Airborne transmission
An airborne transmission is disease transmission through small particulates that can be transmitted through the air over time and distance.[2] Diseases capable of airborne transmission include many of considerable importance both in human and veterinary medicine. The relevant pathogens may be viruses, bacteria, or fungi, and they may be spread through breathing, talking, coughing, sneezing, raising of dust, spraying of liquids, flushing toilets, or any activities which generate aerosol particles or droplets. Human airborne diseases do not include conditions caused by air pollution such as volatile organic compounds (VOCs), gases and any airborne particles.
Airborne transmission is distinct from transmission by respiratory droplets. Respiratory droplets are large enough to fall to the ground rapidly after being produced,[3] as opposed to the smaller particles that carry airborne pathogens. Also, while respiratory droplets consist mostly of water, airborne particles are relatively dry, which damages many pathogens so that their ability to transmit infection is lessened or eliminated. Thus the number of pathogens that can be transmitted through an airborne route is limited.[4][5][6]
Both aerosols and respiratory droplets are part of the respiratory route of transmitting communicable diseases. Individuals generate aerosols and droplets across a wide range of sizes and concentrations, and the amount produced varies widely by person and activity.[7] Larger droplets, greater than 100 μm fall to the ground, and settle within 2 m, except when propelled.[7][3] Smaller particles can carry airborne pathogens for extended periods of time. There is a greater concentration of airborne pathogens within 2m, however they can travel farther and build up in concentration in a room.
The traditional hard size cutoff of 5 μm between airborne and respiratory droplets has been criticized as a false dichotomy not grounded in science, as exhaled particles form a continuum of sizes whose fates depend on environmental conditions in addition to their initial sizes. However, it has informed hospital based transmission based precautions for decades.[7] Recent data on indoor respiratory secretion transfer suggest that droplets/aerosols in the 20 μm size range initially travel with the air flow from cough jets and air conditioning like aerosols but fall out gravitationally at a larger distance.[8] As this size range is most efficiently filtered out in the nasal mucosa,[9] the primordial infection site in Covid-19, aerosols/droplets in this size range may contribute to driving the Covid-19 pandemic.
Overview
Airborne diseases include any that are caused via transmission through the air. Many airborne diseases are of great medical importance. The pathogens transmitted may be any kind of microbe, and they may be spread in aerosols, dust or liquids. The aerosols might be generated from sources of infection such as the bodily secretions of an infected animal or person, or biological wastes such as accumulate in lofts, caves, garbage and the like. Such infected aerosols may stay suspended in air currents long enough to travel for considerable distances; sneezes, for example, can easily project infectious droplets the full length of a bus.[10]
Airborne pathogens or allergens often cause inflammation in the nose, throat, sinuses and the lungs. This is caused by the inhalation of these pathogens that affect a person's respiratory system or even the rest of the body. Sinus congestion, coughing and sore throats are examples of inflammation of the upper respiratory air way due to these airborne agents. Air pollution plays a significant role in airborne diseases which is linked to asthma. Pollutants are said to influence lung function by increasing air way inflammation.[11]
Many common infections can spread by airborne transmission at least in some cases, including but not limited to: COVID-19;[12] measles morbillivirus, chickenpox virus;[4] Mycobacterium tuberculosis, influenza virus, enterovirus, norovirus and less commonly coronavirus, adenovirus, and possibly respiratory syncytial virus.[13] Because the drying process often damages the pathogens, the number of diseases that can be spread through an airborne route is limited.[4]
Airborne diseases can also affect non-humans. For example, Newcastle disease is an avian disease that affects many types of domestic poultry worldwide which is transmitted via airborne contamination.[14] Often, airborne pathogens or allergens cause inflammation in the nose, throat, sinuses, and the upper airway lungs. Upper airway inflammation causes coughing congestion, and sore throat. This is caused by the inhalation of these pathogens that affect a person's respiratory system or even the rest of the body. Sinus congestion, coughing and sore throats are examples of inflammation of the upper respiratory air way due to these airborne agents.
