Clinical Epidemiology. 59 (4): 354–7. doi:10.1016/j.jclinepi.2005.10.004. PMID 16549256.
- McKenzie, Jack E.; Osgood, David W. (2004). "Validation of a new telemetric core temperature monitor". Journal of Thermal Biology. 29 (7–8): 605. doi:10.1016/j.jtherbio.2004.08.020.
- Nidermann, Reto; Wyss, Eva; Annaheim, Simon; Psikuta, Agnes; Davey, Sarah; Rossi, René Michel (January 2014). "Prediction of Human Core Body Temperature Using Non-Invasive Measurement Methods". International Journal of Biometereology. 58 (1): 7–15. Bibcode:2014IJBm...58....7N. doi:10.1007/s00484-013-0687-2. PMID 23760405. S2CID 11772946.
- Mendt, Stefan; Maggioni, Martina Ana; Nordine, Michael; Steinach, Mathias; Opatz, Oliver; Belavy, Daniel; Felsenberg, Dieter; Koch, Joachim; Shang, Peng; Hanns-Christian, Gunga; Stahn, Alexander (2017). "Circadian Rhythms in Bed Rest: Monitoring Core Body Temperature via Heat-Flux Approach Is Superior to Skin Surface Temperature". Chronobiology International. 34 (5): 666–676. doi:10.1080/07420528.2016.1224241. PMID 27726448. S2CID 205581198.
- Uth, Marc-Florian; Koch, Jochim; Sattler, Frank (2016). "Body Core Temperature Sensing: Challenges and New Sensor Technologies". Procedia Engineering. 168: 89–92. doi:10.1016/j.proeng.2016.11.154.
- Chudler, Eric H. "Biological Rhythms", Neuroscience for Kids, faculty.washington.edu
- "Man's temperature registered more than 115.7", Bulletin Journal, August 7, 1980
- MacDonald, Fiona. "This Is How a Norwegian Woman Survived The Lowest Body Temperature Ever Recorded". ScienceAlert. Retrieved 9 May 2020.
- Tomita, K., et al. "Examination of factors affecting the intraoral perception of object size: A preliminary study." Journal of oral rehabilitation 44.4 (2017): 237-243.
- Al-Tubaikh, Jarrah Ali. "Infectious Diseases and Tropical Medicine." Internal Medicine. Springer, Cham, 2017. 441-493.
- Inwit Publishing, Inc. and Inwit, LLC – Writings, Links and Software Demonstrations – A Fahrenheit–Celsius Activity, inwit.com
- Oxford Dictionary of English, 2010 edition, entry on "blood heat"
- Collins English Dictionary, 1979 edition, entry on "blood heat"
- Wunderlich, Carl Reinhold August (1868). Das Verhalten der Eigenwärme in Krankheiten [The behavior of the self-warmth in diseases]. Leipzig: O. Wigand.; its 1871 2nd edition translated into English and published with the title On the temperature in diseases: a manual of medical thermometry.
- Fischetti, Mark (2018), "Graphic Science: Goodbye, 98.6", Scientific American, vol. 319, no. 6 (December)