Blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in the large arteries. Blood pressure is usually expressed in terms of the systolic pressure (maximum pressure during one heartbeat) over diastolic pressure (minimum pressure between two heartbeats) in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure.
| Blood pressure | |
|---|---|
 A healthcare worker measuring blood pressure using a sphygmomanometer. | |
| MeSH | D001795 |
| MedlinePlus | 007490 |
| LOINC | 35094-2 |
Blood pressure is one of the vital signs—together with respiratory rate, heart rate, oxygen saturation, and body temperature—that healthcare professionals use in evaluating a patient's health. Normal resting blood pressure, in an adult is approximately 120 millimetres of mercury (16 kPa) systolic over 80 millimetres of mercury (11 kPa) diastolic, denoted as "120/80 mmHg". Globally, the average blood pressure, age standardized, has remained about the same since 1975 to the present, at approx. 127/79 mmHg in men and 122/77 mmHg in women, although these average data mask quite large divergent regional trends.[1]
Traditionally, blood pressure was measured non-invasively using auscultation with either an aneroid gauge, or a mercury-tube sphygmomanometer.[2] Auscultation is still generally considered to be the gold standard of accuracy for non-invasive blood pressure readings in clinic.[3] However, semi-automated methods have become common, largely due to concerns about potential mercury toxicity,[4] although cost, ease of use and applicability to ambulatory blood pressure or home blood pressure measurements have also influenced this trend.[5] Early automated alternatives to mercury-tube sphygmomanometers were often seriously inaccurate, but modern devices validated to international standards achieve an average difference between two standardized reading methods of 5 mm Hg or less, and a standard deviation of less than 8 mm Hg.[5] Most of these semi-automated methods measure blood pressure using oscillometry.[6]
Blood pressure is influenced by cardiac output, systemic vascular resistance and arterial stiffness and varies depending on situation, emotional state, activity, and relative health/disease states. In the short term, blood pressure is regulated by baroreceptors which act via the brain to influence the nervous and the endocrine systems.
Blood pressure that is too low is called hypotension, pressure that is consistently too high is called hypertension, and normal pressure is called normotension.[7] Both hypertension and hypotension have many causes and may be of sudden onset or of long duration. Long-term hypertension is a risk factor for many diseases, including heart disease, stroke and kidney failure. Long-term hypertension is more common than long-term hypotension.
Classification, normal and abnormal values
Systemic arterial pressure
| Category | Systolic BP, mmHg |
Diastolic BP, mmHg |
|---|---|---|
| Optimal | < 120 | < 80 |
| Normal | 120–129 | 80–84 |
| High normal | 130–139 | 85–89 |
| Grade 1 hypertension | 140–159 | 90–99 |
| Grade 2 hypertension | 160–179 | 100–109 |
| Grade 3 hypertension | ≥ 180 | ≥ 110 |
| Isolated systolic hypertensionb | ≥ 140 | < 90 |
| The same classification is used for all ages from 16 years.
a BP category is defined according to seated clinic BP and by the highest level of BP, whether systolic or diastolic. b Isolated systolic hypertension is graded 1, 2, or 3 according to systolic BP values in the ranges indicated. | ||
The risk of cardiovascular disease increases progressively above 115/75 mmHg,[8] below this level there is limited evidence.[9]
Observational studies demonstrate that people who maintain arterial pressures at the low end of these pressure ranges have much better long-term cardiovascular health. There is an ongoing medical debate over what is the optimal level of blood pressure to target when using drugs to lower blood pressure with hypertension, particularly in older people.[10]
The table shows the most recent classification (2018) of office (or clinic) blood pressure by The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH).[11] Similar thresholds had been adopted by the American Heart Association for adults who are 18 years and older,[12] but in November 2017 the American Heart Association announced revised definitions for blood pressure categories that increased the number of people considered to have high blood pressure.[13]
Blood pressure fluctuates from minute to minute and normally shows a circadian rhythm over a 24-hour period,[14] with highest readings in the early morning and evenings and lowest readings at night.[15][16] Loss of the normal fall in blood pressure at night is associated with a greater future risk of cardiovascular disease and there is evidence that night-time blood pressure is a stronger predictor of cardiovascular events than day-time blood pressure.[17] Blood pressure varies over longer time periods (months to years) and this variability predicts adverse outcomes.[18] Blood pressure also changes in response to temperature, noise, emotional stress, consumption of food or liquid, dietary factors, physical activity, changes in posture (such as standing-up), drugs, and disease.[19] The variability in blood pressure and the better predictive value of ambulatory blood pressure measurements has led some authorities, such as the National Institute for Health and Care Excellence (NICE) in the UK, to advocate for the use of ambulatory blood pressure as the preferred method for diagnosis of hypertension.[20]

