Guillain–Barré syndrome
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system.[2] Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain often in the back along with muscle weakness, beginning in the feet and hands, often spreading to the arms and upper body.[2] The symptoms may develop over hours to a few weeks.[2] During the acute phase, the disorder can be life-threatening, with about 15 percent of people developing weakness of the breathing muscles and, therefore, requiring mechanical ventilation.[1] Some are affected by changes in the function of the autonomic nervous system, which can lead to dangerous abnormalities in heart rate and blood pressure.[2]
| Guillain–Barré syndrome (GBS) | |
|---|---|
| Other names | Guillain–Barré–Strohl syndrome, Landry's paralysis, postinfectious polyneuritis[1] |
| Pronunciation | |
| Specialty | Neurology |
| Symptoms | Muscle weakness beginning in the feet and hands, usually ascending upward [2] |
| Complications | Breathing difficulties, heart and blood pressure problems[1][2] |
| Usual onset | Rapid (hours to weeks)[2] |
| Causes | Unknown[2] |
| Diagnostic method | Based on symptoms, nerve conduction studies, lumbar puncture[2] |
| Treatment | Supportive care, intravenous immunoglobulin, plasmapheresis |
| Prognosis | Weeks to years for recovery[2] |
| Frequency | 2 per 100,000 people per year[2][3] |
| Deaths | 7.5% of those affected[1] |
Although the cause is unknown, the underlying mechanism involves an autoimmune disorder in which the body's immune system mistakenly attacks the peripheral nerves and damages their myelin insulation.[2] Sometimes this immune dysfunction is triggered by an infection or, less commonly, by surgery, and rarely, by vaccination.[1][2] The diagnosis is usually based on the signs and symptoms through the exclusion of alternative causes and supported by tests such as nerve conduction studies and examination of the cerebrospinal fluid.[2] There are a number of subtypes based on the areas of weakness, results of nerve conduction studies, and the presence of certain antibodies.[4] It is classified as an acute polyneuropathy.[1]
In those with severe weakness, prompt treatment with intravenous immunoglobulins or plasmapheresis, together with supportive care, will lead to good recovery in the majority of people.[2] Recovery may take weeks to years, with about a third having some permanent weakness.[2] Globally, death occurs in approximately 7.5% of those affected.[1] Guillain–Barré syndrome is rare, at one or two cases per 100,000 people every year.[2][3] Both sexes and all parts of the world have similar rates of disease.[1][2]
The syndrome is named after the French neurologists Georges Guillain and Jean Alexandre Barré, who, together with French physician André Strohl, described the condition in 1916.[5][6]
Signs and symptoms
The first symptoms of Guillain–Barré syndrome are numbness, tingling, and pain, alone or in combination. This is followed by weakness of the legs and arms that affects both sides equally and worsens over time.[7][8] The weakness can take half a day to over two weeks to reach maximum severity, and then becomes steady.[8] In one in five people, the weakness continues to progress for as long as four weeks.[4] The muscles of the neck may also be affected, and about half experience involvement of the cranial nerves that supply the head and face; this may lead to weakness of the muscles of the face, swallowing difficulties and sometimes weakness of the eye muscles.[4] In 8%, the weakness affects only the legs (paraplegia or paraparesis).[4] Involvement of the muscles that control the bladder and anus is unusual.[8] In total, about a third of people with Guillain–Barré syndrome continue to be able to walk.[4] Once the weakness has stopped progressing, it persists at a stable level ("plateau phase") before improvement occurs. The plateau phase can take between two days and six months, but the most common duration is a week.[4] Pain-related symptoms affect more than half, and include back pain, painful tingling, muscle pain, and pain in the head and neck relating to irritation of the lining of the brain.[4]
Many people with Guillain–Barré syndrome have experienced the signs and symptoms of an infection in the 3–6 weeks prior to the onset of the neurological symptoms. This may consist of upper respiratory tract infection (rhinitis, sore throat), or diarrhea.[8]
In children, particularly those younger than six years old, the diagnosis can be difficult and the condition is often initially mistaken (sometimes for up to two weeks) for other causes of pains and difficulty walking, such as viral infections,[4] or bone and joint problems.[9]
On neurological examination, characteristic features are the reduced strength of muscles and reduced or absent tendon reflexes (hypo- or areflexia, respectively). However, a small proportion have normal reflexes in affected limbs before developing areflexia, and some may have exaggerated reflexes.[4] In the Miller Fisher variant of Guillain–Barré syndrome (see below), a triad of weakness of the eye muscles, abnormalities in coordination, as well as absent reflexes can be found.[8] The level of consciousness is normally unaffected in Guillain–Barré syndrome, but the Bickerstaff brainstem encephalitis subtype may feature drowsiness, sleepiness, or coma.[5][10]
Respiratory failure
