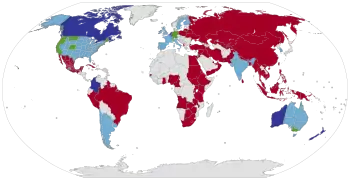
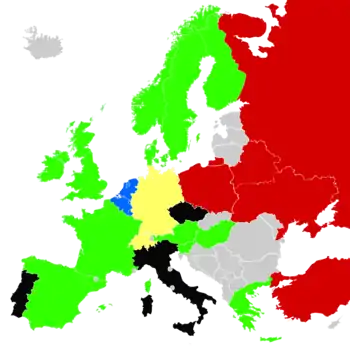
Legality of euthanasia
Efforts to change government policies on euthanasia of humans in the 20th and 21st centuries have met limited success in Western countries. Human euthanasia policies have also been developed by a variety of NGOs, most notably medical associations and advocacy organizations. As of December 2020, active human euthanasia is legal in the Netherlands, Belgium, Colombia,[1] Luxembourg, Western Australia, Spain and Canada.[2] Assisted suicide is legal in Switzerland, Germany, the Australian state of Victoria and in the U.S. states of Washington, Oregon, Colorado, Hawaii, Vermont, Maine,[3] New Jersey,[4] California,[5] and in the District of Columbia.[6]
Timeline legalization active euthanasia at national level
| Country | Legalization method | Date effective | |
|---|---|---|---|
| 1 | Passed by the States General. | 1 April 2002 | |
| 2 | Passed by the Belgian Federal Parliament. | 28 May 2002 | |
| 3 | Passed by the Chamber of Deputies. | 19 March 2009 | |
| 4 | Ruling of the Constitutional Court of Colombia. | 15 December 2014 | |
| 5 | Passed by the Parliament of Canada. | 17 June 2016 | |
| 6 | Passed by the Parliament of New Zealand and approved by the citizens in a binding referendum. | November 2021 | |
| 7 | Passed by the Congress of Deputies. | TBA | |
| 8 | Passed by the Assembly of the Republic. | TBA |
Euthanasia law by country
Argentina
On 9 May 2012, the Argentine Senate turned into law a project that enables to reject treatments that artificially prolong the life of patients with terminal or irreversible symptoms. The consent may be given by the patient or, if not in a position to do so, their relatives or legal representatives. It was promulgated on 24 May 2012 as "Law 26,742".[7]
Australia
The Australian state of Victoria has a law allowing physician-assisted suicide which came into effect in June 2019,[8] with Western Australia passing a similar law in December 2019.[9] Physician-assisted suicide and voluntary euthanasia is illegal in all other Australian states and territories. Although rare, charges have been laid for 'aiding and abetting' the suicide of others.[10] It was once legal in the Northern Territory, by the Rights of the Terminally Ill Act 1995. In 1997, the Australian Federal Government overrode the Northern Territory legislation through the introduction of the Euthanasia Laws Act 1997.[11] Unlike the states, legislation in the Northern Territory is not guaranteed by the Australian constitution. During the brief period in which euthanasia was legal in the Northern Territory, Dr. Philip Nitschke helped three people end their lives through assisted suicide using his Deliverance machine. Organizations such as Exit International want the government to bring back euthanasia rights to Australia. Exit made TV commercials which were banned before they made it to air in September 2010.[12]
Belgium
The Belgian parliament legalised euthanasia on 28 May 2002.[13][14]
A survey published in 2010 reported that those who died from euthanasia (compared with other deaths) were more often younger, male, cancer patients and more often died in their homes. In almost all cases, unbearable physical suffering were reported. Euthanasia for nonterminal patients was rare.[15][16] There have been about 1,400 cases a year since the law was introduced, and a record 1,807 cases were recorded in 2013.[17][18]
In December 2003, the Belgian Senate voted in favour of extending its euthanasia law to terminally ill children. Conditions imposed on children seeking euthanasia are that "the patient must be conscious of their decision and understand the meaning of euthanasia", "the request must have been approved by the child's parents and medical team", "their illness must be terminal" and "they must be in great pain, with no available treatment to alleviate their distress".[19] A psychologist must also determine the patient's maturity to make the decision. The amendment emphasizes that the patient's request be voluntary.[20] The first minor to be euthanized under these new regulations occurred in September 2016.[21]
In September 2014, the Federal Euthanasia Commission gave convicted rapist and murderer Frank Van Den Bleeken the right to assisted suicide. Van Den Bleeken had served decades in prison for a 1989 crime and no longer wished to live. Over a dozen other inmates filed similar petitions.[22] In January 2015, the Justice Ministry acknowledged that Van Den Bleeken's doctors recommended against euthanasia and that alternative psychological care would be sought for him.[23]
In late 2014, a doctor administered a lethal dose of drugs to a patient after struggling with mental illness for years, upon the patient own request. Quote: "Belgium is one of five countries that allow doctors to kill patients at their request, and one of two, along with the Netherlands, that grant the procedure for people with mental illness. The idea is that those with a psychiatric illness should be afforded the same rights as those suffering from a physical one." [24]
In January 2020, the assizes court in Ghent acquitted three doctors of murder charges for an euthanasia in 2010.[25]
Canada
Voluntary active euthanasia, called "physician assisted dying", is legal in Canada for all people over the age of 18 who have a terminal illness that has progressed to the point where natural death is "reasonably foreseeable." To prevent suicide tourism, only people eligible to claim Canadian health insurance may use it. Legalization of the practice came in 2015/2016 as a result of a series of Supreme Court rulings striking down Canada's ban on medically assisted suicide. Below is a timeline of events:
On 6 February 2015, the Supreme Court of Canada unanimously ruled in Carter v Canada (AG) that Canadian adults who are mentally competent and suffering intolerably and permanently have the right to a doctor's help in dying. The court however suspended its ruling for 12 months to give the government an opportunity to write legislation and draft new laws and policies around assisted dying.[26][27] In January 2016 the court granted an additional 4-month extension to its ruling suspension to allow time for the newly elected Liberal government to consult with Canadians on drafting a law to comply with the ruling. As an interim measure, it also ruled that provincial courts can now begin approving applications for euthanasia until the new law passes.[28]
A parliamentary committee report tasked with studying the issue in light of the Supreme Court of Canada's ruling recommended that anyone experiencing "intolerable suffering" should be able to seek a doctor's help to die. On 14 April 2016, Canada's federal Liberal government introduced legislation to legalize assisted dying under more restrictive conditions than recommended by the committee, allowing access to only those with terminal illnesses for whom death is "reasonably foreseeable".[29] The British Columbia Civil Liberties Association argues that the government's assisted dying law is unconstitutional, because it limits access to only those whose death is "reasonably foreseeable", rather than provide access to anybody suffering from a "grievous and irremediable" condition, the definition used by the Supreme Court of Canada in their court ruling that the BCCLA argues would include non-terminal conditions.[30]
The bill received considerable multi-partisan opposition within the Senate, where it was criticized as being drafted too quickly, and being too restrictive compared with the Supreme Court decision.[31] As a result, the Senate made a series of amendments to the bill. The House of Commons accepted all of the amendments made by the Senate except one, which removed the requirement that death be "reasonably foreseeable."