Various other factors, such as age and sex, also influence a person's blood pressure. Differences between left and right arm blood pressure measurements tend to be small. However, occasionally there is a consistent difference greater than 10 mmHg which may need further investigation, e.g. for peripheral arterial disease or obstructive arterial disease.[21][22][23]
There is no accepted diagnostic standard for hypotension, although pressures less than 90/60 are commonly regarded as hypotensive.[24] In practice blood pressure is considered too low only if symptoms are present.[25]
Fetal blood pressure
In pregnancy, it is the fetal heart and not the mother's heart that builds up the fetal blood pressure to drive blood through the fetal circulation. The blood pressure in the fetal aorta is approximately 30 mmHg at 20 weeks of gestation, and increases to approximately 45 mmHg at 40 weeks of gestation.[26]
The average blood pressure for full-term infants:[27]
- Systolic 65–95 mmHg
- Diastolic 30–60 mmHg
Childhood
| Stage | Approximate age | Systolic BP, mmHg |
Diastolic BP, mmHg |
|---|---|---|---|
| Infants | 0 to 12 months | 75–100 | 50–70 |
| Toddlers and preschoolers | 1 to 5 years | 80–110 | 50–80 |
| School age | 6 to 12 years | 85–120 | 50–80 |
| Adolescents | 13 to 18 years | 95–140 | 60–90 |
In children, the normal ranges for blood pressure are lower than for adults and depend on height.[29] Reference blood pressure values have been developed for children in different countries, based on the distribution of blood pressure in children of these countries.[30]
Aging adults
In adults in most societies, systolic blood pressure tends to rise from early adulthood onward, up to at least age 70;[31][32] diastolic pressure tends to begin to rise at the same time but to start to fall earlier in mid-life, approximately age 55.[32] Mean blood pressure rises from early adulthood, plateauing in mid-life, while pulse pressure rises quite markedly after the age of 40. Consequently, in many older people, systolic blood pressure often exceeds the normal adult range,[32] if the diastolic pressure is in the normal range this is termed isolated systolic hypertension. The rise in pulse pressure with age is attributed to increased stiffness of the arteries.[33] An age-related rise in blood pressure is not considered healthy and is not observed in some isolated unacculturated communities.[34]
Systemic venous pressure
| Site | Normal pressure range (in mmHg)[35] | |
|---|---|---|
| Central venous pressure | 3–8 | |
| Right ventricular pressure | systolic | 15–30 |
| diastolic | 3–8 | |
| Pulmonary artery pressure | systolic | 15–30 |
| diastolic | 4–12 | |
| Pulmonary vein/ |
2–15 | |
| Left ventricular pressure | systolic | 100–140 |
| diastolic | 3–12 | |
Blood pressure generally refers to the arterial pressure in the systemic circulation. However, measurement of pressures in the venous system and the pulmonary vessels plays an important role in intensive care medicine but requires invasive measurement of pressure using a catheter.
Venous pressure is the vascular pressure in a vein or in the atria of the heart. It is much lower than arterial pressure, with common values of 5 mmHg in the right atrium and 8 mmHg in the left atrium.
Variants of venous pressure include:
- Central venous pressure, which is a good approximation of right atrial pressure,[36] which is a major determinant of right ventricular end diastolic volume. (However, there can be exceptions in some cases.)[37]
- The jugular venous pressure (JVP) is the indirectly observed pressure over the venous system. It can be useful in the differentiation of different forms of heart and lung disease.
- The portal venous pressure is the blood pressure in the portal vein. It is normally 5–10 mmHg[38]
Pulmonary pressure
Normally, the pressure in the pulmonary artery is about 15 mmHg at rest.[39]
Increased blood pressure in the capillaries of the lung causes pulmonary hypertension, leading to interstitial edema if the pressure increases to above 20 mmHg, and to pulmonary edema at pressures above 25 mmHg.[40]
Mean systemic pressure
If the heart is stopped, blood pressure falls, but it does not fall to zero. The remaining pressure measured after cessation of the heart beat and redistribution of blood throughout the circulation is termed the mean systemic pressure or mean circulatory filling pressure;[41] typically this is of the order of ~7mm Hg.[41]
Disorders of blood pressure
Disorders of blood pressure control include high blood pressure, low blood pressure, and blood pressure that shows excessive or maladaptive fluctuation.
High blood pressure
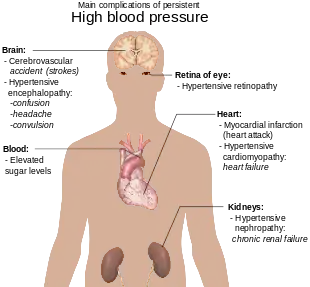
Arterial hypertension can be an indicator of other problems and may have long-term adverse effects. Sometimes it can be an acute problem, for example hypertensive emergency.
Levels of arterial pressure put mechanical stress on the arterial walls. Higher pressures increase heart workload and progression of unhealthy tissue growth (atheroma) that develops within the walls of arteries. The higher the pressure, the more stress that is present and the more atheroma tend to progress and the heart muscle tends to thicken, enlarge and become weaker over time.
Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure, and arterial aneurysms, and is the leading cause of chronic kidney failure. Even moderate elevation of arterial pressure leads to shortened life expectancy. At severely high pressures, mean arterial pressures 50% or more above average, a person can expect to live no more than a few years unless appropriately treated.[42]
In the past, most attention was paid to diastolic pressure; but nowadays it is recognized that both high systolic pressure and high pulse pressure (the numerical difference between systolic and diastolic pressures) are also risk factors. In some cases, it appears that a decrease in excessive diastolic pressure can actually increase risk, due probably to the increased difference between systolic and diastolic pressures (see the article on pulse pressure). If systolic blood pressure is elevated (>140 mmHg) with a normal diastolic blood pressure (<90 mmHg), it is called "isolated systolic hypertension" and may present a health concern.[43][44]
For those with heart valve regurgitation, a change in its severity may be associated with a change in diastolic pressure. In a study of people with heart valve regurgitation that compared measurements two weeks apart for each person, there was an increased severity of aortic and mitral regurgitation when diastolic blood pressure increased, whereas when diastolic blood pressure decreased, there was a decreased severity.[45]
Low blood pressure
Blood pressure that is too low is known as hypotension. This is a medical concern if it causes signs or symptoms, such as dizziness, fainting, or in extreme cases, circulatory shock.[46]
Causes of low arterial pressure include:[47]
- Sepsis
- Hemorrhage – blood loss
- Cardiogenic shock
- Neurally mediated hypotension (or reflex syncope)
- Toxins including toxic doses of blood pressure medicine
- Hormonal abnormalities, such as Addison's disease
- Eating disorders, particularly anorexia nervosa and bulimia
Orthostatic hypotension
A large fall in blood pressure upon standing (persistent systolic/diastolic blood pressure decrease of >20/10 mm Hg) is termed orthostatic hypotension (postural hypotension) and represents a failure of the body to compensate for the effect of gravity on the circulation. Standing results in an increased hydrostatic pressure in the blood vessels of the lower limbs. The consequent distension of the veins below the diaphragm (venous pooling) causes ~500 ml of blood to be relocated from the chest and upper body. This results in a rapid decrease in central blood volume and a reduction of ventricular preload which in turn reduces stroke volume, and mean arterial pressure. Normally this is compensated for by multiple mechanisms, including activation of the autonomic nervous system which increases heart rate, myocardial contractility and systemic arterial vasoconstriction to preserve blood pressure and elicits venous vasoconstriction to decrease venous compliance. Decreased venous compliance also results from an intrinsic myogenic increase in venous smooth muscle tone in response to the elevated pressure in the veins of the lower body. Other compensatory mechanisms include the veno-arteriolar axon reflex, the 'skeletal muscle pump' and 'respiratory pump'. Together these mechanisms normally stabilize blood pressure within a minute or less.[48] If these compensatory mechanisms fail and arterial pressure and blood flow decrease beyond a certain point, the perfusion of the brain becomes critically compromised (i.e., the blood supply is not sufficient), causing lightheadedness, dizziness, weakness or fainting.[49] Usually this failure of compensation is due to disease, or drugs that affect the sympathetic nervous system.[48] A similar effect is observed following the experience of excessive gravitational forces (G-loading), such as routinely experienced by aerobatic or combat pilots 'pulling Gs' where the extreme hydrostatic pressures exceed the ability of the body's compensatory mechanisms.
Variable or fluctuating blood pressure
Some fluctuation or variation in blood pressure is normal. Variations in pressure that are significantly greater than the norm are associated with increased risk of cardiovascular disease[50] brain small vessel disease,[51] and dementia[52] independent of the average blood pressure level. Recent evidence from clinical trials has also linked variation in blood pressure to stroke,[53] heart failure,[54] and cardiac changes that may give rise to heart failure.[55] These data have prompted discussion of whether excessive variation in blood pressure should be treated, even among normotensive older adults.[56] Older individuals and those who had received blood pressure medications are more likely to exhibit larger fluctuations in pressure,[57] and there is some evidence that different antihypertensive agents have different effects on blood pressure variability;[52] whether these differences translate to benefits in outcome is uncertain.[52]
Physiology
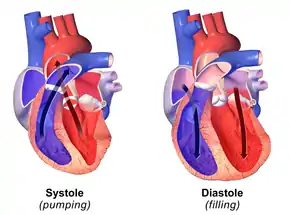
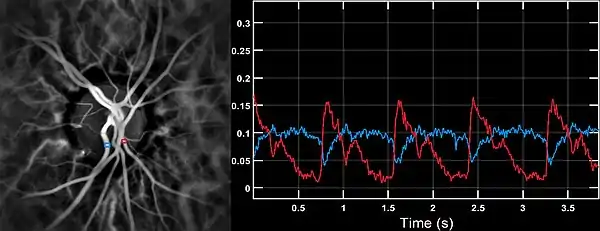
During each heartbeat, blood pressure varies between a maximum (systolic) and a minimum (diastolic) pressure.[58] The blood pressure in the circulation is principally due to the pumping action of the heart.[59] However, blood pressure is also regulated by neural regulation from the brain (see Hypertension and the Brain), as well as osmotic regulation from the kidney. Differences in mean blood pressure drive the flow of blood around the circulation. The rate of mean blood flow depends on both blood pressure and the resistance to flow presented by the blood vessels. In the absence of hydrostatic effects (e.g. standing), mean blood pressure decreases as the circulating blood moves away from the heart through arteries and capillaries due to viscous losses of energy. Mean blood pressure drops over the whole circulation, although most of the fall occurs along the small arteries and arterioles.[60] Pulsatility also diminishes in the smaller elements of the arterial circulation, although some transmitted pulsatility is observed in capillaries.[61]

Gravity affects blood pressure via hydrostatic forces (e.g., during standing), and valves in veins, breathing, and pumping from contraction of skeletal muscles also influence blood pressure, particularly in veins.[59]
Hemodynamics
A simple view of the hemodynamics of systemic arterial pressure is based around mean arterial pressure (MAP) and pulse pressure. Most influences on blood pressure can be understood in terms of their effect on cardiac output,[62] systemic vascular resistance, or arterial stiffness (the inverse of arterial compliance). Cardiac output is the product of stroke volume and heart rate. Stroke volume is influenced by 1) the end diastolic volume or filling pressure of the ventricle acting via the Frank Starling mechanism - this is influenced by blood volume ; 2) cardiac contractility; and 3) afterload, the impedance to blood flow presented by the circulation.[63] In the short-term, the greater the blood volume, the higher the cardiac output. This has been proposed as an explanation of the relationship between high dietary salt intake and increased blood pressure; however, responses to increased dietary sodium intake vary between individuals and are highly dependent on autonomic nervous system responses and the renin–angiotensin system,[64][65][66] changes in plasma osmolarity may also be important.[67] In the longer-term the relationship between volume and blood pressure is more complex.[68] In simple terms systemic vascular resistance is mainly determined by the caliber of small arteries and arterioles. The resistance attributable to a blood vessel depends on its radius as described by the Hagen-Poiseuille's equation (resistance∝1/radius4). Hence, the smaller the radius, the higher the resistance. Other physical factors that affect resistance include: vessel length (the longer the vessel, the higher the resistance), blood viscosity (the higher the viscosity, the higher the resistance)[69] and the number of vessels, particularly the smaller numerous, arterioles and capillaries. The presence of a severe arterial stenosis increases resistance to flow, however this increase in resistance rarely increases systemic blood pressure because its contribution to total systemic resistance is small, although it may profoundly decrease downstream flow.[70] Substances called vasoconstrictors reduce the caliber of blood vessels, thereby increasing blood pressure. Vasodilators (such as nitroglycerin) increase the caliber of blood vessels, thereby decreasing arterial pressure. In the longer term a process termed remodeling also contributes to changing the caliber of small blood vessels and influencing resistance and reactivity to vasoactive agents.[71][72] Reductions in capillary density, termed capillary rarefaction, may also contribute to increased resistance in some circumstances.[73]
In practice, each individual's autonomic nervous system and other systems regulating blood pressure, notably the kidney,[74] respond to and regulate all these factors so that, although the above issues are important, they rarely act in isolation and the actual arterial pressure response of a given individual can vary widely in the short and long term.