A quarter of all people with Guillain–Barré syndrome develop weakness of the breathing muscles leading to respiratory failure, the inability to breathe adequately to maintain healthy levels of oxygen, and/or carbon dioxide in the blood.[4][8][11] This life-threatening scenario is complicated by other medical problems such as pneumonia, severe infections, blood clots in the lungs, and bleeding in the digestive tract in 60% of those who require artificial ventilation.[8]
Autonomic dysfunction
The autonomic or involuntary nervous system, which is involved in the control of body functions such as heart rate and blood pressure, is affected in two thirds of people with Guillain–Barré syndrome, but the impact is variable.[4] Twenty percent may experience severe blood-pressure fluctuations and irregularities in the heart beat, sometimes to the point that the heart beat stops and requires pacemaker-based treatment.[8] Other associated problems are abnormalities in perspiration and changes in the reactivity of the pupils.[5] Autonomic nervous system involvement can affect even those who do not have severe muscle weakness.[5]
Causes
Infection onset

Two thirds of people with Guillain–Barré syndrome have experienced an infection before the onset of the condition. Most commonly these are episodes of gastroenteritis or a respiratory tract infection. In many cases, the exact nature of the infection can be confirmed.[4] Approximately 30% of cases are provoked by Campylobacter jejuni bacteria, which cause diarrhea. A further 10% are attributable to cytomegalovirus (CMV, HHV-5). Despite this, only very few people with Campylobacter or CMV infections develop Guillain–Barré syndrome (0.25–0.65 per 1000 and 0.6–2.2 per 1000 episodes, respectively).[8] The strain of Campylobacter involved may determine the risk of GBS; different forms of the bacteria have different lipopolysaccharides on their surface, and some may induce illness (see below) while others will not.[4]
Links between other infections and GBS are less certain. Two other herpesviruses (Epstein–Barr virus/HHV-4 and varicella zoster virus/HHV-3) and the bacterium Mycoplasma pneumoniae have been associated with GBS.[8] GBS is known to occur after influenza, and influenza vaccination has been demonstrated to be associated with a reduced risk.[12] The tropical flaviviral infections dengue fever and Zika virus have also been associated with episodes of GBS.[13][14] Previous hepatitis E virus infection has been found to be more common in people with GBS.[4][6]
GBS has also been reported in association with COVID-19, and may be a potential neurological complication of the disease.[15][16][17]
Vaccine onset
An increased incidence of Guillain–Barré syndrome followed influenza immunization that followed the 1976 swine flu outbreak (H1N1 A/NJ/76); 8.8 cases per million (0.0088 per 1000) recipients developed it as a complication.[18] GBS cases occurred in 362 patients during the 6 weeks after influenza vaccination of 45 million persons, an 8.8-fold increase over normal rates.[19] The 1976 swine flu vaccination-induced GBS was an outlier; small increases in incidence have been observed in subsequent vaccination campaigns, but not to the same extent.[18] The 2009 flu pandemic vaccine against pandemic swine flu virus H1N1/PDM09 did not cause a significant increase in cases. In fact, "studies found a small increase of approximately 1 case per million vaccines above the baseline rate, which is similar to that observed after administration of seasonal influenza vaccines over the past several years."[8] The benefits to the population as a whole of vaccination in preventing influenza outweigh the small risks to individuals of that group of GBS after vaccination.[20] Natural influenza infection is a stronger risk factor for the development of GBS than is influenza vaccination and the vaccination reduced the risk of GBS overall by lowering the risk of catching influenza.[21]
In the United States, GBS after seasonal influenza vaccination is listed on the federal government's vaccine injury table,[22] and compensation may be available through the National Vaccine Injury Compensation Program.[23]
Mechanism
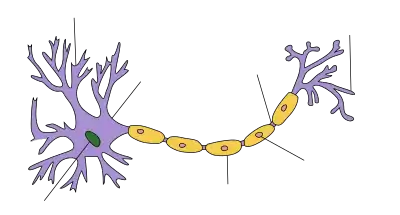
| Neuron |
|---|
The nerve dysfunction in Guillain–Barré syndrome is caused by an immune attack on the nerve cells of the peripheral nervous system and their support structures. The nerve cells have their body (the soma) in the spinal cord and a long projection (the axon) that carries electrical nerve impulses to the neuromuscular junction, where the impulse is transferred to the muscle. Axons are wrapped in a sheath of Schwann cells that contain myelin. Between Schwann cells are gaps (nodes of Ranvier) where the axon is exposed.[8] Different types of Guillain–Barré syndrome feature different types of immune attack. The demyelinating variant (AIDP, see below) features damage to the myelin sheath by white blood cells (T lymphocytes and macrophages); this process is preceded by activation of a group of blood proteins known as complement. In contrast, the axonal variant is mediated by IgG antibodies and complement against the cell membrane covering the axon without direct lymphocyte involvement.[8]
