Non-voluntary euthanasia
Non-voluntary euthanasia is euthanasia conducted when the explicit consent of the individual concerned is unavailable, such as when the person is in a persistent vegetative state, or in the case of young children. It contrasts with involuntary euthanasia, when euthanasia is performed against the will of the patient.[1][2]
| Part of a series on |
| Euthanasia |
|---|
| Types |
| Views |
| Groups |
| People |
| Books |
| Jurisdictions |
| Laws |
| Alternatives |
| Other issues |
The different possible situations considered non-voluntary euthanasia are when the decision to end the life of the patient is 1) based on what the incapacitated individual would have wanted if they could be asked, 2) based on what the decision maker would want if he or she were in the patient's place, and 3) made by a doctor based on their own criteria and reasoning.[3]
Legal status
Euthanasia can all be divided into passive or active variants.[4] Passive euthanasia entails the withholding of common treatments, such as antibiotics, necessary for the continuance of life.[5] Active euthanasia entails the use of lethal substances or forces, such as administering a lethal injection, to kill and is the most controversial means. A number of authors consider these terms to be misleading and unhelpful.[5]
Active non-voluntary euthanasia is illegal in all countries in the world, although it is practised in the Netherlands on infants (see below) under an agreement between physicians and district attorneys.[6] Passive non-voluntary euthanasia (withholding life support) is legal in various countries, such as India, Albania, and many parts of the United States and is practiced in English hospitals.[7][8]
Non-voluntary euthanasia has been heavily debated. For example, Len Doyal, a professor of medical ethics and former member of the ethics committee of the British Medical Association, argued for legalization, saying in 2006 that "[p]roponents of voluntary euthanasia should support non-voluntary euthanasia under appropriate circumstances and with proper regulation".[9] Arguing against legalization, Peter Saunders, campaign director for Care Not Killing, an alliance of Christian and disability groups, called Doyal's proposals "the very worst form of medical paternalism whereby doctors can end the lives of patients after making a judgment that their lives are of no value and claim that they are simply acting in their patients' best interests".[10]
Slippery slope debate
Non-voluntary euthanasia is cited as one of the possible outcomes of the slippery slope argument against euthanasia, in which it is claimed that permitting voluntary euthanasia to occur will lead to the support and legalization of non-voluntary and involuntary euthanasia,[11] although other ethicists have contested this idea.[12][13][14]
Non-voluntary euthanasia in the Netherlands
Permitted euthanasia in the Netherlands has been regulated by law since 2002. It states that euthanasia and physician-assisted suicide are not punishable if the attending physician acts in accordance with criteria of due care.[15] Prior to the establishment of that law, euthanasia and assisted suicide in the Netherlands were already tolerated for many years, as for example described by G. van der Wal and R. J. Dillmann in 1994.[16] In a 1994 study, of the studied 5000 requests in the Netherlands, in about 1000 of the cases, doctors prescribed drugs with the explicit goal of shortening the patient's life without the explicit request of the patient, which can be considered cases of non-voluntary euthanasia.[16][17]
Since 2004, the Netherlands, also has a protocol to be followed in cases of euthanasia on children under the age of 12 (see also below), which was ratified by the Dutch National Association of Pediatricians, although the practice remains technically illegal. Together with colleagues and prosecutors, Eduard Verhagen developed the Groningen Protocol, in which cases prosecutors will refrain from pressing charges.[18][19]
Non-voluntary euthanasia on children
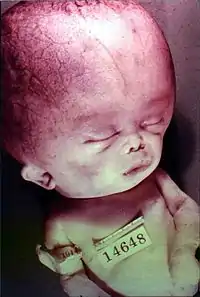
Newborns and euthanasia
Active euthanasia on newborns is illegal throughout the world, with the de facto exception of the Netherlands mentioned above. Because a newborn child is never able to speak for themselves, euthanasia on newborns is by definition non-voluntary. An early example of documented cases of child euthanasia are those performed by the surgeon Harry J. Haiselden in Chicago in the early 20th century.