Airborne transmission can be classified into three categories; obligate, preferential, and opportunistic. The first category, obligate airborne infections, are only through aerosols and the most common example of this category is tuberculosis. Preferential airborne infections, such as chicken pox, can be obtained through different routes, but mainly by aerosols. The last category, opportunistic airborne infections, typically transmit through other routes, however under favourable conditions, aerosol transmission can occur. An example of an opportunistic airborne infection includes influenza.[15]
Routes of transmission
Airborne infections usually occur by the respiratory route, with the agent present in aerosols (infectious particles < 5 µm in diameter).[16] This includes dry particles, often the remainders of an evaporated wet particle called nuclei, and wet particles. This kind of infection usually requires independent ventilation during treatment. e.g., tuberculosis.
Relative Humidity (RH)
Relative humidity (RH) plays an important role in the evaporation of droplets and the distance they travel. The 30 μm droplets evaporate in seconds.[17]
The CDC recommends a minimum of 40% RH indoors.[18] Maintaining indoor relative humidity >40% will significantly reduce the infectivity of aerosolized virus. An ideal humidity for preventing aerosol respiratory viral transmission at room temperature appears to be between 40% and 60% RH. If the relative humidity goes below 35% RH, there is more virus in the air.
Transmission
Environmental factors influence the efficacy of airborne disease transmission; the most evident environmental conditions are temperature and relative humidity. The sum of all the factors that influence temperature and humidity, either meteorological (outdoor) or human (indoor), as well as other circumstances influencing the spread of droplets containing infectious particles, as winds, or human behavior, influence the transmission of airborne diseases.
- Rainfall, the number of rainy days[19] being more important than total precipitation;[20][21] mean daily sunshine hours;[22] latitude and altitude[20] are relevant when assessing the possibility of spread of any airborne infection. Some infrequent or exceptional events influence the dissemination of airborne diseases, including tropical storms, hurricanes, typhoons, or monsoons.[23]
Climate determines temperature, winds and relative humidity, the main factors affecting the spread, duration and infectiousness of droplets containing infectious particles. The influenza virus is spread easily in the Northern Hemisphere winter due to climate conditions which favour the infectiousness of the virus.
- After isolated weather events, the concentration of airborne fungal spores is decreased; a few days later, an exponentially increased number of spores is found, compared to normal conditions.[24]
- Socioeconomics has a minor role in airborne disease transmission. In cities, the spread of airborne disease is more rapid than in rural areas and urban outskirts. Rural areas generally favor higher airborne fungal dissemination.[25]
- Proximity to large bodies of water such as rivers and lakes can be a cause of some outbreaks of airborne disease.[23]
- Poor maintenance of air conditioning systems has led to outbreaks of Legionella pneumophila.[26]
- Hospital-acquired airborne diseases are associated with poorly-resourced medical systems, which make isolation challenging.
Prevention
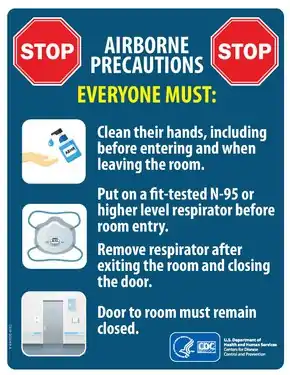
Some ways to prevent airborne diseases include disease-specific immunization, wearing a respirator and limiting time spent in the presence of any patient likely to be a source of infection.[27] Wearing a face mask can also lower the risk of transmission, as it slows down the air flow between individuals.[28] Exposure to a patient or animal with an airborne disease does not guarantee contracting the disease, as infection is dependent on host immune system competency plus the quantity of infectious particles ingested.[27]
Antibiotics may be used in dealing with air-borne bacterial primary infections, such as pneumonic plague.[29]
The United States Centers for Disease Control and Prevention (CDC) advises the public about vaccination and following careful hygiene and sanitation protocols for airborne disease prevention.[30] Many public health specialists recommend physical distancing (also known as social distancing) to reduce the transmission of airborne infections.[31]
A 2011 study concluded that vuvuzelas (a type of air horn popular e.g. with fans at football games) presented a particularly high risk of airborne transmission when their operator has a respiratory infection, as they were spreading a much higher number of aerosol particles than e.g. the act of shouting.[32]
References
- "Transmission-Based Precautions". U.S. Centers for Disease Control and Prevention. 7 January 2016. Retrieved 31 March 2020.