On 17 June 2016, a bill to legally allow assisted suicide within Canada became law after it passed both houses of the Parliament of Canada and received Royal Assent.[32]
Chile
Active euthanasia or assisted suicide are not legal in Chile. Passive euthanasia, however, is legal. Since 2012, the regulation of patients' rights creates the right to informed consent, which allows accepting or refusing any medical treatment. Patients can refuse treatment when they are terminal.[33] Currently, a bill to allow active euthanasia and assisted suicide is being discussed by the congress.[34][35] The bill was approved in general by the Chamber of Deputies on 12 December 2020.[36]
Colombia
In a 6–3 decision, Colombia's Constitutional Court ruled in 1997 that "no person can be held criminally responsible for taking the life of a terminally ill patient who has given clear authorization to do so," according to the Washington Post.[37] The court defined "terminally ill" person as those with diseases such as "cancer, AIDS, and kidney or liver failure if they are terminal and the cause of extreme suffering," the Post reported. The ruling specifically refused to authorize euthanasia for people with degenerative diseases such as Alzheimer's, Parkinson's, or Lou Gehrig's disease. On 15 December 2014, the Constitutional Court had given the Ministry of Health and Social Protection 30 days to publish guidelines for the healthcare sector to use in order to guarantee terminated ill patients, with the wish to undergo euthanasia, their right to a dignified death.[38]
Denmark
Parliament has assigned ethics panels over the years that have advised against legalisation each time[39] however it is still not specifically outlawed[40] and a study published in 2003 showed 41% of deaths under medical supervision involved doctors taking "end-of-life" decisions to help ease their patients' suffering before death (about 1% of which were via prescription drugs).[41][42]
Finland
Active euthanasia is not legal in Finland. Passive euthanasia, however, is legal.[43]
France
In July 2013, French President François Hollande stated his personal support for decriminalisation of voluntary euthanasia in France, which had been one of his presidential campaign promises ("introduction of the right to die with dignity"), despite objections from France's National Consultative Ethics Committee/ Comité national consultatif d'éthique, which alleged "abuses" in adjacent jurisdictions that have decriminalised and regulated either voluntary euthanasia or physician-assisted suicide (Belgium, Switzerland, the Netherlands and Luxembourg). More socially conservative members of the Catholic Church and other major religious groups in France had announced that after expressing an opposition to the introduction of same-sex marriage in France, their next target may be the possible decriminalisation of voluntary euthanasia.[44]
In January 2016 both houses of France's parliament approved a measure that, while stopping short of euthanasia, would allow doctors to keep terminal patients sedated until death.[45]
Germany
Passive euthanasia is legal in Germany if the patient has requested it.[46] On 17 May 2014 the Federal Constitutional Court legalized passive euthanasia by means of the withdrawal of life support to patients who request euthanasia. Forms of active euthanasia, including the lethal compound administration, are illegal.
On 6 November 2015, the German Parliament passed a bill incriminating assisted suicide if it is done in a business-like manner. "Business-like" was meant by the legislator to include any recurrent assistance. Consequently, it typically included physicians. There did not need to be an intention to gain benefits.[47]
On 2 March 2017, the Federal Administrative Court ruled that, in extreme circumstances, it was illegal that an agency denied access to life-ending substances. The relevant legal basis must be interpreted in accordance with the fundamental right to personal self-determination.[48][49]
On 7 May 2019, the Federal Court of Justice, changing its previous judicature from 1984,[50] confirmed that doctors have no obligation to stop the death of a person who, pursuant to a valid autonomous decision, attempts suicide.[51]
On 26 February 2020, the Federal Constitutional Court ruled the provision which penalized assisted suicide services unconstitutional and thus void. The provision violated the fundamental right to personal self-determination.[52][53][54]
India
Passive euthanasia is legal in India.[55] On 7 March 2018 the Supreme Court of India legalised passive euthanasia by means of the withdrawal of life support to patients in a permanent vegetative state.[56][57] Forms of active euthanasia, including the administration of lethal compounds, are illegal.[58]
Ireland
In Ireland, it is illegal for a doctor (or anyone) to actively contribute to someone's death. It is not, however, illegal to remove life support and other treatment (the "right to die") should a person (or their next of kin) request it. A September 2010 Irish Times poll showed that a majority, 57% of adults, believed that doctor-assisted suicide should be legal for terminally ill patients who request it.[59] Doctors can stop giving a patient life sustaining treatments such as ventilators, feeding tube etc. after being sedated, allowing the patient to die peacefully in their sleep.This only occurs in certain circumstances.[60]
On 7 October 2020 the Dying with Dignity Bill[61] passed its second reading and a delaying amendment was defeated, moving Ireland closer towards the legalisation of assisted dying.[62]
Israel
The Israeli Penal Law forbids causing the death of another and specifically forbids shortening the life of another. Active euthanasia has been accepted in some cases under Israeli law.[63] In 2005, proposals were put forward to allow passive euthanasia to be administered using a switch mechanism similar to Sabbath clocks.[64] In 2006, the Steinberg Commission was set up to look into whether life and death issues could be rethought in the context of Jewish law, which suggested that hospitals could set up committees to determine whether patients would be given passive euthanasia.[65]
Japan