Mean arterial pressure
MAP is the average of blood pressure over a cardiac cycle and is determined by the cardiac output (CO), systemic vascular resistance (SVR), and central venous pressure (CVP)):[75][76][77]
In practice, the contribution of CVP (which is small) is generally ignored and so
MAP is often estimated from measurements of the systolic pressure, and the diastolic pressure, [77] using the equation:
where k = 0.333 although other values for k have been advocated.[78][79]
Pulse pressure

The pulse pressure is the difference between the measured systolic and diastolic pressures,[80]
The pulse pressure is a consequence of the pulsatile nature of the cardiac output, i.e. the heartbeat. The magnitude of the pulse pressure is usually attributed to the interaction of the stroke volume of the heart, the compliance (ability to expand) of the arterial system—largely attributable to the aorta and large elastic arteries—and the resistance to flow in the arterial tree.[80]
Regulation of blood pressure
The endogenous, homeostatic regulation of arterial pressure is not completely understood, but the following mechanisms of regulating arterial pressure have been well-characterized:
- Baroreceptor reflex: Baroreceptors in the high pressure receptor zones detect changes in arterial pressure. These baroreceptors send signals ultimately to the medulla of the brain stem, specifically to the rostral ventrolateral medulla (RVLM). The medulla, by way of the autonomic nervous system, adjusts the mean arterial pressure by altering both the force and speed of the heart's contractions, as well as the systemic vascular resistance. The most important arterial baroreceptors are located in the left and right carotid sinuses and in the aortic arch.[81]
- Renin–angiotensin system (RAS): This system is generally known for its long-term adjustment of arterial pressure. This system allows the kidney to compensate for loss in blood volume or drops in arterial pressure by activating an endogenous vasoconstrictor known as angiotensin II.
- Aldosterone release: This steroid hormone is released from the adrenal cortex in response to angiotensin II or high serum potassium levels. Aldosterone stimulates sodium retention and potassium excretion by the kidneys. Since sodium is the main ion that determines the amount of fluid in the blood vessels by osmosis, aldosterone will increase fluid retention, and indirectly, arterial pressure.
- Baroreceptors in low pressure receptor zones (mainly in the venae cavae and the pulmonary veins, and in the atria) result in feedback by regulating the secretion of antidiuretic hormone (ADH/Vasopressin), renin and aldosterone. The resultant increase in blood volume results in an increased cardiac output by the Frank–Starling law of the heart, in turn increasing arterial blood pressure.
These different mechanisms are not necessarily independent of each other, as indicated by the link between the RAS and aldosterone release. When blood pressure falls many physiological cascades commence in order to return the blood pressure to a more appropriate level.
- The blood pressure fall is detected by a decrease in blood flow and thus a decrease in glomerular filtration rate (GFR).
- Decrease in GFR is sensed as a decrease in Na+ levels by the macula densa.
- The macula densa causes an increase in Na+ reabsorption, which causes water to follow in via osmosis and leads to an ultimate increase in plasma volume. Further, the macula densa releases adenosine which causes constriction of the afferent arterioles.
- At the same time, the juxtaglomerular cells sense the decrease in blood pressure and release renin.
- Renin converts angiotensinogen (inactive form) to angiotensin I (active form).
- Angiotensin I flows in the bloodstream until it reaches the capillaries of the lungs where angiotensin converting enzyme (ACE) acts on it to convert it into angiotensin II.
- Angiotensin II is a vasoconstrictor that will increase blood flow to the heart and subsequently the preload, ultimately increasing the cardiac output.
- Angiotensin II also causes an increase in the release of aldosterone from the adrenal glands.
- Aldosterone further increases the Na+ and H2O reabsorption in the distal convoluted tubule of the nephron.
Currently, the RAS is targeted pharmacologically by ACE inhibitors and angiotensin II receptor antagonists, also known as angiotensin receptor blockers (ARBs). The aldosterone system is directly targeted by spironolactone, an aldosterone antagonist. The fluid retention may be targeted by diuretics; the antihypertensive effect of diuretics is due to its effect on blood volume. Generally, the baroreceptor reflex is not targeted in hypertension because if blocked, individuals may suffer from orthostatic hypotension and fainting.

