Shellfish allergy
Shellfish allergy is among the most common food allergies. "Shellfish" is a colloquial and fisheries term for aquatic invertebrates used as food, including various species of molluscs such as clams, mussels, oysters and scallops, crustaceans such as shrimp, lobsters and crabs, and cephalopods such as squid and octopus. Shellfish allergy is an immune hypersensitivity to proteins found in shellfish. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus.[2] Shellfish is one of the eight common food allergens, responsible for 90% of allergic reactions to foods: cow's milk, eggs, wheat, shellfish, peanuts, tree nuts, fish, and soy beans.[3][4]
| Shellfish allergy | |
|---|---|
 | |
| Shellfish (shrimp, crab legs, mussels) on platter | |
| Specialty | Immunology |
| Frequency | Shellfish allergy frequency estimated at ~0.5-2.5% (self-reported)[1] |
Unlike early childhood allergic reactions to milk and eggs, which often lessen as the children age,[5] shellfish allergy tends to first appear in school-age children and older, and persist in adulthood.[6] Strong predictors for adult-persistence are anaphylaxis, high shellfish-specific serum immunoglobulin E (IgE) and robust response to the skin prick test. Adult onset of fish allergy is common in workers in the shellfish catching and processing industry.[7][8]
Signs and symptoms
Food allergies in general usually have a fast onset (from seconds to one hour).[9] Symptoms may include: rash, hives, itching of mouth, lips, tongue, throat, eyes, skin, or other areas, swelling of lips, tongue, eyelids, or the whole face, difficulty swallowing, runny or congested nose, hoarse voice, wheezing, shortness of breath, diarrhea, abdominal pain, lightheadedness, fainting, nausea, or vomiting.[9] Symptoms of allergies vary from person to person and may vary from incident to incident.[9] Serious danger regarding allergies can begin when the respiratory tract or blood circulation is affected. The former can be indicated by wheezing, a blocked airway and cyanosis, the latter by weak pulse, pale skin, and fainting. When these symptoms occur the allergic reaction is called anaphylaxis.[9] Anaphylaxis occurs when IgE antibodies are involved, and areas of the body that are not in direct contact with the food become affected and show severe symptoms.[9][10] Untreated, this can proceed to vasodilation, a low blood pressure situation called anaphylactic shock.[10]
Causes
Eating shellfish
The cause is typically the eating of shellfish or foods that contain shellfish. The shellfish types causing clinical allergy are, in decreasing incidence, shrimp, crab, lobster, clam, oyster and mussel.[11] Once an allergic reaction has occurred it usually remains a lifelong sensitivity.[12] Briefly, the immune system overreacts to proteins found in shellfish, most commonly to tropomyosin, but often to other proteins, such as arginine kinase, myosin light chain and sarcoplasmic calcium-binding protein.[13][14][15] The allergic reaction to fish is to a different protein, parvalbumin, so there is no cross-reactivity between fish and shellfish allergy.[6][16][17]
Cross-contact
Cross-contact, also referred to as cross-contamination, occurs when foods are being processed in factories or at food markets, or are being prepared for cooking in restaurants and home kitchens. The allergenic proteins are transferred from one food to another.[18]
Shellfish parasite
The food-borne parasite Anisakis is a genus of nematodes known to be present in squid.[19]Anisakis are directly infective to humans whenever infected squid (or marine fish) are consumed raw or slightly processed, causing a condition call anisakiasis. Symptoms from consuming live nematodes include severe abdominal pain, nausea, and vomiting.[20] In addition, there can be an allergic reaction to Anisakis proteins, even if the food in question was frozen or cooked before being consumed, killing the nematodes, as some of the nematode proteins are resistant to cold and heat.[19] Allergic reactions can include hives, asthma and true anaphylactic reactions.[12][21]
Occupational exposure