The Japanese government has no official laws on the status of euthanasia and the Supreme Court of Japan has never ruled on the matter. Rather, to date, Japan's euthanasia policy has been decided by two local court cases, one in Nagoya in 1962, and another after an incident at Tokai University in 1995. The first case involved "passive euthanasia" (消極的安楽死, shōkyokuteki anrakushi) (i.e., allowing a patient to die by turning off life support) and the latter case involved "active euthanasia" (積極的安楽死, sekkyokuteki anrakushi) (e.g., through injection). The judgments in these cases set forth a legal framework and a set of conditions within which both passive and active euthanasia could be legal. Nevertheless, in both of these particular cases the doctors were found guilty of violating these conditions when taking the lives of their patients. Further, because the findings of these courts have yet to be upheld at the national level, these precedents are not necessarily binding. Nevertheless, at present, there is a tentative legal framework for implementing euthanasia in Japan.[66]
In the case of passive euthanasia, three conditions must be met:
- the patient must be suffering from an incurable disease, and in the final stages of the disease from which he/she is unlikely to make a recovery;
- the patient must give express consent to stopping treatment, and this consent must be obtained and preserved prior to death. If the patient is not able to give clear consent, their consent may be determined from a pre-written document such as a living will or the testimony of the family;
- the patient may be passively euthanized by stopping medical treatment, chemotherapy, dialysis, artificial respiration, blood transfusion, IV drip, etc.
For active euthanasia, four conditions must be met:
- the patient must be suffering from unbearable physical pain;
- death must be inevitable and drawing near;
- the patient must give consent. (Unlike passive euthanasia, living wills and family consent will not suffice.)
- the physician must have (ineffectively) exhausted all other measures of pain relief.
The problems that arose from this, in addition to the problem faced by many other families in the country, has led to the creation of "bioethics SWAT teams".[67] These teams will be made available to the families of terminally ill patients in order to help them, along with the doctors, come to a decision based on the personal facts of the case. Though in its early stages and relying on "subsidies from the Ministry of Health, Labor and Welfare" there are plans to create a nonprofit organization to "allow this effort to continue."[68]
Latvia
Euthanasia is not legal in Latvia.[69] However a doctor may refuse further treatment of a patient if they believe it is the best course of action.[70]
Lithuania
Euthanasia is not legal in Lithuania.However, as of 2016 a draft of a law about the right to die has been produced.[71]
Luxembourg
The country's parliament passed a bill legalizing euthanasia on 20 February 2008 in the first reading with 30 of 59 votes in favour. On 19 March 2009, the bill passed the second reading, making Luxembourg the third European Union country, after the Netherlands and Belgium, to decriminalise euthanasia. Terminally ill patients will have the option of euthanasia after receiving the approval of two doctors and a panel of experts.[72]
Mexico
In Mexico, active euthanasia is illegal but since 7 January 2008 the law allows the terminally ill —or closest relatives, if unconscious— to refuse medication or further medical treatment to extend life (also known as passive euthanasia) in Mexico City,[73] in the central state of Aguascalientes (since 6 April 2009)[74] and, since 1 September 2009, in the Western state of Michoacán.[75] A similar law extending the same provisions at the national level has been approved by the senate[76] and an initiative decriminalizing active euthanasia has entered the same legislative chamber on 13 April 2007.[77]
Netherlands
In the 1973 "Postma case" a physician was convicted for having facilitated the death of her mother following repeated explicit requests for euthanasia.[78] While upholding the conviction, the court's judgment set out criteria when a doctor would not be required to keep a patient alive contrary to their will. This set of criteria was formalized in the course of a number of court cases during the 1980s.
In 2001,[79] the Netherlands passed a law legalizing euthanasia including physician-assisted suicide.[80] This law codifies the twenty-year-old convention of not prosecuting doctors who have committed euthanasia in very specific cases, under very specific circumstances. The Ministry of Public Health, Wellbeing and Sports claims that this practice "allows a person to end their life in dignity after having received every available type of palliative care."[81] The United Nations has reviewed and commented on the Netherlands euthanasia law.[82]
In September 2004 the Groningen Protocol was developed, which sets out criteria to be met for carrying out child euthanasia without the physician being prosecuted.[83]
New Zealand
Assisted suicide and voluntary euthanasia are illegal in New Zealand under Section 179 of the New Zealand Crimes Act 1961, which renders it a criminal offence to "aid and abet suicide."
Two decriminalisation attempts – the Death With Dignity Bill 1995 and the Death With Dignity Bill 2003 – failed, the latter by only a three-vote margin within the New Zealand Parliament. In May 2012, Labour Party of New Zealand MP Maryan Street introduced a private member's bill into the ballot box, the End of Life Choices Bill, which was taken over by MP Iain Lees-Galloway when she failed to get re-elected in the 2014 General Election. The bill was dropped in December 2014 at the request of Labour Party leader Andrew Little as the issue was deemed to be distracting from bigger issues that concerned the party.[84]
In November 2019, ACT MP David Seymour's End of Life Choice Bill, which will legalise assisted suicide for a select group of people if successful, passed its third reading 69 votes in favor to 51 opposed. In return for the New Zealand First party's support of the bill through its third reading, the bill be subject to a binding referendum held alongside the 2020 general election,[85] which will take place on 17 October 2020.[86] If a majority of voters support the referendum, the End of Life Choice Act will come into force 12 months after the official referendum results are declared.[87]
The End of Life Choice binding referendum passed with 65.1% of the vote on 30 October 2020.[88]
Norway
Active voluntary euthanasia remains illegal, though a caregiver may receive a reduced punishment for taking the life of someone who consents to it.[89] Passive euthanasia is legal.