Measurement

Arterial pressure is most commonly measured via a sphygmomanometer, which uses the height of a column of mercury, or an aneroid gauge, to reflect the blood pressure by auscultation.[2] The most common automated blood pressure measurement technique is based on the oscillometric method.[82] Fully automated oscillometric measurement has been available since 1981.[83] This principle has recently been used to measure blood pressure with a smartphone.[84] Measuring pressure invasively, by penetrating the arterial wall to take the measurement, is much less common and usually restricted to a hospital setting. Novel methods to measure blood pressure without penetrating the arterial wall, and without applying any pressure on patient's body are currently being explored.[85] So-called cuffless measurements, these methods open the door to more comfortable and acceptable blood pressure monitors. An example is a cuffless blood pressure monitor at the wrist that uses only optical sensors[86]
Blood pressure in other animals
Blood pressure in non-human mammals is similar to human blood pressure. In contrast, heart rate differs markedly, largely depending on the size of the animal (larger animals have slower heart rates).[87] As in humans, blood pressure in animals differs by age, sex, time of day and circumstances:[88][89] measurements made in laboratories or under anesthesia may not be representative of values under free-living conditions. Rats, mice, dogs and rabbits have been used extensively to study the causes of high blood pressure.[90]
| Species | Blood pressure mm Hg |
Heart rate beats per minute | |
|---|---|---|---|
| Systolic | Diastolic | ||
| Calves | 140 | 70 | 75–146 |
| Cats | 155 | 68 | 100–259 |
| Dogs | 161 | 51 | 62–170 |
| Goats | 140 | 90 | 80–120 |
| Guinea-pigs | 140 | 90 | 240–300 |
| Mice | 120 | 75 | 580–680 |
| Pigs | 169 | 55 | 74–116 |
| Rabbits | 118 | 67 | 205–306 |
| Rats | 153 | 51 | 305–500 |
| Rhesus monkeys | 160 | 125 | 180–210 |
| Sheep | 140 | 80 | 63–210 |
Hypertension in cats and dogs
Hypertension in cats and dogs is generally diagnosed if the blood pressure is greater than 160 mm Hg (systolic), however sight hounds have higher blood pressures than most other breeds so a blood pressure >180mmHg is considered abnormal in these dogs.[91]
References
- NCD Risk Factor Collaboration (NCD-RisC) (January 2017). "Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants". The Lancet. 389 (10064): 37–55. doi:10.1016/S0140-6736(16)31919-5. PMC 5220163. PMID 27863813.
- Booth J (November 1977). "A short history of blood pressure measurement". Proceedings of the Royal Society of Medicine. 70 (11): 793–9. doi:10.1177/003591577707001112. PMC 1543468. PMID 341169.
- Grim CE, Grim CM (March 2016). "Auscultatory BP: still the gold standard". Journal of the American Society of Hypertension. 10 (3): 191–3. doi:10.1016/j.jash.2016.01.004. PMID 26839183.
- O'Brien E (January 2001). "Blood pressure measurement is changing!". Heart. 85 (1): 3–5. doi:10.1136/heart.85.1.3. PMC 1729570. PMID 11119446.
- Ogedegbe G, Pickering T (November 2010). "Principles and techniques of blood pressure measurement". Cardiology Clinics. 28 (4): 571–86. doi:10.1016/j.ccl.2010.07.006. PMC 3639494. PMID 20937442.
- Alpert BS, Quinn D, Gallick D (December 2014). "Oscillometric blood pressure: a review for clinicians". Journal of the American Society of Hypertension. 8 (12): 930–8. doi:10.1016/j.jash.2014.08.014. PMID 25492837.
- William Alexander Newman, ed. (2012). Dorland's illustrated medical dictionary (32nd ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-6257-8. OCLC 706780870.
- Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM (February 2006). "Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association". Hypertension. 47 (2): 296–308. CiteSeerX 10.1.1.617.6244. doi:10.1161/01.HYP.0000202568.01167.B6. PMID 16434724. S2CID 1447853.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (December 2002). "Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies". Lancet. 360 (9349): 1903–13. doi:10.1016/S0140-6736(02)11911-8. PMID 12493255.
- Yusuf S, Lonn E (November 2016). "The SPRINT and the HOPE-3 Trial in the Context of Other Blood Pressure-Lowering Trials". JAMA Cardiology. 1 (8): 857–858. doi:10.1001/jamacardio.2016.2169. PMID 27602555.
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. (September 2018). "2018 ESC/ESH Guidelines for the management of arterial hypertension". European Heart Journal. 39 (33): 3021–3104. doi:10.1093/eurheartj/ehy339. PMID 30165516.
- "Understanding blood pressure readings". American Heart Association. 11 January 2011. Retrieved 30 March 2011.
- "Nearly half of US adults could now be classified with high blood pressure, under new definitions". American Heart Association. 13 November 2017. Retrieved 2019-07-28.
- Smolensky MH, Hermida RC, Portaluppi F (June 2017). "Circadian mechanisms of 24-hour blood pressure regulation and patterning". Sleep Medicine Reviews. 33: 4–16. doi:10.1016/j.smrv.2016.02.003. PMID 27076261.
- van Berge-Landry HM, Bovbjerg DH, James GD (October 2008). "Relationship between waking-sleep blood pressure and catecholamine changes in African-American and European-American women". Blood Pressure Monitoring. 13 (5): 257–62. doi:10.1097/MBP.0b013e3283078f45. PMC 2655229. PMID 18799950.
Table2: Comparison of ambulatory blood pressures and urinary norepinephrine and epinephrine excretion measured at work, home, and during sleep between European–American (n = 110) and African–American (n = 51) women
- van Berge-Landry HM, Bovbjerg DH, James GD (October 2008). "Relationship between waking-sleep blood pressure and catecholamine changes in African-American and European-American women". Blood Pressure Monitoring. 13 (5): 257–62. doi:10.1097/MBP.0b013e3283078f45. PMC 2655229. PMID 18799950. NIHMS90092.
- Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA (January 2011). "Predictive role of the nighttime blood pressure". Hypertension. 57 (1): 3–10. doi:10.1161/HYPERTENSIONAHA.109.133900. PMID 21079049.
- Rothwell PM (June 2011). "Does blood pressure variability modulate cardiovascular risk?". Current Hypertension Reports. 13 (3): 177–86. doi:10.1007/s11906-011-0201-3. PMID 21465141. S2CID 207331784.