An industry review conducted in 1990 estimated that 28.5 million people worldwide were engaged in some aspect of the seafood industry: fishing, aquaculture, processing and industrial cooking. Men predominate in fishing, women in processing facilities.[7] Exposure to shellfish allergenic proteins includes inhalation of wet aerosols from fresh shellfish handling, and dermal contact through skin breaks and cuts.[7][8] Prevalence of seafood-induced adult asthma is on the order of 10% (higher for crustaceans and lower for fish). Prevalence of skin allergy reactions, often characterized by itchy rash (hives), range from 3% to 11%. The shellfish-induced health outcomes are mainly due to the protein tropomyosin causing an IgE mediated immune system response.[7][8]
Cross-reactivity to non-shellfish
Tropomyosin, the major allergen in shellfish allergy, is also found in house dust mites and cockroaches.[14][15] Exposure to inhaled tropomyosins from dust mites is thought to be the primary sensitizer for shellfish allergy, an example of inhalant-to-food cross-reactivity.[22] Epidemiological surveys have confirmed correlation between shellfish and dust mite sensitizations. An additional confirmation was seen in Orthodox Jews with no history of shellfish consumption, in that skin tests confirming dust mite allergy were also positive for shellfish tropomyosin.[14][23] In addition to tropomyosin, arginine kinase and hemocyanin seem to have a role in cross-reactivity to dust mites.[13]
Exercise as contributing factor
Exercise can be a contributing factor to an allergic food response. There is a condition called food-dependent, exercise-induced anaphylaxis. For people with this condition, exercise alone is not sufficient, nor consumption of a food to which they are mildly allergic sufficient, but when the food in question is consumed within a few hours before high intensity exercise, the result can be anaphylaxis. Shellfish are specifically mentioned as a causative food.[24][25][26] One theory is that exercise is stimulating the release of mediators such as histamine from IgE-activated mast cells.[26] Two of the reviews postulate that exercise is not essential for the development of symptoms, but rather that it is one of several augmentation factors, citing evidence that the culprit food in combination with alcohol or aspirin will result in a respiratory anaphylactic reaction.[24][26]
Mechanisms
Allergic response
Conditions caused by food allergies are classified into three groups according to the mechanism of the allergic response:[4]
- IgE-mediated (classic) – the most common type, manifesting acute changes that occur shortly after eating, and may progress to anaphylaxis
- Non-IgE mediated – characterized by an immune response not involving immunoglobulin E; may occur hours to days after eating, complicating diagnosis
- IgE and non-IgE-mediated – a hybrid of the above two types
Allergic reactions are hyperactive responses of the immune system to generally innocuous substances, such as food proteins.[27] Why some proteins trigger allergic reactions while others do not is not entirely clear. One theory holds that proteins which resist digestion in the stomach, therefore reaching the small intestine relatively intact, are more likely to be allergenic, but studies have shown that digestion may abolish, decrease, have no effect, or even increase the allergenicity of food allergens.[28] The heat of cooking structurally degrades protein molecules, potentially making them less allergenic.[29][30]
Hypersensitivities are categorized according to the parts of the immune system that are attacked and the amount of time it takes for the response to occur. The four types of hypersensitivity reaction are: type 1, immediate IgE-mediated; type 2, cytotoxic; type 3, immune complex-mediated; and type 4, delayed cell-mediated.[31] The consequent pathophysiology of allergic responses can be divided into two time periods. The first is an acute response that occurs immediately after exposure to an allergen. This phase can either subside or progress into a "late-phase reaction" which can substantially prolong the symptoms of a response, and result in more tissue damage.