Peru
Euthanasia is a delict under the laws of Peru, although there have been some attempts to reform them.
In October 2009, the Reviser Special Commission of the Penal Code of the Parliament expressed its support of a proposal that tried to amend article 112 of the Penal Code, but it did not succeed.
However, at the beginning of 2015, the case of the Chilean woman young Valentina Maureira, who suffered from cystic fibrosis, an incurable disease, and who asked that euthanasia be allowed in her country, attracted the interest of the press of Chile and also of foreign media.[90]
On 4 March of the same year, the Peruvian legislator Roberto Angulo Álvarez, membership of Dignity and Democracy parliamentary group, motivated by this case, presented a bill that proposed to allow assisted death in case of terminal or degenerative disease, with the objective of "avoid the physical and psychological pains of the patient, as well the unnecessary expenses for the family members and the State". Angulo Álvarez also argued that his legislative project "would contribute to respect for individual freedom and human dignity".[91][92]
Poland
Active euthanasia in the Polish Criminal Code is defined as always appearing under the influence of sympathy for the suffering person and at their request. It is forbidden; it is treated as a kind of murder punishable in a milder way. The perpetrator is punishable by imprisonment of between 3 months and 5 years. Exceptionally, a court may apply leniency or even waive the sentence. The provision of Article 150 of the Penal Code, which defines the crime of euthanasia murder, does not, however, explicitly require the person requesting it to be terminally ill, but this requirement is introduced by case law. A specific type of crime related to euthanasia in the broad sense of the term is assistance to suicide (Article 151 of the Penal Code), which also includes so-called euthanasic assistance to suicide, i.e. facilitating the suicide of a terminally ill person.
Portugal
The issue hit the headlines following a petition calling for euthanasia to be legalized, it rode headlong into controversy with the full knowledge of the nursing staff.[93]
One of the current ‘hot topics’ in Portugal, the deeply divisive issue was latest point of friction between faith and politics in a Catholic and a Republican country.[94] A proposal to make Portugal one of only a handful of countries allowing euthanasia and doctor-assisted suicide was narrowly rejected (115-110 vote) by lawmakers on late May 2018.[95]
Following the 2019 elections the issue began to be discussed again in the Assembly of the Republic, where, as of February 2020, it is expected to be approved by left-wing and liberal parties.[96][97][98]
On 20 February 2020, the Portuguese Parliament voted to approve plans to introduce voluntary euthanasia laws.[99] On January 29, 2021, the Assembly of the Republic approved the final version of the law, with 136 votes supporting the bill.[100] It is yet to be enacted by the President of the Republic and subsequently published.
Philippines
Euthanasia is illegal in the Philippines. In 1997, the Philippine Senate considered passing a bill legalizing passive euthanasia. The bill met strong opposition from the country's Catholic Church. If legalized the Philippines would have been the first country to legalize euthanasia. Under current laws, doctors assisting a patient to die can be imprisoned and charged with malpractice.[101]
South Korea
The National Assembly and The Ministry of Health and Welfare voted in favor of active and passive euthanasia and went into effect since February 2018, and has announced to issue a "Well-Dying" Bill.[102] However, the topic and debate of euthanasia in South Korea sparked for a long time, starting back on 4 December 1997 when a doctor was sent to prison for a major duration for voluntarily cutting life support of a braindead patient who injured himself from a head trauma, upon the request of his wife. This incident is well known in Korea as 'Boramae Hospital Incident' (보라매병원 사건). Another incident that sparked further debate was from the imprisonment of a father who plugged off a respirator for his braindead son.[103]
Patients who qualify for active or passive euthanasia in South Korea are reserved for the terminally ill with a nonexistent chance of recovery. Patients who have a beneficial reaction to any medications, or are not in a rapidly deteriorating state of health leading to imminent death may not be qualified. Patients must have a confirmation of a registered physician and a doctor to die under dignity, and comatose patients must have the approval of both guardians.[104]
Spain
Active euthanasia or assisted suicide are not legal in Spain. Passive euthanasia, however, is legal.
In February 2020 the Spanish parliament voted to approve plans to legalise voluntary euthanasia. The bill will now go to committee and the Senate before a final vote in the lower house.[105] The lower house approved the bill in December 2020.[106]
On 17 December 2020, the Congress of Deputies passed a bill to regulate the right to euthanasia.[107] The final draft, whose intellectual authorship was attributed to María Luisa Carcedo, commanded the support from 192 legislators (PSOE, Podemos, ERC, Ciudadanos, Junts per Catalunya, PNV, Bildu, CUP, Más País, BNG), the opposition from 138 (PP, Vox, UPN) and 2 abstentions.[107][108] Given widespread parliamentary support and the incorporation of amendments, the law is expected to be directly passed by the Senate, sanctioned by the King and then published in the BOE, without needing to return to the Congress of Deputies.[108]
Sweden
Passive euthanasia was deemed legal after a landmark court ruling in 2010. That means a health care professional can legally cease life support upon request from a patient if they understand the consequences stated by their health care provider, and administering a lethal substance is also illegal.[109]
Switzerland
In Switzerland, deadly drugs may be prescribed to a Swiss person or to a foreigner, where the recipient takes an active role in the drug administration.[110] More generally, article 115 of the Swiss penal code, which came into effect in 1942 (having been written in 1918), considers assisting suicide a crime only if the motive is selfish.
Turkey
Euthanasia is strictly forbidden in Turkey. The aide who helped a person to suicide or other ways to kill oneself will be punished for assisting and encouraging suicide under the stipulation of article 84 of the Turkish Criminal Law. In condition of active euthanasia, article 81 of the same law sets forth that any person who carries out this act will be judged and punished for life imprisonment just like a simple murder.