- H.), Schmidt, T. F. H. (Thomas F. (1992). Temporal Variations of the Cardiovascular System. Engel, Bernard T., Blümchen, Gerhard. Berlin, Heidelberg: Springer Berlin Heidelberg. ISBN 9783662027486. OCLC 851391490.
- National Clinical Guideline Centre (UK) (2011). Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34. National Institute for Health and Clinical Excellence: Guidance. London: Royal College of Physicians (UK). PMID 22855971.
- Eguchi K, Yacoub M, Jhalani J, Gerin W, Schwartz JE, Pickering TG (February 2007). "Consistency of blood pressure differences between the left and right arms". Arch Intern Med. 167 (4): 388–93. doi:10.1001/archinte.167.4.388. PMID 17325301.
- Agarwal R, Bunaye Z, Bekele DM (March 2008). "Prognostic significance of between-arm blood pressure differences". Hypertension. 51 (3): 657–62. CiteSeerX 10.1.1.540.5836. doi:10.1161/HYPERTENSIONAHA.107.104943. PMID 18212263. S2CID 1101762.
- Clark, C. E.; Campbell, J. L.; Evans, P. H.; Millward, A. (December 2006). "Prevalence and clinical implications of the inter-arm blood pressure difference: A systematic review". Journal of Human Hypertension. 20 (12): 923–931. doi:10.1038/sj.jhh.1002093. ISSN 0950-9240. PMID 17036043.
- Sharma S, Bhattacharya PT (2018). Hypotension. StatPearls. StatPearls Publishing. PMID 29763136. Retrieved 2018-12-23.
- Mayo Clinic staff (2009-05-23). "Low blood pressure (hypotension) – Causes". MayoClinic.com. Mayo Foundation for Medical Education and Research. Retrieved 2010-10-19.
- Struijk PC, Mathews VJ, Loupas T, Stewart PA, Clark EB, Steegers EA, Wladimiroff JW (October 2008). "Blood pressure estimation in the human fetal descending aorta". Ultrasound Obstet Gynecol. 32 (5): 673–81. doi:10.1002/uog.6137. PMID 18816497.
- Sharon SM, Emily SM (2006). Foundations of Maternal-Newborn Nursing (4th ed.). Philadelphia: Elsevier. p. 476.
- Pediatric Age Specific, p. 6. Revised 6/10. By Theresa Kirkpatrick and Kateri Tobias. UCLA Health System
- National Heart Lung and Blood Institute. "Blood pressure tables for children and adolescents". Archived from the original on 2014-06-18. Retrieved 2008-09-23. (Note that the median blood pressure is given by the 50th percentile and hypertension is defined by the 95th percentile for a given age, height, and sex.)
- Chiolero A (Mar 2014). "The quest for blood pressure reference values in children". Journal of Hypertension. 32 (3): 477–79. doi:10.1097/HJH.0000000000000109. PMID 24477093. S2CID 1949314.
- Wills AK, Lawlor DA, Matthews FE, Sayer AA, Bakra E, Ben-Shlomo Y, Benzeval M, Brunner E, Cooper R, Kivimaki M, Kuh D, Muniz-Terrera G, Hardy R (June 2011). "Life course trajectories of systolic blood pressure using longitudinal data from eight UK cohorts". PLOS Medicine. 8 (6): e1000440. doi:10.1371/journal.pmed.1000440. PMC 3114857. PMID 21695075.
- Franklin SS, Gustin W, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D (July 1997). "Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study". Circulation. 96 (1): 308–15. doi:10.1161/01.CIR.96.1.308. PMID 9236450. S2CID 40209177.
- Franklin SS (2008-05-01). "Beyond blood pressure: Arterial stiffness as a new biomarker of cardiovascular disease". Journal of the American Society of Hypertension. 2 (3): 140–51. doi:10.1016/j.jash.2007.09.002. PMID 20409896.
- Gurven, Michael; Blackwell, Aaron D.; Rodríguez, Daniel Eid; Stieglitz, Jonathan; Kaplan, Hillard (July 2012). "Does blood pressure inevitably rise with age?: longitudinal evidence among forager-horticulturalists". Hypertension. 60 (1): 25–33. doi:10.1161/HYPERTENSIONAHA.111.189100. ISSN 1524-4563. PMC 3392307. PMID 22700319.
- Table 30-1 in: Trudie A Goers; Washington University School of Medicine Department of Surgery; Klingensmith, Mary E; Li Ern Chen; Sean C Glasgow (2008). The Washington manual of surgery. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 0-7817-7447-0.CS1 maint: multiple names: authors list (link)
- "Central Venous Catheter Physiology". Archived from the original on 2008-08-21. Retrieved 2009-02-27.
- Tkachenko BI, Evlakhov VI, Poyasov IZ (2002). "Independence of changes in right atrial pressure and central venous pressure". Bull. Exp. Biol. Med. 134 (4): 318–20. doi:10.1023/A:1021931508946. PMID 12533747. S2CID 23726657.
- "Esophageal Varices : Article Excerpt by: Samy A Azer". eMedicine. Retrieved 2011-08-22.
- What Is Pulmonary Hypertension? From Diseases and Conditions Index (DCI). National Heart, Lung, and Blood Institute. Last updated September 2008. Retrieved on 6 April 2009.
- Chapter 41, p. 210 in: Cardiology secrets By Olivia Vynn Adair Edition: 2, illustrated Published by Elsevier Health Sciences, 2001 ISBN 1-56053-420-6, 978-1-56053-420-4
- Rothe, C. F. (1993). "Mean circulatory filling pressure: its meaning and measurement". Journal of Applied Physiology. 74 (2): 499–509. doi:10.1152/jappl.1993.74.2.499. ISSN 8750-7587. PMID 8458763.