Various antibodies directed at nerve cells have been reported in Guillain–Barré syndrome. In the axonal subtype, these antibodies have been shown to bind to gangliosides, a group of substances found in peripheral nerves. A ganglioside is a molecule consisting of ceramide bound to a small group of hexose-type sugars and containing various numbers of N-acetylneuraminic acid groups. The key four gangliosides against which antibodies have been described are GM1, GD1a, GT1a, and GQ1b, with different anti-ganglioside antibodies being associated with particular features; for instance, GQ1b antibodies have been linked with Miller Fisher variant GBS and related forms including Bickerstaff encephalitis.[8] The production of these antibodies after an infection probably is the result of molecular mimicry, where the immune system is reacting to microbial substances, but the resultant antibodies also react with substances occurring naturally in the body.[8][24] After a Campylobacter infection, the body produces antibodies of the IgA class; only a small proportion of people also produce IgG antibodies against bacterial substance cell wall substances (e.g. lipooligosaccharides) that crossreact with human nerve cell gangliosides. It is not currently known how this process escapes central tolerance to gangliosides, which is meant to suppress the production of antibodies against the body's own substances.[25] Not all antiganglioside antibodies cause disease, and it has recently been suggested that some antibodies bind to more than one type of epitope simultaneously (heterodimeric binding) and that this determines the response. Furthermore, the development of pathogenic antibodies may depend on the presence of other strains of bacteria in the bowel.[25]
Diagnosis
The diagnosis of Guillain–Barré syndrome depends on findings such as rapid development of muscle paralysis, absent reflexes, absence of fever, and absence of a likely cause. Cerebrospinal fluid analysis (through a lumbar spinal puncture) and nerve conduction studies are supportive investigations commonly performed in the diagnosis of GBS.[4][6][8] Testing for antiganglioside antibodies is often performed, but their contribution to diagnosis is usually limited.[4] Blood tests are generally performed to exclude the possibility of another cause for weakness, such as a low level of potassium in the blood.[8] An abnormally low level of sodium in the blood is often encountered in Guillain–Barré syndrome. This has been attributed to the inappropriate secretion of antidiuretic hormone, leading to relative retention of water.[26]
In many cases, magnetic resonance imaging of the spinal cord is performed to distinguish between Guillain–Barré syndrome and other conditions causing limb weakness, such as spinal cord compression.[4][8] If an MRI scan shows enhancement of the nerve roots, this may be indicative of GBS.[4] In children, this feature is present in 95% of scans, but it is not specific to Guillain–Barré syndrome, so other confirmation is also needed.[9]
Spinal fluid
Cerebrospinal fluid envelops the brain and the spine, and lumbar puncture or spinal tap is the removal of a small amount of fluid using a needle inserted between the lumbar vertebrae. Characteristic findings in Guillain–Barré syndrome are an elevated protein level, usually greater than 0.55 g/L, and fewer than 10 white blood cells per cubic millimeter of fluid ("albuminocytological dissociation").[27] This pattern distinguishes Guillain–Barré syndrome from other conditions (such as lymphoma and poliomyelitis) in which both the protein and the cell count are elevated. Elevated CSF protein levels are found in approximately 50% of patients in the first 3 days after onset of weakness, which increases to 80% after the first week.[4]
Repeating the lumbar puncture during the disease course is not recommended. The protein levels may rise after treatment has been administered.[4]
Neurophysiology
Directly assessing nerve conduction of electrical impulses can exclude other causes of acute muscle weakness, as well as distinguish the different types of Guillain–Barré syndrome. Needle electromyography (EMG) and nerve conduction studies may be performed. In the first two weeks, these investigations may not show any abnormality.[4][20] Neurophysiology studies are not required for the diagnosis.[8]
Formal criteria exist for each of the main subtypes of Guillain–Barré syndrome (AIDP and AMAN/AMSAN, see below), but these may misclassify some cases (particularly where there is reversible conduction failure) and therefore changes to these criteria have been proposed.[28] Sometimes, repeated testing may be helpful.[28]
Clinical subtypes
A number of subtypes of Guillain–Barré syndrome are recognized.[4][28] Despite this, many people have overlapping symptoms that can make the classification difficult in individual cases.[5][29] All types have partial forms. For instance, some people experience only isolated eye-movement or coordination problems; these are thought to be a subtype of Miller Fisher syndrome and have similar antiganglioside antibody patterns.[10][29]
| Type[4] | Symptoms | Population affected | Nerve conduction studies | Antiganglioside antibodies |
|---|---|---|---|---|
| Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) | Sensory symptoms and muscle weakness, often with cranial nerve weakness and autonomic involvement | Most common in Europe and North America | Demyelinating polyneuropathy | No clear association |