In the early stages of acute allergic reaction, lymphocytes previously sensitized to a specific protein or protein fraction react by quickly producing a particular type of antibody known as secreted IgE (sIgE), which circulates in the blood and binds to IgE-specific receptors on the surface of other kinds of immune cells called mast cells and basophils. Both of these are involved in the acute inflammatory response.[32] Activated mast cells and basophils undergo a process called degranulation, during which they release histamine and other inflammatory chemical mediators called (cytokines, interleukins, leukotrienes, and prostaglandins) into the surrounding tissue causing several systemic effects, such as vasodilation, mucous secretion, nerve stimulation, and smooth-muscle contraction.[32] This results in runny nose, itchiness, shortness of breath, and potentially anaphylaxis.[32] Depending on the individual, the allergen, and the mode of introduction, the symptoms can be system-wide (classical anaphylaxis), or localized to particular body systems; asthma is localized to the respiratory system while hives and eczema are localized to the skin.[32] In addition to reacting to oral consumption, skin reactions can be triggered by contact if there are skin abrasions or cuts.[7][8]

After the chemical mediators of the acute response subside, late-phase responses can often occur due to the migration of other white blood cells such as neutrophils, lymphocytes, eosinophils, and macrophages to the initial reaction sites. This is usually seen 2–24 hours after the original reaction.[33] Cytokines from mast cells may also play a role in the persistence of long-term effects. Late-phase responses seen in asthma are slightly different from those seen in other allergic responses, although they are still caused by release of mediators from eosinophils.[34]
In addition to IgE-mediated responses, shellfish allergy can manifest as atopic dermatitis, especially in infants and young children.[35] Some will display both, so that a child could react to an oral food challenge with allergic symptoms, followed a day or two later with a flare up of atopic dermatitis and/or gastrointestinal symptoms, including allergic eosinophilic esophagitis.[36]
Shellfish allergenic proteins
Several proteins from shellfish are either clearly involved in allergenic reactions or suspected to be. Tropomyosin, arginine kinase, myosin light chain and sarcoplasmic calcium-binding protein are widely present across shellfish species.[13][14][15][37] Troponin, actin, triosephosphate isomerase and hemocyanin are also identified as allergenic proteins.[1][14] As of a 2016 review, only three (tropomyosin, arginine kinase and sarcoplasmic calcium-binding protein) were available for routine diagnostic skin testing.[14] Shellfish do not manifest the proteins β-parvalbumin (found in bony fishes) or α-parvalbumin (found in cartilaginous fishes such as sharks and rays), so there is not cross-reactivity of shellfish allergy to fish allergy.[6][16][17]
Diagnosis
Diagnosis of shellfish allergy is based on the person's history of allergic reactions, skin prick test and measurement of shellfish-specific serum immunoglobulin E (IgE or sIgE). Confirmation is by double-blind, placebo-controlled food challenges.[16] Self-reported shellfish allergy often fails to be confirmed by food challenge.[38]
Prevention
Reviews of food allergens in general stated that introducing solid foods at 4–6 months may result in the lowest subsequent allergy risks for exzema, allergic rhinitis and more severe reactions.[39] The evidence is best for peanuts, eggs and milk.[40] The literature is sparse for consequences of early introduction of shellfish.[40]
Treatment
Treatment for accidental ingestion of shellfish products by allergic individuals varies depending on the sensitivity of the person. An antihistamine such as diphenhydramine may be prescribed. Sometimes prednisone will be prescribed to prevent a possible late phase Type I hypersensitivity reaction.[41] Severe allergic reactions (anaphalaxis) may require treatment with an epinephrine pen, which is an injection device designed to be used by a non-healthcare professional when emergency treatment is warranted.[42] Unlike for egg allergy, for which there is active research on trying oral immunotherapy (OIT) to desensitize people to egg allergens,[43] reviews mention that there are no published clinical trials evaluating oral immunotherapy for shellfish allergy.[6][11]
Prognosis
Unlike milk and egg allergies,[5][44] shellfish allergy usually persists into adulthood.[11][12]
Epidemiology