- Siegel JD, Rhinehart E, Jackson M, Chiarello L, Healthcare Infection Control Practices Advisory Committee. "2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings" (PDF). CDC. p. 19. Retrieved 7 February 2019.
Airborne transmission occurs by dissemination of either airborne droplet nuclei or small particles in the respirable size range containing infectious agents that remain infective over time and distance
- Zhang N, Chen W, Chan PT, Yen HL, Tang JW, Li Y (July 2020). "Close contact behavior in indoor environment and transmission of respiratory infection". Indoor Air. 30 (4): 645–661. doi:10.1111/ina.12673. PMID 32259319.
- "FAQ: Methods of Disease Transmission". Mount Sinai Hospital (Toronto). Retrieved 31 March 2020.
- Atkinson J, Chartier Y, Pessoa-Silva CL, Jensen P, Li Y, Seto WH (2009). "Annex C: Respiratory droplets". Natural Ventilation for Infection Control in Health-Care Settings. World Health Organization. ISBN 978-92-4-154785-7.
- Morawska L (October 2006). "Droplet fate in indoor environments, or can we prevent the spread of infection?" (PDF). Indoor Air. 16 (5): 335–47. doi:10.1111/j.1600-0668.2006.00432.x. PMID 16948710.
- Staudt A, Saunders J, Pavlin J, Shelton-Davenport M, et al. (Environmental Health Matters Initiative, National Academies of Sciences, Engineering, and Medicine) (22 October 2020). Shelton-Davenport M, Pavlin J, Saunders J, Staudt A (eds.). Airborne Transmission of SARS-CoV-2: Proceedings of a Workshop in Brief. Washington, D.C.: National Academies Press. doi:10.17226/25958. ISBN 978-0-309-68408-8. PMID 33119244.
- Hunziker P (16 December 2020). "Minimizing exposure to respiratory droplets, 'jet riders' and aerosols in air-conditioned hospital rooms by a 'Shield-and-Sink' strategy". doi:10.1101/2020.12.08.20233056. Cite journal requires
|journal=(help) - Kesavanathan J, Swift DL (January 1998). "Human Nasal Passage Particle Deposition: The Effect of Particle Size, Flow Rate, and Anatomical Factors". Aerosol Science and Technology. 28 (5): 457–463. doi:10.1080/02786829808965537. ISSN 0278-6826.
- https://www.chicagotribune.com/opinion/ct-xpm-2014-04-19-ct-sneeze-germs-edit-20140419-story.html
- "Airborne diseases". Archived from the original on 28 June 2012. Retrieved 21 May 2013.
- "COVID-19: epidemiology, virology and clinical features". GOV.UK. Retrieved 24 October 2020.
- La Rosa G, Fratini M, Della Libera S, Iaconelli M, Muscillo M (1 June 2013). "Viral infections acquired indoors through airborne, droplet or contact transmission". Annali dell'Istituto Superiore di Sanità. 49 (2): 124–32. doi:10.4415/ANN_13_02_03. PMID 23771256.
- Mitchell BW, King DJ (October–December 1994). "Effect of negative air ionization on airborne transmission of Newcastle disease virus". Avian Diseases. 38 (4): 725–32. doi:10.2307/1592107. JSTOR 1592107. PMID 7702504.
- Seto WH (April 2015). "Airborne transmission and precautions: facts and myths". The Journal of Hospital Infection. 89 (4): 225–8. doi:10.1016/j.jhin.2014.11.005. PMID 25578684.
- "Prevention of hospital-acquired infections" (PDF). World Health Organization (WHO).
- Bahl P, Doolan C, de Silva C, Chughtai AA, Bourouiba L, MacIntyre CR (April 2020). "Airborne or droplet precautions for health workers treating COVID-19?". The Journal of Infectious Diseases. doi:10.1093/infdis/jiaa189. PMC 7184471. PMID 32301491.