| Acute motor axonal neuropathy (AMAN) | Isolated muscle weakness without sensory symptoms in less than 10%; cranial nerve involvement uncommon | Rare in Europe and North America, substantial proportion (30-65%) in Asia and Central and South America; sometimes called "Chinese paralytic syndrome" | Axonal polyneuropathy, normal sensory action potential | GM1a/b, GD1a & GalNac-GD1a |
| Acute motor and sensory axonal neuropathy (AMSAN) | Severe muscle weakness similar to AMAN but with sensory loss | - | Axonal polyneuropathy, reduced or absent sensory action potential | GM1, GD1a |
| Pharyngeal-cervical-brachial variant | Weakness particularly of the throat muscles, and face, neck, and shoulder muscles | - | Generally normal, sometimes axonal neuropathy in arms | Mostly GT1a, occasionally GQ1b, rarely GD1a |
| Miller Fisher syndrome | Ataxia, eye muscle weakness, areflexia but usually no limb weakness | This variant occurs more commonly in men than in women (2:1 ratio). Cases typically occur in the spring and the average age of occurrence is 43 years old.[30] | Generally normal, sometimes discrete changes in sensory conduction or H-reflex detected | GQ1b, GT1a |
Other diagnostic entities are often included in the spectrum of Guillain–Barré syndrome. Bickerstaff's brainstem encephalitis (BBE), for instance, is part of the group of conditions now regarded as forms of Miller Fisher syndrome (anti-GQ1b antibody syndrome),[10] as well as a related condition labelled "acute ataxic hypersomnolence" where coordination problems and drowsiness are present but no muscle weakness can be detected.[29] BBE is characterized by the rapid onset of ophthalmoplegia, ataxia, and disturbance of consciousness, and may be associated with absent or decreased tendon reflexes and as well as Babinski's sign.[29] The course of the disease is usually monophasic, but recurrent episodes have been reported. MRI abnormalities in the brainstem have been reported in 11%.[10]
Whether isolated acute sensory loss can be regarded as a form of Guillain–Barré syndrome is a matter of dispute; this is a rare occurrence compared to GBS with muscle weakness but no sensory symptoms.[20]
Treatment
Immunotherapy
Plasmapheresis and intravenous immunoglobulins (IVIG) are the two main immunotherapy treatments for GBS. Plasmapheresis attempts to reduce the body's attack on the nervous system by filtering antibodies out of the bloodstream. Similarly, administration of IVIG neutralizes harmful antibodies and inflammation. These two treatments are equally effective, but a combination of the two is not significantly better than either alone.[31] Plasmapheresis speeds recovery when used within four weeks of the onset of symptoms.[32] IVIG works as well as plasmapheresis when started within two weeks of the onset of symptoms, and has fewer complications.[32] IVIG is usually used first because of its ease of administration and safety. Its use is not without risk; occasionally it causes liver inflammation, or in rare cases, kidney failure.[33] Glucocorticoids alone have not been found to be effective in speeding recovery and could potentially delay recovery.[34]
Respiratory failure
Respiratory failure may require intubation of the trachea and breathing support through mechanical ventilation, generally on an intensive care unit. The need for ventilatory support can be anticipated by measurement of two spirometry-based breathing tests: the forced vital capacity (FVC) and the negative inspiratory force (NIF). An FVC of less than 15 ml per kilogram body weight or an NIF of less than 60 cmH2O are considered markers of severe respiratory failure.[35]
Pain
While pain is common in people with Guillain–Barré syndrome, studies comparing different types of pain medication are insufficient to make a recommendation as to which should be used.[36]
Rehabilitation
Following the acute phase, around 40% of people require intensive rehabilitation with the help of a multidisciplinary team to focus on improving activities of daily living (ADLs).[37] Studies into the subject have been limited, but it is likely that intensive rehabilitation improves long-term symptoms.[38] Teams may include physical therapists, occupational therapists, speech language pathologists, social workers, psychologists, other allied health professionals and nurses. The team usually works under the supervision of a neurologist or rehabilitation physician directing treatment goals.[37]
Physiotherapy interventions include strength, endurance and gait training with graduated increases in mobility, maintenance of posture and alignment as well as joint function. Occupational therapy aims to improve everyday function with domestic and community tasks as well as driving and work. Home modifications, gait aids, orthotics and splints may be provided.[37] Speech-language pathology input may be required in those with speech and swallowing problems, as well as to support communication in those who require ongoing breathing support (often through a tracheostomy). Nutritional support may be provided by the team and by dietitians. Psychologists may provide counseling and support. Psychological interventions may also be required for anxiety, fear and depression.[37]
Prognosis
Guillain–Barré syndrome can lead to death as a result of a number of complications: severe infections, blood clots, and cardiac arrest likely due to autonomic neuropathy. Despite optimum care, this occurs in about 5% of cases.[8]