Incidence and prevalence are terms commonly used in describing disease epidemiology. Incidence is newly diagnosed cases, which can be expressed as new cases per year per million people. Prevalence is the number of cases alive, expressible as existing cases per million people during a period of time.[45] Worldwide, the prevalence of shellfish allergy is increasing because shellfish consumption is increasing,[46] and among adults shellfish is the most common anaphylaxis-eliciting food.[11] Reviews cite self-reported shellfish allergy in range of 0.5 to 2.5 percent in the general population.[1][38][47] Prevalence is higher in coastal southeast Asian countries, where shellfish consumption is more common.[1][11][48][49] Self-reported allergy prevalence is always higher than food-challenge confirmed allergy, which one review put at 0% to 0.9% (the higher value in southeast Asia).[50]
Society and culture
Whether food allergy prevalence is increasing or not, food allergy awareness has definitely increased, with impacts on the quality of life for children, their parents and their immediate caregivers.[51][52][53][54] In the United States, the Food Allergen Labeling and Consumer Protection Act of 2004 causes people to be reminded of allergy problems every time they handle a food package, and restaurants have added allergen warnings to menus. The Culinary Institute of America, a premier school for chef training, has courses in allergen-free cooking and a separate teaching kitchen.[55] School systems have protocols about what foods can be brought into the school. Despite all these precautions, people with serious allergies are aware that accidental exposure can easily occur at other peoples' houses, at school or in restaurants.[56] Food fear has a significant impact on quality of life.[53][54]
Regulation of labelling
In response to the risk that certain foods pose to those with food allergies, some countries have responded by instituting labeling laws that require food products to clearly inform consumers if their products contain major allergens or byproducts of major allergens among the ingredients intentionally added to foods. Nevertheless, there are no labeling laws to mandatory declare the presence of trace amounts in the final product as a consequence of cross-contamination.[57][58][59][60][61]
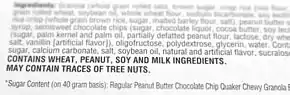
Ingredients intentionally added
In the United States, the Food Allergen Labeling and Consumer Protection Act of 2004 (FALCPA) requires companies to disclose on the label whether a packaged food product contains any of these eight major food allergens, added intentionally: cow's milk, peanuts, eggs, shellfish, fish, tree nuts, soy and wheat.[57] This list originated in 1999 from the World Health Organisation Codex Alimentarius Commission.[62] To meet FALCPA labeling requirements, if an ingredient is derived from one of the required-label allergens, then it must either have its "food sourced name" in parentheses, for example "Casein (milk)," or as an alternative, there must be a statement separate but adjacent to the ingredients list: "Contains milk" (and any other of the allergens with mandatory labeling).[57][59] The European Union requires listing for those eight major allergens plus molluscs, celery, mustard, lupin, sesame and sulfites.[58]
FALCPA applies to packaged foods regulated by the FDA, which does not include poultry, most meats, certain egg products, and most alcoholic beverages.[63] However, some meat, poultry, and egg processed products may contain allergenic ingredients. These products are regulated by the Food Safety and Inspection Service (FSIS), which requires that any ingredient be declared in the labeling only by its common or usual name. Neither the identification of the source of a specific ingredient in a parenthetical statement nor the use of statements to alert for the presence of specific ingredients, like "Contains: milk", are mandatory according to FSIS.[60][61] FALCPA also does not apply to food prepared in restaurants.[64][65] The EU Food Information for Consumers Regulation 1169/2011 requires food businesses to provide allergy information on food sold unpackaged. Examples would include by catering outlets and deli counters, bakeries and sandwich bars.[66]
See also
- List of allergens (food and non-food)
References
- Khora SS (August 2016). "Seafood-Associated Shellfish Allergy: A Comprehensive Review". Immunol Invest. 45 (6): 504–30. doi:10.1080/08820139.2016.1180301. PMID 27404324.
- National Report of the Expert Panel on Food Allergy Research, NIH-NIAID 2003 "June 30 2003.pdf" (PDF). Archived from the original (PDF) on 2006-10-04. Retrieved 2006-08-07.
- "Food Allergy Facts" Archived 2012-10-06 at the Wayback Machine Asthma and Allergy Foundation of America
- "Food allergy". National Health Service (England). 16 May 2016. Retrieved 27 December 2020.
- Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, Kohno Y, Kondo N (2014). "Japanese Guideline for Food Allergy 2014". Allergol Int. 63 (3): 399–419. doi:10.2332/allergolint.14-RAI-0770. PMID 25178179.
- Thalayasingam M, Lee BW (2015). "Fish and shellfish allergy". Chem Immunol Allergy. Chemical Immunology and Allergy. 101: 152–61. doi:10.1159/000375508. ISBN 978-3-318-02340-4. PMID 26022875.
- Lopata AL, Jeebhay MF (June 2013). "Airborne seafood allergens as a cause of occupational allergy and asthma". Curr Allergy Asthma Rep. 13 (3): 288–97. doi:10.1007/s11882-013-0347-y. PMID 23575656. S2CID 1276304.
- Jeebhay MF, Robins TG, Lehrer SB, Lopata AL (September 2001). "Occupational seafood allergy: a review". Occup Environ Med. 58 (9): 553–62. doi:10.1136/oem.58.9.553. PMC 1740192. PMID 11511741.
- MedlinePlus Encyclopedia: Food allergy
- Sicherer SH, Sampson HA (2014). "Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment". J Allergy Clin Immunol. 133 (2): 291–307. doi:10.1016/j.jaci.2013.11.020. PMID 24388012.
- Wai CY, Leung NY, Chu KH, Leung PS, Leung AS, Wong GW, Leung TF (March 2020). "Overcoming Shellfish Allergy: How Far Have We Come?". Int J Mol Sci. 21 (6). doi:10.3390/ijms21062234. PMC 7139905. PMID 32210187.
- Prester L (2016). "Seafood Allergy, Toxicity, and Intolerance: A Review". J Am Coll Nutr. 35 (3): 271–83. doi:10.1080/07315724.2015.1014120. PMID 26252073. S2CID 1154235.
- Gelis S, Rueda M, Valero A, Fernández EA, Moran M, Fernández-Caldas E (2020). "Shellfish Allergy: Unmet Needs in Diagnosis and Treatment". J Investig Allergol Clin Immunol. 30 (6): 409–20. doi:10.18176/jiaci.0565. PMID 32694101.
- Lopata AL, Kleine-Tebbe J, Kamath SD (2016). "Allergens and molecular diagnostics of shellfish allergy: Part 22 of the Series Molecular Allergology". Allergo J Int. 25 (7): 210–218. doi:10.1007/s40629-016-0124-2. PMC 5306157. PMID 28239537.
- Pedrosa M, Boyano-Martínez T, García-Ara C, Quirce S (October 2015). "Shellfish Allergy: a Comprehensive Review". Clin Rev Allergy Immunol. 49 (2): 203–16. doi:10.1007/s12016-014-8429-8. PMID 24870065.
- Tong WS, Yuen AW, Wai CY, Leung NY, Chu KH, Leung PS (2018). "Diagnosis of fish and shellfish allergies". J Asthma Allergy. 11: 247–60. doi:10.2147/JAA.S142476. PMC 6181092. PMID 30323632.
- Ruethers T, Taki AC, Johnston EB, Nugraha R, Le TT, Kalic T, McLean TR, Kamath SD, Lopata AL (August 2018). "Seafood allergy: A comprehensive review of fish and shellfish allergens". Mol. Immunol. 100: 28–57. doi:10.1016/j.molimm.2018.04.008. PMID 29858102.
- "Avoiding Cross-Contact". FARE: Food Allergy Research & Education. Retrieved 5 December 2020.
- Morozińska-Gogol J (2019). "Anisakis spp. as etiological agent of zoonotic disease and allergy in European region – an overview". Ann Parasitol. 65 (4): 303–14. doi:10.17420/ap6504.214. PMID 32191412.