- Textbook of Medical Physiology, 7th Ed., Guyton & Hall, Elsevier-Saunders, ISBN 0-7216-0240-1, p. 220.
- "Isolated systolic hypertension: A health concern?". MayoClinic.com. Retrieved 2018-01-25.
- "Clinical Management of Isolated Systolic Hypertension". Archived from the original on September 29, 2011. Retrieved 2011-12-07.
- Gottdiener JS, Panza JA, St John Sutton M, Bannon P, Kushner H, Weissman NJ (July 2002). "Testing the test: The reliability of echocardiography in the sequential assessment of valvular regurgitation". American Heart Journal. 144 (1): 115–21. doi:10.1067/mhj.2002.123139. PMID 12094197.
- "Diseases and conditions index – hypotension". National Heart Lung and Blood Institute. September 2008. Retrieved 2008-09-16.
- Braunwald, Eugene; Bonow, Robert O. (2012). Braunwald's heart disease : a textbook of cardiovascular medicine (9th ed.). Philadelphia: Saunders. ISBN 9781437703986. OCLC 671465395.
- Ricci, Fabrizio; De Caterina, Raffaele; Fedorowski, Artur (2015-08-18). "Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment". Journal of the American College of Cardiology. 66 (7): 848–860. doi:10.1016/j.jacc.2015.06.1084. ISSN 0735-1097. PMID 26271068.
- Franco Folino A (2007). "Cerebral autoregulation and syncope". Prog Cardiovasc Dis. 50 (1): 49–80. doi:10.1016/j.pcad.2007.01.001. PMID 17631437.
- Stevens, Sarah L.; Wood, Sally; Koshiaris, Constantinos; Law, Kathryn; Glasziou, Paul; Stevens, Richard J.; McManus, Richard J. (2016-08-09). "Blood pressure variability and cardiovascular disease: systematic review and meta-analysis". BMJ (Clinical Research Ed.). 354: i4098. doi:10.1136/bmj.i4098. ISSN 1756-1833. PMC 4979357. PMID 27511067.
- Tully, Phillip J.; Yano, Yuichiro; Launer, Lenore J.; Kario, Kazuomi; Nagai, Michiaki; Mooijaart, Simon P.; Claassen, Jurgen A. H. R.; Lattanzi, Simona; Vincent, Andrew D.; Tzourio, Christophe; Variability in Blood Pressure and Brain Health Consortium † (2020-01-07). "Association Between Blood Pressure Variability and Cerebral Small-Vessel Disease: A Systematic Review and Meta-Analysis". Journal of the American Heart Association. 9 (1): e013841. doi:10.1161/JAHA.119.013841. ISSN 2047-9980. PMC 6988154. PMID 31870233.
- Messerli, Franz H.; Hofstetter, Louis; Rimoldi, Stefano F.; Rexhaj, Emrush; Bangalore, Sripal (2019-05-28). "Risk Factor Variability and Cardiovascular Outcome: JACC Review Topic of the Week". Journal of the American College of Cardiology. 73 (20): 2596–2603. doi:10.1016/j.jacc.2019.02.063. ISSN 0735-1097. PMID 31118154.
- Muntner, P (2015). "Visit-to-visit variability of blood pressure and coronary heart disease, stroke, heart failure and mortality: A cohort study". Annals of Internal Medicine. 163 (5): 329–338. doi:10.7326/M14-2803. PMC 5021508. PMID 26215765.
- Nuyujukian, DS; Koska, J; Bahn, G; Reaven, PD; Zhou, JJ (2020). "Blood pressure variability and risk of heart failure in ACCORD and the VADT". Diabetes Care. 43 (7): 1471–1478. doi:10.2337/dc19-2540. hdl:10150/641980. PMC 7305004. PMID 32327422.
- Nwabuo, CC (2020). "Association Between Visit-to-Visit Blood Pressure Variability in Early Adulthood and Myocardial Structure and Function in Later Life". JAMA Cardiology. 5 (7): 795. doi:10.1001/jamacardio.2020.0799. PMC 7160747. PMID 32293640.
- Parati, Gianfranco; Ochoa, Juan E.; Lombardi, Carolina; Bilo, Grzegorz (March 2013). "Assessment and management of blood-pressure variability". Nature Reviews. Cardiology. 10 (3): 143–155. doi:10.1038/nrcardio.2013.1. ISSN 1759-5010. PMID 23399972. S2CID 22425558.
- Brickman AM, Reitz C, Luchsinger JA, Manly JJ, Schupf N, Muraskin J, DeCarli C, Brown TR, Mayeux R (2010). "Long-term Blood Pressure Fluctuation and Cerebrovascular Disease in an Elderly Cohort". Archives of Neurology. 67 (5): 564–69. doi:10.1001/archneurol.2010.70. PMC 2917204. PMID 20457955.
- "Normal Blood Pressure Range Adults". Health and Life. 2010-06-07. Archived from the original on 2016-03-18. Retrieved 2010-06-20.
- Caro CG (1978). The Mechanics of The Circulation. Oxford [Oxfordshire]: Oxford University Press. ISBN 978-0-19-263323-1.
- Klabunde, Richard (2005). Cardiovascular Physiology Concepts. Lippincott Williams & Wilkins. pp. 93–94. ISBN 978-0-7817-5030-1.
- Mahler, F.; Muheim, M. H.; Intaglietta, M.; Bollinger, A.; Anliker, M. (1979). "Blood pressure fluctuations in human nailfold capillaries". The American Journal of Physiology. 236 (6): H888–893. doi:10.1152/ajpheart.1979.236.6.H888. ISSN 0002-9513. PMID 443454.
- Guyton AC (December 1981). "The relationship of cardiac output and arterial pressure control". Circulation. 64 (6): 1079–88. doi:10.1161/01.cir.64.6.1079. PMID 6794930.