There is a variation in the rate and extent of recovery.[8] The prognosis of Guillain–Barré syndrome is determined mainly by age (those over 40 may have a poorer outcome), and by the severity of symptoms after two weeks. Furthermore, those who experienced diarrhea before the onset of disease have a worse prognosis.[11] On the nerve conduction study, the presence of conduction block predicts poorer outcome at 6 months.[11] In those who have received intravenous immunoglobulins, a smaller increase in IgG in the blood two weeks after administration is associated with poorer mobility outcomes at six months than those whose IgG level increased substantially.[11] If the disease continues to progress beyond four weeks, or there are multiple fluctuations in the severity (more than two in eight weeks), the diagnosis may be chronic inflammatory demyelinating polyneuropathy, which is treated differently.[4]
In research studies, the outcome from an episode of Guillain–Barré syndrome is recorded on a scale from 0 to 6, where 0 denotes completely healthy; 1 very minor symptoms but able to run; 2 able to walk but not to run; 3 requiring a stick or other support; 4 confined to bed or chair; 5 requiring long-term respiratory support; 6 death.[39]
The health-related quality of life (HRQL) after an attack of Guillain–Barré syndrome can be significantly impaired. About a fifth are unable to walk unaided after six months, and many experience chronic pain, fatigue and difficulty with work, education, hobbies and social activities.[40] HRQL improves significantly in the first year.[40]
Epidemiology
In Western countries, the number of new episodes per year has been estimated to be between 0.89 and 1.89 cases per 100,000 people. Children and young adults are less likely to be affected than the elderly: the risk increases by 20% for every decade of life.[3] Men are more likely to develop Guillain–Barré syndrome than women; the relative risk for men is 1.78 compared to women.[3][8]
The distribution of subtypes varies between countries. In Europe and the United States, 60–80% of people with Guillain–Barré syndrome have the demyelinating subtype (AIDP), and AMAN affects only a small number (6–7%). In Asia and Central and South America, that proportion is significantly higher (30–65%). This may be related to the exposure to different kinds of infection, but also the genetic characteristics of that population.[4] Miller Fisher variant is thought to be more common in Southeast Asia.[8][10]
History

French physician Jean-Baptiste Octave Landry first described the disorder in 1859.[42] In 1916, Georges Guillain, Jean Alexandre Barré, and André Strohl diagnosed two soldiers with the illness and described the key diagnostic abnormality—albuminocytological dissociation—of increased spinal fluid protein concentration but a normal cell count.[5][6][43]
Canadian neurologist C. Miller Fisher described the variant that bears his name in 1956.[10][44] British neurologist Edwin Bickerstaff, based in Birmingham, described the brainstem encephalitis type in 1951 with Philip Cloake, and made further contributions with another paper in 1957.[10][45][46] Guillain had reported on some of these features before their full description in 1938.[10] Further subtypes have been described since then, such as the form featuring pure ataxia and the type causing pharyngeal-cervical-brachial weakness.[10] The axonal subtype was first described in 1986.[47]
Diagnostic criteria were developed in the late 1970s after the series of cases associated with swine flu vaccination. These were refined in 1990.[4][48] The case definition was revised by the Brighton Collaboration for vaccine safety in 2009,[49] but is mainly intended for research.[4] Plasma exchange was first used in 1978, and its benefit was confirmed in larger studies in 1985.[50] Intravenous immunoglobulins were introduced in 1988, and studies in the early 1990s demonstrated that they were no less effective than plasma exchange.[50]
Research directions
The understanding of the disease mechanism of Guillain–Barré syndrome has evolved in recent years.[20] Development of new treatments has been limited since immunotherapy was introduced in the 1980s and 1990s.[20][50] Current research is aimed at demonstrating whether some people who have received IVIg might benefit from a second course if the antibody levels measured in blood after treatment have shown only a small increase.[11][50] Studies of the immunosuppressive drugs mycophenolate mofetil, brain-derived neurotrophic factor and interferon beta (IFN-β) have not demonstrated benefit to support their widespread use.[50]
An animal model (experimental autoimmune neuritis in rats) is often used for studies, and some agents have shown promise: glatiramer acetate, quinpramine, fasudil (an inhibitor of the Rho-kinase enzyme),[20] and the heart drug flecainide.[50] An antibody targeted against the anti-GD3 antiganglioside antibody has shown benefit in laboratory research.[20] Given the role of the complement system in GBS, it has been suggested that complement inhibitors (such as the drug eculizumab) may be effective.[50]
References
- Ferri FF (2016). Ferri's Clinical Advisor 2017: 5 Books in 1. Elsevier Health Sciences. p. 529. ISBN 9780323448383. Archived from the original on 2016-08-21.