- Aibinu IE, Smooker PM, Lopata AL (August 2019). "Anisakis Nematodes in Fish and Shellfish- from infection to allergies". Int J Parasitol Parasites Wildl. 9: 384–93. doi:10.1016/j.ijppaw.2019.04.007. PMC 6626974. PMID 31338296.
- Audicana MT, Kennedy MW (2008). "Anisakis Simplex: From Obscure Infectious Worm to Inducer of Immune Hypersensitivity". Clinical Microbiology Reviews. 21 (2): 360–79. doi:10.1128/CMR.00012-07. PMC 2292572. PMID 18400801.
- Wong L, Tham EH, Lee BW (June 2019). "An update on shellfish allergy". Curr Opin Allergy Clin Immunol. 19 (3): 236–42. doi:10.1097/ACI.0000000000000532. PMID 30893087.
- Wong L, Huang CH, Lee BW (March 2016). "Shellfish and House Dust Mite Allergies: Is the Link Tropomyosin?". Allergy Asthma Immunol Res. 8 (2): 101–6. doi:10.4168/aair.2016.8.2.101. PMC 4713872. PMID 26739402.
- Feldweg AM (2017). "Food-Dependent, Exercise-Induced Anaphylaxis: Diagnosis and Management in the Outpatient Setting". J Allergy Clin Immunol Pract. 5 (2): 283–288. doi:10.1016/j.jaip.2016.11.022. PMID 28283153.
- Pravettoni V, Incorvaia C (2016). "Diagnosis of exercise-induced anaphylaxis: current insights". J Asthma Allergy. 9: 191–198. doi:10.2147/JAA.S109105. PMC 5089823. PMID 27822074.
- Kim CW, Figueroa A, Park CH, Kwak YS, Kim KB, Seo DY, Lee HR (2013). "Combined effects of food and exercise on anaphylaxis". Nutr Res Pract. 7 (5): 347–51. doi:10.4162/nrp.2013.7.5.347. PMC 3796658. PMID 24133612.
- McConnell, Thomas H. (2007). The Nature of Disease: Pathology for the Health Professions. Baltimore, MD: Lippincott Williams & Wilkins. p. 159. ISBN 978-0-7817-5317-3.
- Bøgh KL, Madsen CB (July 2016). "Food Allergens: Is There a Correlation between Stability to Digestion and Allergenicity?". Crit Rev Food Sci Nutr. 56 (9): 1545–67. doi:10.1080/10408398.2013.779569. PMID 25607526.
- Davis PJ, Williams SC (1998). "Protein modification by thermal processing". Allergy. 53 (46 Suppl): 102–5. doi:10.1111/j.1398-9995.1998.tb04975.x. PMID 9826012.
- Verhoeckx KC, Vissers YM, Baumert JL, Faludi R, Feys M, Flanagan S, Herouet-Guicheney C, Holzhauser T, Shimojo R, van der Bolt N, Wichers H, Kimber I (June 2015). "Food processing and allergenicity". Food Chem Toxicol. 80: 223–240. doi:10.1016/j.fct.2015.03.005. PMID 25778347.
- Nester, Eugene W.; Anderson, Denise G.; Roberts Jr, C. Evans; Nester, Martha T. (2009). "Immunologic Disorders". Microbiology: A Human Perspective (6th ed.). New York: McGraw-Hill. pp. 414–428.
- Janeway, Charles; Paul Travers; Mark Walport; Mark Shlomchik (2001). Immunobiology; Fifth Edition. New York and London: Garland Science. pp. e–book. ISBN 978-0-8153-4101-7. Archived from the original on 2009-06-28.
- Grimbaldeston MA, Metz M, Yu M, Tsai M, Galli SJ (2006). "Effector and potential immunoregulatory roles of mast cells in IgE-associated acquired immune responses". Curr. Opin. Immunol. 18 (6): 751–60. doi:10.1016/j.coi.2006.09.011. PMID 17011762.