United Kingdom
Active euthanasia is illegal in the United Kingdom. Any person found to be assisting suicide is breaking the law and can be convicted of assisting suicide or attempting to do so.[111][112][113] Between 2003 and 2006 Lord Joffe made four attempts to introduce bills that would have legalised voluntary euthanasia – all were rejected by the UK Parliament.[114] Currently, Dr Nigel Cox is the only British doctor to have been convicted of attempted euthanasia. He was given a 12-month suspended sentence in 1992.[115]
In regard to the principle of double effect, in 1957 Judge Devlin in the trial of Dr John Bodkin Adams ruled that causing death through the administration of lethal drugs to a patient, if the intention is solely to alleviate pain, is not considered murder even if death is a potential or even likely outcome.[116]
Passive euthanasia is legal, by way of advance decisions giving patients the right to refuse life saving treatment.[117] Food and liquid can also be withdrawn from someone in a permanent vegetative state without the need for court approval.[118]
United States
Active euthanasia is illegal throughout the United States. Patients retain the rights to refuse medical treatment and to receive appropriate management of pain at their request (passive euthanasia), even if the patients' choices hasten their deaths. Additionally, futile or disproportionately burdensome treatments, such as life-support machines, may be withdrawn under specified circumstances and, under federal law and most state laws only with the informed consent of the patient or, in the event of the incompetence of the patient, with the informed consent of the legal surrogate. The Supreme Court of the United States has not dealt with "quality of life issues" or "futility issues" and appears to only condone active or passive "euthanasia" (not legally defined) when there is clear and convincing evidence that informed consent to the euthanasia, passive or active, has been obtained from the competent patient or the legal surrogate of the incompetent patient.
While active euthanasia is illegal throughout the U.S., assisted suicide is legal in Colorado, Oregon, Hawaii, Washington, Vermont, Maine,[119] New Jersey,[4] California,[120] the District of Columbia,[6] one county in New Mexico, and is de facto legal in Montana.[121][122] Additionally, Louisiana specifically prohibits euthanasia in its Bill of Rights as cruel and unusual punishment.
Uruguay
Since 1933 the Penal Code of Uruguay, article 37, accept Compassionate Homicide, the first legal document that include euthanasia. It's important to say that this legal document didn't use this denomination. In another article, 127, the judge could waive the doctor, if this action was made by patient pledge and the doctor had an honorable reputation.[123] The main source of this Penal Code was Jimenéz de Asúa, a Spanish penalist, that introduce this concept in his book "Libertad de amar y derecho a morir: ensayos de un criminalista sobre eugenesia, eutanasia, endocrinología", published in Madrid/Spain, in 1928.[124] The first proposal to understand Euthanasia as homicide was made by Ruy Santos in his MD thesis, "Da resistencia dos estados mórbidos à therapeutica e da incurabilidade perante a euthanásia", at Faculdade de Medicina da Bahia/Brazil, in 1928. He made a difference between Euthanasia as homicide and Euthanasia as suicide, probably the first citation about Assisted Suicide.[125]
Non-governmental organizations
There are a number of historical studies about the thorough euthanasia-related policies of professional associations. In their analysis, Brody, B. A. et al. (2001). found it necessary to distinguish such topics as euthanasia, physician-assisted suicide, informed consent and refusal, advance directives, pregnant patients, surrogate decision-making (including neonates), DNR orders, irreversible loss of consciousness, quality of life (as a criterion for limiting end-of-life care), withholding and withdrawing intervention, and futility.[126] Similar distinctions presumably are found outside the U.S., as with the highly contested statements of the British Medical Association.[127][128]
On euthanasia (narrowly defined here as directly causing death), Brody sums up the U.S. medical NGO arena:
The debate in the ethics literature on euthanasia is just as divided as the debate on physician-assisted suicide, perhaps more so. Slippery-slope arguments are often made, supported by claims about abuse of voluntary euthanasia in the Netherlands.... Arguments against it are based on the integrity of medicine as a profession. In response, autonomy and quality-of-life-base arguments are made in support of euthanasia, underscored by claims that when the only way to relieve a dying patient's pain or suffering is terminal sedation with loss of consciousness, death is a preferable alternative – an argument also made in support of physician-assisted suicide.[129]
Other NGOs that advocate for and against various euthanasia-related policies are found throughout the world. Among proponents, perhaps the leading NGO is the UK's Dignity in Dying, the successor to the (Voluntary) Euthanasia Society.[130] In addition to professional and religious groups, there are NGOs opposed to euthanasia[131] found in various countries.
References
- "Minsalud deja en firme la resolución con protocolo de eutanasia". El Tiempo (in Spanish). April 2015.
- "Medical Assistance in Dying Bill". Canada's Justice Laws Website. 2016.
- "Governor Mills signs 'Death with Dignity' bill". WCSH.
- "'Aid-in-Dying' Bill Becomes Law in New Jersey". www.governing.com.
- News, Kelsey Dallas, Deseret. "Canadian Catholic group speaks out against proposed assisted suicide bill". Retrieved 6 October 2018.
- "D.C. physician-assisted suicide law goes into effect". The Washington Times. Retrieved 6 October 2018.
- "Qué dice la ley de muerte digna". La Voz del Interior (in Spanish). 7 July 2015.
- "Euthanasia: Victoria becomes the first Australian state to legalise voluntary assisted dying". ABC News. 29 November 2017.
- "Voluntary euthanasia becomes law in WA in emotional scenes at Parliament". Retrieved 24 February 2020.
- R v Shirley Justins [2011] NSWSC 568, Supreme Court (NSW, Australia).
- "Inquiry into the Rights of the Terminally Ill (Euthanasia Laws Repeal) Bill 2008". Law Council of Australia. April 2008. Archived from the original on 4 March 2011. Retrieved 21 April 2011. Cite journal requires
|journal=(help) - Alexander, Cathy (13 September 2010). "Pro-euthanasia TV ad ban 'a violation of free speech'". The Age. Melbourne.