- "Guillain–Barré Syndrome Fact Sheet". NIAMS. June 1, 2016. Archived from the original on 5 August 2016. Retrieved 13 August 2016.
- Sejvar JJ, Baughman AL, Wise M, Morgan OW (2011). "Population incidence of Guillain-Barré syndrome: a systematic review and meta-analysis". Neuroepidemiology. 36 (2): 123–33. doi:10.1159/000324710. PMC 5703046. PMID 21422765.
- van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA (August 2014). "Guillain-Barré syndrome: pathogenesis, diagnosis, treatment and prognosis". Nature Reviews. Neurology. 10 (8): 469–82. doi:10.1038/nrneurol.2014.121. PMID 25023340. S2CID 25154778.
- van Doorn PA, Ruts L, Jacobs BC (October 2008). "Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome". The Lancet. Neurology. 7 (10): 939–50. doi:10.1016/S1474-4422(08)70215-1. PMID 18848313. S2CID 9307245.
- Eldar AH, Chapman J (April 2014). "Guillain Barré syndrome and other immune mediated neuropathies: diagnosis and classification". Autoimmunity Reviews. 13 (4–5): 525–30. doi:10.1016/j.autrev.2014.01.033. PMID 24434363.
- Willison HJ, Jacobs BC, van Doorn PA (August 2016). "Guillain-Barré syndrome". Lancet. 388 (10045): 717–27. doi:10.1016/S0140-6736(16)00339-1. PMID 26948435.
- Yuki N, Hartung HP (June 2012). "Guillain-Barré syndrome". The New England Journal of Medicine. 366 (24): 2294–304. doi:10.1056/NEJMra1114525. PMID 22694000.
- Ryan MM (December 2013). "Pediatric Guillain-Barré syndrome". Current Opinion in Pediatrics. 25 (6): 689–93. doi:10.1097/MOP.0b013e328365ad3f. PMID 24240288. S2CID 34011924.
- Shahrizaila N, Yuki N (May 2013). "Bickerstaff brainstem encephalitis and Fisher syndrome: anti-GQ1b antibody syndrome". Journal of Neurology, Neurosurgery, and Psychiatry. 84 (5): 576–83. doi:10.1136/jnnp-2012-302824. PMID 22984203.
- van Doorn PA, Kuitwaard K, Walgaard C, van Koningsveld R, Ruts L, Jacobs BC (May 2010). "IVIG treatment and prognosis in Guillain-Barré syndrome". Journal of Clinical Immunology. 30 Suppl 1: S74-8. doi:10.1007/s10875-010-9407-4. PMC 2883091. PMID 20396937.
- Vellozzi, C.; Iqbal, S.; Broder, K. (15 April 2014). "Guillain-Barre Syndrome, Influenza, and Influenza Vaccination: The Epidemiologic Evidence". Clinical Infectious Diseases. 58 (8): 1149–1155. doi:10.1093/cid/ciu005. PMID 24415636.
- Carod-Artal FJ, Wichmann O, Farrar J, Gascón J (September 2013). "Neurological complications of dengue virus infection". The Lancet. Neurology. 12 (9): 906–919. doi:10.1016/S1474-4422(13)70150-9. PMID 23948177. S2CID 13948773.
- Gatherer D, Kohl A (February 2016). "Zika virus: a previously slow pandemic spreads rapidly through the Americas" (PDF). The Journal of General Virology. 97 (2): 269–273. doi:10.1099/jgv.0.000381. PMID 26684466.
- Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. (September 2020). "Neurological associations of COVID-19". The Lancet. Neurology. 19 (9): 767–783. doi:10.1016/S1474-4422(20)30221-0. PMC 7332267. PMID 32622375.
- Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, et al. (June 2020). "Guillain-Barré Syndrome Associated with SARS-CoV-2". The New England Journal of Medicine. 382 (26): 2574–2576. doi:10.1056/NEJMc2009191. PMC 7182017. PMID 32302082.
- Paterson RW, Brown RL, Benjamin L, Nortley R, Wiethoff S, Bharucha T, et al. (July 2020). "The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings". Brain. 143 (10): 3104–3120. doi:10.1093/brain/awaa240. PMC 7454352. PMID 32637987.
- Lehmann HC, Hartung HP, Kieseier BC, Hughes RA (September 2010). "Guillain-Barré syndrome after exposure to influenza virus". The Lancet. Infectious Diseases. 10 (9): 643–51. doi:10.1016/S1473-3099(10)70140-7. PMID 20797646.