- Holt PG, Sly PD (2007). "Th2 cytokines in the asthma late-phase response". Lancet. 370 (9596): 1396–8. doi:10.1016/S0140-6736(07)61587-6. PMID 17950849. S2CID 40819814.
- Bergmann MM, Caubet JC, Boguniewicz M, Eigenmann PA (January 2013). "Evaluation of food allergy in patients with atopic dermatitis". J Allergy Clin Immunol Pract. 1 (1): 22–8. doi:10.1016/j.jaip.2012.11.005. PMID 24229818.
- Ho MH, Wong WH, Chang C (June 2014). "Clinical spectrum of food allergies: a comprehensive review". Clin Rev Allergy Immunol. 46 (3): 225–40. doi:10.1007/s12016-012-8339-6. PMID 23229594.
- Faber MA, Pascal M, El Kharbouchi O, Sabato V, Hagendorens MM, Decuyper II, Bridts CH, Ebo DG (June 2017). "Shellfish allergens: tropomyosin and beyond". Allergy. 72 (6): 842–48. doi:10.1111/all.13115. PMID 28027402.
- Nwaru BI, Hickstein L, Panesar SS, Roberts G, Muraro A, Sheikh A (August 2014). "Prevalence of common food allergies in Europe: a systematic review and meta-analysis". Allergy. 69 (8): 992–1007. doi:10.1111/all.12423. PMID 24816523. S2CID 28692645.
- Ferraro V, Zanconato S, Carraro S (May 2019). "Timing of Food Introduction and the Risk of Food Allergy". Nutrients. 11 (5): 1131. doi:10.3390/nu11051131. PMC 6567868. PMID 31117223.
- Perkin MR, Logan K, Tseng A, Raji B, Ayis S, Peacock J, Brough H, Marrs T, Radulovic S, Craven J, Flohr C, Lack G (May 2016). "Randomized Trial of Introduction of Allergenic Foods in Breast-Fed Infants". N Engl J Med. 374 (18): 1733–43. doi:10.1056/NEJMoa1514210. PMID 26943128.
- Tang AW (2003). "A practical guide to anaphylaxis". Am Fam Physician. 68 (7): 1325–1332. PMID 14567487.
- The EAACI Food Allergy and Anaphylaxis Guidelines Group (August 2014). "Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology". Allergy. 69 (8): 1026–45. doi:10.1111/all.12437. PMID 24909803. S2CID 11054771.
- Romantsik, O; Tosca, MA; Zappettini, S; Calevo, MG (20 April 2018). "Oral and sublingual immunotherapy for egg allergy". The Cochrane Database of Systematic Reviews. 4: CD010638. doi:10.1002/14651858.CD010638.pub3. PMC 6494514. PMID 29676439.
- Savage J, Johns CB (February 2015). "Food allergy: epidemiology and natural history". Immunology and Allergy Clinics of North America. 35 (1): 45–59. doi:10.1016/j.iac.2014.09.004. PMC 4254585. PMID 25459576.
- "What is Prevalence?" National Institute of Mental Health (Accessed 25 December 2020).
- Tsabouri S, Triga M, Makris M, Kalogeromitros D, Church MK, Priftis KN (November 2012). "Fish and shellfish allergy in children: review of a persistent food allergy". Pediatr Allergy Immunol. 23 (7): 608–15. doi:10.1111/j.1399-3038.2012.01275.x. PMID 22554093.
- Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, Sigurdardottir ST, Lindner T, Goldhahn K, Dahlstrom J, McBride D, Madsen C (September 2007). "The prevalence of food allergy: a meta-analysis". J. Allergy Clin. Immunol. 120 (3): 638–46. doi:10.1016/j.jaci.2007.05.026. PMID 17628647.
- Tham EH, Shek LP, Van Bever HP, Vichyanond P, Ebisawa M, Wong GW, Lee BW (February 2018). "Early introduction of allergenic foods for the prevention of food allergy from an Asian perspective-An Asia Pacific Association of Pediatric Allergy, Respirology & Immunology (APAPARI) consensus statement". Pediatr Allergy Immunol. 29 (1): 18–27. doi:10.1111/pai.12820. PMID 29068090.