- "Moniteur Belge - Belgisch Staatsblad". www.ejustice.just.fgov.be. Retrieved 6 October 2018.
- Adams M, Nys H (2003). "Comparative reflections on the Belgian Euthanasia Act 2002". Med Law Rev. 11 (3): 353–76. doi:10.1093/medlaw/11.3.353. PMID 16733879.
- Smets T, Bilsen J, Cohen J, Rurup ML, Deliens L (February 2010). "Legal euthanasia in Belgium: characteristics of all reported euthanasia cases". Med Care. 48 (2): 187–92. doi:10.1097/MLR.0b013e3181bd4dde. hdl:1854/LU-5933562. PMID 19890220. S2CID 36399849.
- Aviv, Rachel (22 June 2015). "The Death Treatment". The New Yorker. Retrieved 19 June 2015.
- AP (16 September 2014). "Belgian convicted killer with 'incurable' psychiatric condition granted right to die". The Guardian. Retrieved 3 January 2015.
- Porter, Tim (3 January 2015). "Belgian serial rapist and murderer Frank Van Den Bleeken 'to be euthanised' in January". International Business Times. Retrieved 3 January 2015.
- "Belgian Senate votes to extend euthanasia to children". BBC News. 13 December 2013.
- Higgins, Andrew (12 December 2013). "Belgian Senate Votes to Allow Euthanasia for Terminally Ill Children". The New York Times.
- "Belgium minor first to be granted euthanasia". BBC News. 17 September 2016. Retrieved 17 September 2016.
- "Brussels: Murderer may kill himself". The Week (page 6). 26 September 2014.
- "Belgian rapist Van Den Bleeken refused 'right to die'". BBC News. 6 January 2015. Retrieved 31 January 2018.
- "'What could help me to die?' Doctors clash over euthanasia". STAT News. 26 October 2017. Retrieved 25 September 2020.
- "Vrijspraak voor drie artsen: doek valt over euthanasieproces in Gent" (in Dutch). 31 January 2020.
- Fine, Sean (6 February 2015). "Canadians have right to doctor-assisted suicide, Supreme Court rules". The Globe and Mail.
- Carter v. Canada (Attorney General), 2015 SCC 5, online at: http://scc-csc.lexum.com/scc-csc/scc-csc/en/item/14637/index.do
- "Supreme court gives Parliament 4-month extension on doctor-assisted dying law". 15 January 2016. Retrieved 28 February 2016.
- "Canada's new doctor-assisted dying law takes shape". The Economist. 19 April 2016. Retrieved 6 October 2018.
- "Children of assisted-death advocate Kay Carter urge amendments to Liberal bill". 21 April 2016. Retrieved 6 October 2018.
- Tasker, John Paul (28 May 2016). "'Rushed' assisted-dying legislation to face strong opposition in the Senate". CBC News. Retrieved 1 June 2016.
- "Canada legalises euthanasia for the terminally ill - Her.ie". Retrieved 6 October 2018.
- "Ley. Nº 20.584. Regula los derechos y deberes de los pacientes" (in Spanish). Biblioteca del Congreso Nacional de Chile. 24 April 2012. Retrieved 7 May 2018.
- "Mayoría de Comisión de Salud se inclina por aprobar eutanasia". La Tercera (in Spanish). 20 April 2018. Retrieved 7 May 2018.
- "Comisión de Salud aprueba suicidio asistido en proyecto de eutanasia". La Tercera (in Spanish). 23 April 2019. Retrieved 2 May 2019.
- "Diputados aprueban legislar sobre la eutanasia en Chile". La Tercera (in Spanish). 17 December 2020. Retrieved 17 December 2020.
- "Colombia Debates Court Ruling That Legalizes Mercy Killing". The Washington Post. 18 August 1997. Archived from the original on 29 March 2015. Retrieved 6 October 2018.
- Redacción Salud (19 February 2015). "Los principios para regular la eutanasia" (in Spanish). ElEspectador.com.
- Cook, Michael. "Denmark quietly debates euthanasia". BioEdge. Retrieved 11 October 2014.
- Humphry, Derek (2005). The Good Euthanasia Guide: Where, What, and Who in Choices in Dying. Junction City, Oregon, U.S.A.: Norris Lane Press. p. 4. ISBN 978-0-9768283-1-0.
- "Doctor-assisted euthanasia common in Europe". Australian Broadcasting Commission. Agençe France-Presse. 4 August 2003. Retrieved 11 October 2014.
- van der Heide, Agnes; Deliens, Luc; Faisst, Karin; Nilstun, Tore; Norup, Michael; Paci, Eugenio; van der Wal, Gerrit; van der Maas, Paul J (17 June 2003). "End-of-life decision-making in six European countries: descriptive study" (PDF). The Lancet. 362 (9381): 345–350. doi:10.1016/s0140-6736(03)14019-6. PMID 12907005. S2CID 22917898. Retrieved 11 October 2014.
- Silvoniemi, M.; Vasankari, T.; Vahlberg, T.; Clemens, KE; Salminen, E. (2010). "Physicians' attitudes towards euthanasia in Finland: would training in palliative care make a difference?". Palliative Medicine. 24 (7): 744–746. doi:10.1177/0269216310376556. PMID 20921095. S2CID 35349562.
- "France aims to allow euthanasia despite ethics doubts". TVNZ News. 2 July 2013. Archived from the original on 2 July 2013. Retrieved 2 July 2013.
- "France adopts sedated dying law as compromise on euthanasia". The Guardian. Associated Press. 27 January 2016. ISSN 0261-3077. Retrieved 6 December 2016.
- "The state of euthanasia in Europe". Retrieved 6 October 2018.
- "Assisted Suicide Law In Germany Passes Despite Concerns Over Nazi Association". International Business Times. 6 November 2015. Retrieved 3 October 2018.
- "Licence for acquiring a lethal dose of sodium pentobarbital to commit suicide". Federal Administrative Court. 2 March 2017. Retrieved 7 March 2020.
- "German Federal Court rules patients should have access to life-ending drugs". Retrieved 7 March 2020.