- Nelson, K. E. (2012). "Invited Commentary: Influenza Vaccine and Guillain-Barre Syndrome--Is There a Risk?". American Journal of Epidemiology. 175 (11): 1129–1132. doi:10.1093/aje/kws194. PMID 22582208.
- Rinaldi S (June 2013). "Update on Guillain-Barré syndrome". Journal of the Peripheral Nervous System. 18 (2): 99–112. doi:10.1111/jns5.12020. PMID 23781958. S2CID 23577086.
- DeStefano F, Bodenstab HM, Offit PA (August 2019). "Principal controversies in vaccine safety in the United States". Clinical Infectious Diseases. 69 (4): 726–731. doi:10.1093/cid/ciz135. PMID 30753348.
- "Vaccine Injury Table - HRSA" (PDF). HRSA. March 22, 2017. Retrieved October 23, 2019.
- "National Vaccine Injury Compensation Program". www.hrsa.gov. 11 May 2017. Retrieved 24 October 2019.
- Kuwabara S, Yuki N (December 2013). "Axonal Guillain-Barré syndrome: concepts and controversies". The Lancet. Neurology. 12 (12): 1180–8. doi:10.1016/S1474-4422(13)70215-1. PMID 24229616. S2CID 35101547.
- Willison HJ, Goodyear CS (September 2013). "Glycolipid antigens and autoantibodies in autoimmune neuropathies". Trends in Immunology. 34 (9): 453–9. doi:10.1016/j.it.2013.05.001. PMID 23770405.
- Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al. (March 2014). "Clinical practice guideline on diagnosis and treatment of hyponatraemia". European Journal of Endocrinology. 170 (3): G1-47. doi:10.1530/EJE-13-1020. PMID 24569125.
- Ropper AH (April 1992). "The Guillain-Barré syndrome". The New England Journal of Medicine. 326 (17): 1130–6. doi:10.1056/NEJM199204233261706. PMID 1552914.
- Uncini A, Kuwabara S (August 2012). "Electrodiagnostic criteria for Guillain-Barrè syndrome: a critical revision and the need for an update". Clinical Neurophysiology. 123 (8): 1487–95. doi:10.1016/j.clinph.2012.01.025. PMID 22480600. S2CID 33276521.
- Wakerley BR, Uncini A, Yuki N (September 2014). "Guillain-Barré and Miller Fisher syndromes--new diagnostic classification". Nature Reviews. Neurology. 10 (9): 537–44. doi:10.1038/nrneurol.2014.138. PMID 25072194. S2CID 205515884.
- Mori M, Kuwabara S, Yuki N (January 2012). "Fisher syndrome: clinical features, immunopathogenesis and management". Expert Review of Neurotherapeutics. 12 (1): 39–51. doi:10.1586/ern.11.182. PMID 22149656. S2CID 5597853.
- Hughes RA, Swan AV, van Doorn PA (September 2014). "Intravenous immunoglobulin for Guillain-Barré syndrome". The Cochrane Database of Systematic Reviews. 9 (9): CD002063. doi:10.1002/14651858.CD002063.pub6. PMC 6781841. PMID 25238327.
- Hughes RA, Wijdicks EF, Barohn R, Benson E, Cornblath DR, Hahn AF, et al. (September 2003). "Practice parameter: immunotherapy for Guillain-Barré syndrome: report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 61 (6): 736–40. doi:10.1212/WNL.61.6.736. PMID 14504313.
- Dantal J (October 2013). "Intravenous immunoglobulins: in-depth review of excipients and acute kidney injury risk". American Journal of Nephrology. 38 (4): 275–84. doi:10.1159/000354893. PMID 24051350.
- Hughes, Richard Ac; Brassington, Ruth; Gunn, Angela A.; van Doorn, Pieter A. (2016-10-24). "Corticosteroids for Guillain-Barré syndrome". The Cochrane Database of Systematic Reviews. 10: CD001446. doi:10.1002/14651858.CD001446.pub5. ISSN 1469-493X. PMC 6464149. PMID 27775812.
- Dimachkie MM, Barohn RJ (May 2013). "Guillain-Barré syndrome and variants". Neurologic Clinics. 31 (2): 491–510. doi:10.1016/j.ncl.2013.01.005. PMC 3939842. PMID 23642721.
- Liu, Jia; Wang, Lu-Ning; McNicol, Ewan D. (2015-04-09). "Pharmacological treatment for pain in Guillain-Barré syndrome". The Cochrane Database of Systematic Reviews (4): CD009950. doi:10.1002/14651858.CD009950.pub3. ISSN 1469-493X. PMC 6361619. PMID 25855461.