- Lee AJ, Gerez I, Shek LP, Lee BW (March 2012). "Shellfish allergy--an Asia-Pacific perspective". Asian Pac J Allergy Immunol. 30 (1): 3–10. PMID 22523902.
- Moonesinghe H, Mackenzie H, Venter C, Kilburn S, Turner P, Weir K, Dean T (September 2016). "Prevalence of fish and shellfish allergy: A systematic review". Ann Allergy Asthma Immunol. 117 (3): 264–72.e4. doi:10.1016/j.anai.2016.07.015. hdl:10044/1/45844. PMID 27613460.
- Ravid NL, Annunziato RA, Ambrose MA, Chuang K, Mullarkey C, Sicherer SH, Shemesh E, Cox AL (2015). "Mental health and quality-of-life concerns related to the burden of food allergy". Psychiatr. Clin. North Am. 38 (1): 77–89. doi:10.1016/j.psc.2014.11.004. PMID 25725570.
- Morou Z, Tatsioni A, Dimoliatis ID, Papadopoulos NG (2014). "Health-related quality of life in children with food allergy and their parents: a systematic review of the literature". J Investig Allergol Clin Immunol. 24 (6): 382–95. PMID 25668890.
- Lange L (2014). "Quality of life in the setting of anaphylaxis and food allergy". Allergo J Int. 23 (7): 252–260. doi:10.1007/s40629-014-0029-x. PMC 4479473. PMID 26120535.
- van der Velde JL, Dubois AE, Flokstra-de Blok BM (2013). "Food allergy and quality of life: what have we learned?". Curr Allergy Asthma Rep. 13 (6): 651–61. doi:10.1007/s11882-013-0391-7. PMID 24122150. S2CID 326837.
- Culinary Institute of America Allergen-free oasis comes to the CIA (2017)
- Shah E, Pongracic J (2008). "Food-induced anaphylaxis: who, what, why, and where?". Pediatr Ann. 37 (8): 536–41. doi:10.3928/00904481-20080801-06. PMID 18751571.
- "Food Allergen Labeling and Consumer Protection Act of 2004". FDA. August 2, 2004. Archived from the original on 2011-02-02.
- "Food allergen labelling and information requirements under the EU Food Information for Consumers Regulation No. 1169/2011: Technical Guidance" (April 2015).
- FDA (14 December 2017). "Have Food Allergies? Read the Label". Retrieved 14 January 2018.
- "Food Ingredients of Public Health Concern" (PDF). United States Department of Agriculture. Food Safety and Inspection Service. 7 March 2017. Retrieved 16 February 2018.
- "Allergies and Food Safety". United States Department of Agriculture. Food Safety and Inspection Service. 1 December 2016. Retrieved 16 February 2018.
- Allen KJ, Turner PJ, Pawankar R, Taylor S, Sicherer S, Lack G, Rosario N, Ebisawa M, Wong G, Mills EN, Beyer K, Fiocchi A, Sampson HA (2014). "Precautionary labelling of foods for allergen content: are we ready for a global framework?". World Allergy Organ J. 7 (1): 1–14. doi:10.1186/1939-4551-7-10. PMC 4005619. PMID 24791183.
- FDA (18 December 2017). "Food Allergies: What You Need to Know". Retrieved 12 January 2018.
- Roses JB (2011). "Food allergen law and the Food Allergen Labeling and Consumer Protection Act of 2004: falling short of true protection for food allergy sufferers". Food Drug Law J. 66 (2): 225–42, ii. PMID 24505841.
- FDA (18 July 2006). "Food Allergen Labeling And Consumer Protection Act of 2004 Questions and Answers". Retrieved 12 March 2018.
- "Allergy and intolerance: guidance for businesses". Archived from the original on 2014-12-08. Retrieved 2014-12-12.