- "Teilnahme am Suizid". Retrieved 7 March 2020.
- "German court clears two doctors present as patients committed suicide". Retrieved 7 March 2020.
- "Criminalisation of assisted suicide services unconstitutional". Bundesverfassungsgericht. Retrieved 7 March 2020.
- "Germany overturns ban on professionally assisted suicide". Retrieved 26 February 2020.
- "Germany's top court paves the way for assisted suicide". Retrieved 7 March 2020.
- "India joins select nations in legalising "passive euthanasia"". The Hindu. Chennai, India. 7 March 2011. Retrieved 8 March 2011.
- Venkatesan, J. (7 March 2011). "Supreme Court disallows friend's plea for mercy killing of vegetative Aruna". The Hindu. Chennai, India. Retrieved 7 March 2011.
- "Aruna Shanbaug case: SC allows passive euthanasia in path-breaking judgment". The Times of India. 7 March 2011. Retrieved 7 March 2011.
- Magnier, Mark (8 March 2011). "India's Supreme Court lays out euthanasia guidelines". LA Times. Retrieved 8 March 2011.
- "The Irish Times (17 September 2010) – Majority believe assisted suicide should be legal".
- "Alternatives to euthanasia and assisted suicide - HSE.ie". Retrieved 6 October 2018.
- "Dying with Dignity Bill 2020". Retrieved 8 October 2020.
- "Government proposal to block assisted dying Bill voted down in the Dáil". Retrieved 8 October 2020.
- "Euthanasia: The Approach of the Courts in Israel and the Application of Jewish Law Principles". Jewish Virtual Library.
- Butcher, Tim (8 December 2005). "Israelis to be allowed euthanasia by machine". Daily Telegraph. London. Retrieved 6 January 2012.
- Brody, Shlomo (19 November 2009). "Ask the Rabbi: 'Passive euthanasia'". Jerusalem Post. Retrieved 6 January 2012.
- "安楽死". 現代用語の基礎知識. 自由国民社. 2007. pp. 951, 953.
- McDougall & Gorman 2008, p. 89
- McDougall & Gorman 2008, p. 90
- "Euthanasia debated in Latvia". Retrieved 30 January 2018.
- "Medical Treatment Law" (PDF). Valsts valodas centrs. 2015. p. 11, 13.
- "Assisted suicide, euthanasia and the European Association for Palliative Care". 25 February 2016. Retrieved 6 October 2018.
- "Mémorial A n° 46 de 2009 - Legilux" (PDF). www.legilux.public.lu. Archived from the original (PDF) on 13 March 2013. Retrieved 6 October 2018.
- "Publica GDF Ley de Voluntad Anticipada". ElUniversal (in Spanish). Mexico City. Notimex. 7 January 2008. Retrieved 25 September 2009.
- Rodríguez, Susana; Salazar, Aníbal (8 April 2009). "Sólo falta reglamentar la voluntad anticipada para aplicarla: Ruvalcaba". La Jornada Aguascalientes (in Spanish). Archived from the original on 27 February 2012. Retrieved 26 September 2009.
- "Michoacán aprueba Ley de Voluntad Anticipada". El Economista (in Spanish). Morelia, Mexico. Notimex. 1 September 2009. Retrieved 25 September 2009.
- "Senado México aprueba a enfermos terminales rehusar tratamientos". EcoDiario (in Spanish). Mexico. Reuters. 26 November 2008. Retrieved 25 September 2009.
- "Mexico moves to legalise euthanasia". Reuters. Mexico City. 13 April 2007. Retrieved 25 September 2009.
- Rietjens JA, van der Maas PJ, Onwuteaka-Philipsen BD, van Delden JJ, van der Heide A (September 2009). "Two Decades of Research on Euthanasia from the Netherlands. What Have We Learnt and What Questions Remain?". J Bioeth Inq. 6 (3): 271–283. doi:10.1007/s11673-009-9172-3. PMC 2733179. PMID 19718271.
- "Dutch 'mercy killing law' passed". BBC. 11 April 2001.
- Janssen, André (2002). "The New Regulation of Voluntary Euthanasia and Medically Assisted Suicide in the Netherlands". Int J Law Policy Family. 16 (2): 260–269. doi:10.1093/lawfam/16.2.260. PMID 16848072.
- Sport, Ministerie van Volksgezondheid, Welzijn en. "Ministerie van Volksgezondheid, Welzijn en Sport". www.minvws.nl. Retrieved 6 October 2018.
- "HUMAN RIGHTS COMMITTEE CONCLUDES SEVENTY-SECOND SESSION | Meetings Coverage and Press Releases". www.un.org. Retrieved 5 August 2019.
- Verhagen E, Sauer PJ (March 2005). "The Groningen protocol—euthanasia in severely ill newborns". N. Engl. J. Med. 352 (10): 959–62. doi:10.1056/NEJMp058026. PMID 15758003.
- @isaac_davison, Isaac Davison Political reporter, NZ Herald isaac davison@nzherald co nz (14 December 2014). "Labour MP drops euthanasia bill". Retrieved 6 October 2018 – via www.nzherald.co.nz.
- "Euthanasia bill passes 69-51, sending the final decision to a referendum". Stuff. Retrieved 28 November 2019.
- "Prime Minister Jacinda Ardern changes election date to 17 October". RNZ. 17 August 2020. Retrieved 18 August 2020.
- "Referendum on the End of Life Choice Act 2019". referendum.govt.nz. New Zealand Government. Retrieved 28 January 2020.
- "Official Count - Referendums Results". electionresults.govt.nz. Electoral Commission New Zealand. Retrieved 15 November 2020.
- "Straffeloven 2005". Criminal Law 2005. 20 May 2005. Retrieved 19 April 2016.
- "Michelle Bachelet visita en el hospital a Valentina, la niña que le pidió eutanasia". La República. 1 March 2015. Retrieved 22 June 2017.