- Khan F, Amatya B (September 2012). "Rehabilitation interventions in patients with acute demyelinating inflammatory polyneuropathy: a systematic review". European Journal of Physical and Rehabilitation Medicine. 48 (3): 507–22. PMID 22820829. Archived from the original on 2015-08-26.
- Khan F, Ng L, Amatya B, Brand C, Turner-Stokes L (October 2010). "Multidisciplinary care for Guillain-Barré syndrome". The Cochrane Database of Systematic Reviews (10): CD008505. doi:10.1002/14651858.CD008505.pub2. PMID 20927774.
- Hughes RA, Swan AV, Raphaël JC, Annane D, van Koningsveld R, van Doorn PA (September 2007). "Immunotherapy for Guillain-Barré syndrome: a systematic review". Brain. 130 (Pt 9): 2245–57. doi:10.1093/brain/awm004. PMID 17337484. Archived from the original on 2014-10-29.
- Darweesh SK, Polinder S, Mulder MJ, Baena CP, van Leeuwen N, Franco OH, et al. (March 2014). "Health-related quality of life in Guillain-Barré syndrome patients: a systematic review". Journal of the Peripheral Nervous System. 19 (1): 24–35. doi:10.1111/jns5.12051. PMID 24456426. S2CID 6822.
- Goetz CG (May 1998). "Georges Guillain's neurologic exploration of America". Neurology. 50 (5): 1451–5. doi:10.1212/WNL.50.5.1451. PMID 9596004. S2CID 823333.
- Landry J (1859). "Note sur la paralysie ascendante aiguë". Gazette Hebdomadaire de Médecine et de Chirurgie. 6: 472–474, 486–488. Archived from the original on 2017-02-27.
- Guillain G, Barré J, Strohl A (1916). "Sur un syndrome de radiculonévrite avec hyperalbuminose du liquide céphalo-rachidien sans réaction cellulaire. Remarques sur les caractères cliniques et graphiques des réflexes tendineux". Bulletins et Mémoires de la Société des Médecins des Hôpitaux de Paris. 40: 1462–70.
- Fisher M (July 1956). "An unusual variant of acute idiopathic polyneuritis (syndrome of ophthalmoplegia, ataxia and areflexia)". The New England Journal of Medicine. 255 (2): 57–65. doi:10.1056/NEJM195607122550201. PMID 13334797.
- Bickerstaff ER, Cloake PC (July 1951). "Mesencephalitis and rhombencephalitis". British Medical Journal. 2 (4723): 77–81. doi:10.1136/bmj.2.4723.77. PMC 2069534. PMID 14848512.
- Bickerstaff ER (June 1957). "Brain-stem encephalitis; further observations on a grave syndrome with benign prognosis". British Medical Journal. 1 (5032): 1384–7. doi:10.1136/bmj.1.5032.1384. PMC 1973653. PMID 13436795.
- Compston A (2016-07-01). "Recurrent and chronic relapsing Guillain-Barré polyneuritis by P.K. Thomas, R.G. Lascelles, J.F. Hallpike and R.L. Hewer. From the Institute of Neurology and National Hospital, Queen Square, the Royal National Orthopaedic Hospital, and Guy's Hospital, London. Brain 1969; 92: 589–606; with An acute axonal form of Guillain-Barré polyneuropathy by T.E. Feasby, J.J. Gilbert, W.F. Brown, C.F. Bolton, A.F. Hahn, W.F. Koopman and D.W. Zochodne. Brain 1986; 109: 1115–1126". Brain. 139 (7): 2096–2100. doi:10.1093/brain/aww127. ISSN 0006-8950.
- Asbury AK, Cornblath DR (1990). "Assessment of current diagnostic criteria for Guillain-Barré syndrome". Annals of Neurology. 27 Suppl: S21-4. doi:10.1002/ana.410270707. PMID 2194422. S2CID 39483795.
- Sejvar JJ, Kohl KS, Gidudu J, Amato A, Bakshi N, Baxter R, et al. (January 2011). "Guillain-Barré syndrome and Fisher syndrome: case definitions and guidelines for collection, analysis, and presentation of immunization safety data". Vaccine. 29 (3): 599–612. doi:10.1016/j.vaccine.2010.06.003. PMID 20600491.
- Walgaard C, Jacobs BC, van Doorn PA (March 2011). "Emerging drugs for Guillain-Barré syndrome". Expert Opinion on Emerging Drugs. 16 (1): 105–20. doi:10.1517/14728214.2011.531699. PMID 21352072. S2CID 3162151.
Further reading
- Steinberg GJ, Parry JS (2006). Guillain–Barré syndrome: from diagnosis to recovery. New York, N.Y.: Demos; ANN Press (American Academy of Neurology). ISBN 9781932603569.
External links
| Classification | |
|---|---|
| External resources |