Ancient Greece
In ancient Greece, non-voluntary euthanasia of children was practiced as an early form of eugenics, the belief and practice of improving the genetic quality of the human population, usually by withdrawing care (i.e. passive euthanasia) rather than a physical extermination, an act termed as “exposure”.[20]
References
- Perrett RW (October 1996). "Buddhism, euthanasia and the sanctity of life". J Med Ethics. 22 (5): 309–13. doi:10.1136/jme.22.5.309. PMC 1377066. PMID 8910785.
- LaFollette, Hugh (2002). Ethics in practice: an anthology. Oxford: Blackwell. pp. 25–26. ISBN 0-631-22834-9.
- Biggs, Hazel (2001). Euthanasia: Death with Dignity and the Law. Hart Publishing. ISBN 1-84113-091-5.
- Rachels J (January 1975). "Active and passive euthanasia". N. Engl. J. Med. 292 (2): 78–80. doi:10.1056/NEJM197501092920206. PMID 1109443.
- Harris, NM. (Oct 2001). "The euthanasia debate". J R Army Med Corps. 147 (3): 367–70. doi:10.1136/jramc-147-03-22. PMID 11766225.
- "Ending the Life of a Newborn: The Groningen Protocol,: Introduction". www.medscape.com. Archived from the original on 2010-11-09. Retrieved 2009-11-03.
- "India joins select nations in legalising "passive euthanasia"". The Hindu. Chennai, India. 7 March 2011. Archived from the original on 11 March 2011.
- "American Journal of Respiratory and Critical Care Medicine". Archived from the original on 2012-07-01. Retrieved 2011-03-09.
- "'Legalise euthanasia' says expert". BBC News Online. 8 June 2006. Archived from the original on 3 April 2012.
- Boseley, Sarah (8 June 2006). "Call for no-consent euthanasia". The Guardian. London. Archived from the original on 25 February 2017.
- "Voluntary Euthanasia". Stanford Encyclopedia of Philosophy. Stanford University. March 29, 2010. Retrieved June 13, 2010.
- Lewis, P. (2007). "The empirical slippery slope from voluntary to non-voluntary euthanasia". J Law Med Ethics. 35 (1): 197–210. doi:10.1111/j.1748-720X.2007.00124.x. PMID 17341228.
- Ryan, CJ. (Oct 1998). "Pulling up the runaway: the effect of new evidence on euthanasia's slippery slope". J Med Ethics. 24 (5): 341–4. doi:10.1136/jme.24.5.341. PMC 1377611. PMID 9800591.
- Manninen, BA. (Nov 2006). "A case for justified non-voluntary active euthanasia: exploring the ethics of the Groningen Protocol". J Med Ethics. 32 (11): 643–51. doi:10.1136/jme.2005.014845. PMC 2563300. PMID 17074822.
- Buiting H, van Delden J, Onwuteaka-Philpsen B, et al. (2009). "Reporting of euthanasia and physician-assisted suicide in the Netherlands: descriptive study". BMC Med Ethics. 10: 18. doi:10.1186/1472-6939-10-18. PMC 2781018. PMID 19860873.
- van der Wal, G. & R. J. Dillmann (1994). "Euthanasia in the Netherlands". British Medical Journal. 308 (6940): 1346–1349. doi:10.1136/bmj.308.6940.1346. PMC 2540255. PMID 8019226.
- Fleming, John (June 1992). "Euthanasia, The Netherlands, and Slippery Slopes". Bioethics Notes Research Occasional Paper (1).
- Verhagen, Eduard; Sauer, Pieter J.J. (2005). "The Groningen Protocol — Euthanasia in Severely Ill Newborns". The New England Journal of Medicine. 352 (10). pp. 959–962. doi:10.1056/NEJMp058026. PMID 15758003.
- "Outrage from Churches over Euthanasia on Newborns". December 1, 2004. Archived from the original on September 28, 2007. Retrieved 2007-05-22.
- Patterson, Cynthia (1985). ""Not Worth the Rearing": Causes of Infant Exposure in Ancient Greece". Transactions of the American Philological Association. 115: 111–123.