- "Roberto Ángulo presenta proyecto de ley que permita eutanasia a pacientes terminales". Diario Correo. 5 March 2015. Retrieved 22 June 2017.
- "Conozca más sobre el proyecto de ley para legalizar la eutanasia en el Perú". La República. 9 March 2015. Retrieved 22 June 2017.
- portugalpress (29 February 2016). "Nursing chief claims Portugal "already practises euthanasia" in state hospitals". Retrieved 6 October 2018.
- portugalpress (6 February 2018). "Parties to debate legalisation of euthanasia". Retrieved 6 October 2018.
- "Euthanasia is rejected by Portugal's parliament". Retrieved 6 October 2018.
- "Eutanásia. Despenalização passa, referendo não - DN". www.dn.pt (in Portuguese). Retrieved 13 February 2020.
- "Eutanásia. A decisão mais importante da nossa vida (por Alexandre Quintanilha)". Jornal Expresso (in Portuguese). Retrieved 13 February 2020.
- Alves, Natália Faria, José. "Eutanásia: tudo o que os partidos propõem". PÚBLICO (in Portuguese). Retrieved 13 February 2020.
- "Politicians in Portugal vote to allow euthanasia". Retrieved 20 February 2020.
- Francisco, Susete (29 January 2021). "Eutanásia aprovada no Parlamento com 136 votos favoráveis". Diário de Notícias (in Portuguese). Retrieved 29 January 2021.
- Wallerstein, C (1997). "Philippines considers euthanasia bill". BMJ. 314 (7095): 1644. doi:10.1136/bmj.314.7095.1641i. PMC 2126848. PMID 9193287.
- "New law enables South Koreans to 'die well'". The Straits Times. 28 January 2016. Retrieved 29 January 2016.
- "Euthanasia Legal for the Terminally Ill In S.Korea Now". Med India. Tanya Thomas. 15 July 2010. Retrieved 15 July 2010.
- "Korea to Temporarily Allow Terminally Ill Patients to Choose Death with Dignity". 조선일보. Choi Won-woo. Retrieved 23 October 2017.
- "Spanish Government Passes 1st Hurdle to Legalize Euthanasia". Retrieved 21 February 2020.
- "Spain's lower house approves euthanasia bill". Retrieved 17 December 2020.
- Hermida, Xosé (17 December 2020). "El Congreso aprueba la primera ley de eutanasia con una holgada mayoría". El País (in Spanish).
- Daniele, Laura (17 December 2020). "El Congreso aprueba por amplia mayoría la ley de eutanasia". ABC.
- "Sweden allows passive euthanasia". The Swedish Wire. AFP. 26 April 2010.
- Lundin, Leigh (2 August 2009). "YOUthanasia". Criminal Brief. Retrieved 27 August 2009.
- Suicide Act 1961 s.2
- Smartt, Ursula (2009). "Euthanasia and the Law". Criminal Law & Justice Weekly. 173 (7): 100.
- "Suicide: Policy for Prosecutors in Respect of Cases of Encouraging or Assisting Suicide - The Crown Prosecution Service". www.cps.gov.uk. Retrieved 6 October 2018.
- "Assisted Dying Bill – latest". BBC News Online.
- "Case Histories: end of life decisions". 10 May 2002. Retrieved 6 October 2018 – via news.bbc.co.uk.
- Otlowski, Margaret (1997). Voluntary Euthanasia and the Common Law. Clarendon Press. pp. 175–177. ISBN 978-0-19-825996-1.
- "Advance decision (living will) - NHS.UK". 29 May 2018.
- "Supreme Court backs agreed end-of-life decisions". BBC News. 30 July 2018.
- Villeneuve, Marina (13 June 2019). "Maine becomes 8th state to legalize assisted suicide". AP NEWS.
- Karlamangla, Soumya (12 May 2016). "How California's aid-in-dying law will work". Los Angeles Times. Retrieved 1 June 2016.
- O'Reilly, Kevin B. (18 January 2010). "Physician-assisted suicide legal in Montana, court rules". American Medical News.
- Eckholm, Erik (7 February 2014). "'Aid in Dying' Movement Takes Hold in Some States". The New York Times.
- Reta A, Grezzi O. Código penal de la República Oriental del Uruguay. 4th ed. Montevideo: Fundación de Cultura Universitaria; 1996.
- Asúa LJ de. Libertad de amar y derecho a morir: ensayos de un criminalista sobre eugenesia, eutanasia, endocrinología. Madrid: Historia Nueva; 1928.
- Santos R. Da euthanásia nos incuráveis dolorosos. These de doutoramento. Salvador (Bahia): Faculdade de Medicina da Bahia; 1928.
- Brody, B. A.; Rothstein, M. A.; McCullough, L. B.; Bobinski, M. A. (2001). Medical Ethics: Analysis of the Issues Raised by the Codes, Opinions and Statements. BNA Books.
- On the BMA controversy. Archived 28 November 2006 at the Wayback Machine
- For professional policies in the English-speaking world, see this selection by an advocacy NGO.
- Brody, B. A. et al. (2001), p. 283
- Dignity in Dying. In an unsympathetic account, the International Task Force on Euthanasia and Assisted Suicide has detailed the ebb and flow of euthanasia proponents. Archived 10 October 2007 at the Wayback Machine
- "Euthanasia suicide mercy-killing right-to-die physician assisted suicide living wills research". www.euthanasia.com. Retrieved 6 October 2018.
Works cited
- McDougall, Jennifer Fecio; Gorman, Martha (2008). Euthanasia: A Reference Handbook. Santa Barbara: ABC-CLIO. p. 89. ISBN 978-1-59884-121-3.
External links
- Focarelli, Carlo. Euthanasia, Max Planck Encyclopedia of Public International Law
- Downie J, Chambaere K, Bernheim JL (2012). "Pereira's attack on legalizing euthanasia or assisted suicide: Smoke and mirrors". Current Oncology. 19 (3): 133–8. doi:10.3747/co.19.1063. PMC 3364762. PMID 22670091.