- Noti JD, Blachere FM, McMillen CM, Lindsley WG, Kashon ML, Slaughter DR, Beezhold DH (2013). "High humidity leads to loss of infectious influenza virus from simulated coughs". PLOS ONE. 8 (2): e57485. Bibcode:2013PLoSO...857485N. doi:10.1371/journal.pone.0057485. PMC 3583861. PMID 23460865.
- Pica N, Bouvier NM (February 2012). "Environmental factors affecting the transmission of respiratory viruses". Current Opinion in Virology. 2 (1): 90–5. doi:10.1016/j.coviro.2011.12.003. PMC 3311988. PMID 22440971.
- Rodríguez-Rajo FJ, Iglesias I, Jato V (April 2005). "Variation assessment of airborne Alternaria and Cladosporium spores at different bioclimatical conditions". Mycological Research. 109 (Pt 4): 497–507. CiteSeerX 10.1.1.487.177. doi:10.1017/s0953756204001777. PMID 15912938.
- Peternel R, Culig J, Hrga I (2004). "Atmospheric concentrations of Cladosporium spp. and Alternaria spp. spores in Zagreb (Croatia) and effects of some meteorological factors". Annals of Agricultural and Environmental Medicine. 11 (2): 303–7. PMID 15627341.
- Sabariego S, Díaz de la Guardia C, Alba F (May 2000). "The effect of meteorological factors on the daily variation of airborne fungal spores in Granada (southern Spain)". International Journal of Biometeorology. 44 (1): 1–5. Bibcode:2000IJBm...44....1S. doi:10.1007/s004840050131. PMID 10879421. S2CID 17834418.
- Hedlund C, Blomstedt Y, Schumann B (2014). "Association of climatic factors with infectious diseases in the Arctic and subarctic region--a systematic review". Global Health Action. 7: 24161. doi:10.3402/gha.v7.24161. PMC 4079933. PMID 24990685.
- Khan NN, Wilson BL (2003). "An environmental assessment of mold concentrations and potential mycotoxin exposures in the greater Southeast Texas area". Journal of Environmental Science and Health. Part A, Toxic/Hazardous Substances & Environmental Engineering. 38 (12): 2759–72. doi:10.1081/ESE-120025829. PMID 14672314. S2CID 6906183.
- Tang JW (December 2009). "The effect of environmental parameters on the survival of airborne infectious agents". Journal of the Royal Society, Interface. 6 Suppl 6: S737-46. doi:10.1098/rsif.2009.0227.focus. PMC 2843949. PMID 19773291.
- "Legionnaire disease". Retrieved 12 April 2015.
- American Academy of Orthopaedic Surgeons (AAOS) (2011). Bloodborne and Airborne Pathogens. Jones & Barlett Publishers. p. 2. ISBN 9781449668273. Retrieved 21 May 2013.
- Clark RP, de Calcina-Goff ML (December 2009). "Some aspects of the airborne transmission of infection". Journal of the Royal Society, Interface. 6 Suppl 6 (suppl_6): S767-82. doi:10.1098/rsif.2009.0236.focus. PMC 2843950. PMID 19815574.
- Ziady LE, Small N (2006). Prevent and Control Infection: Application Made Easy. Juta and Company Ltd. pp. 119–120. ISBN 9780702167904.
- "Redirect - Vaccines: VPD-VAC/VPD menu page". 7 February 2019.
- Glass RJ, Glass LM, Beyeler WE, Min HJ (November 2006). "Targeted social distancing design for pandemic influenza". Emerging Infectious Diseases. 12 (11): 1671–81. doi:10.3201/eid1211.060255. PMC 3372334. PMID 17283616.
- Lai KM, Bottomley C, McNerney R (23 May 2011). "Propagation of respiratory aerosols by the vuvuzela". PLOS ONE. 6 (5): e20086. Bibcode:2011PLoSO...620086L. doi:10.1371/journal.pone.0020086. PMC 3100331. PMID 21629778.