- Milnor, W. R. (May 1975). "Arterial impedance as ventricular afterload". Circulation Research. 36 (5): 565–570. doi:10.1161/01.res.36.5.565. ISSN 0009-7330. PMID 1122568.
- Freis ED (April 1976). "Salt, volume and the prevention of hypertension". Circulation. 53 (4): 589–95. doi:10.1161/01.CIR.53.4.589. PMID 767020.
- Caplea A, Seachrist D, Dunphy G, Ely D (April 2001). "Sodium-induced rise in blood pressure is suppressed by androgen receptor blockade". American Journal of Physiology. Heart and Circulatory Physiology. 4. 280 (4): H1793–801. doi:10.1152/ajpheart.2001.280.4.H1793. PMID 11247793. S2CID 12069178.
- Houston MC (January 1986). "Sodium and hypertension. A review". Archives of Internal Medicine. 1. 146 (1): 179–85. doi:10.1001/archinte.1986.00360130217028. PMID 3510595.
- Kanbay, Mehmet; Aslan, Gamze; Afsar, Baris; Dagel, Tuncay; Siriopol, Dimitrie; Kuwabara, Masanari; Incir, Said; Camkiran, Volkan; Rodriguez-Iturbe, Bernardo; Lanaspa, Miguel A.; Covic, Adrian (October 2018). "Acute effects of salt on blood pressure are mediated by serum osmolality". Journal of Clinical Hypertension (Greenwich, Conn.). 20 (10): 1447–1454. doi:10.1111/jch.13374. ISSN 1751-7176. PMID 30232829.
- Titze, Jens; Luft, Friedrich C. (2017). "Speculations on salt and the genesis of arterial hypertension". Kidney International. 91 (6): 1324–1335. doi:10.1016/j.kint.2017.02.034. ISSN 1523-1755. PMID 28501304.
- Lee AJ (December 1997). "The role of rheological and haemostatic factors in hypertension". Journal of Human Hypertension. 11 (12): 767–76. doi:10.1038/sj.jhh.1000556. PMID 9468002.
- Coffman JD (December 1988). "Pathophysiology of obstructive arterial disease". Herz. 13 (6): 343–50. PMID 3061915.
- Korner, P. I.; Angus, J. A. (1992). "Structural determinants of vascular resistance properties in hypertension. Haemodynamic and model analysis". Journal of Vascular Research. 29 (4): 293–312. doi:10.1159/000158945. ISSN 1018-1172. PMID 1391553.
- Mulvany, Michael J. (2012). "Small artery remodelling in hypertension". Basic & Clinical Pharmacology & Toxicology. 110 (1): 49–55. doi:10.1111/j.1742-7843.2011.00758.x. ISSN 1742-7843. PMID 21733124.
- de Moraes, Roger; Tibirica, Eduardo (2017). "Early Functional and Structural Microvascular Changes in Hypertension Related to Aging". Current Hypertension Reviews. 13 (1): 24–32. doi:10.2174/1573402113666170413095508. ISSN 1875-6506. PMID 28412915.
- Norman, Roger A.; Manning, R. Davis; Scheel, Konrad W.; Cowley, Allen W.; Coleman, Thomas G.; Guyton, Arthur C. (1972-05-01). "Arterial pressure regulation: Overriding dominance of the kidneys in long-term regulation and in hypertension". The American Journal of Medicine. 52 (5): 584–594. doi:10.1016/0002-9343(72)90050-2. ISSN 1555-7162. PMID 4337474.
- Mayet, J; Hughes, A (2003). "Cardiac and vascular pathophysiology in hypertension". Heart. 89 (9): 1104–9. doi:10.1136/heart.89.9.1104. ISSN 1355-6037. PMC 1767863. PMID 12923045.
- Granger, Joey P.; Hall, John E. (2007). "Role of the Kidney in Hypertension". Comprehensive Hypertension. Elsevier. pp. 241–263. doi:10.1016/b978-0-323-03961-1.50026-x. ISBN 978-0-323-03961-1.
- Klabunde RE (2007). "Cardiovascular Physiology Concepts – Mean Arterial Pressure". Archived from the original on 2009-10-02. Retrieved 2008-09-29.
- Bos, Willem J. W.; Verrij, Elisabeth; Vincent, Hieronymus H.; Westerhof, Berend E.; Parati, Gianfranco; van Montfrans, Gert A. (April 2007). "How to assess mean blood pressure properly at the brachial artery level". Journal of Hypertension. 25 (4): 751–755. doi:10.1097/HJH.0b013e32803fb621. ISSN 0263-6352. PMID 17351365. S2CID 23155959.
- Meaney, E.; Alva, F.; Moguel, R.; Meaney, A.; Alva, J.; Webel, R. (July 2000). "Formula and nomogram for the sphygmomanometric calculation of the mean arterial pressure". Heart (British Cardiac Society). 84 (1): 64. doi:10.1136/heart.84.1.64. ISSN 1468-201X. PMC 1729401. PMID 10862592.
- Klabunde RE (2007). "Cardiovascular Physiology Concepts – Pulse Pressure". Archived from the original on 2009-10-18. Retrieved 2008-10-02.
- Klabunde, RE (2007). "Cardiovascular Physiology Concepts – Arterial Baroreceptors". Retrieved 2008-09-09. Archived version 2009-10-03
- Forouzanfar M, Dajani HR, Groza VZ, Bolic M, Rajan S, Batkin I (2015-01-01). "Oscillometric Blood Pressure Estimation: Past, Present, and Future". IEEE Reviews in Biomedical Engineering. 8: 44–63. doi:10.1109/RBME.2015.2434215. PMID 25993705. S2CID 8940215.
- Google patents: Donald Nunn—Apparatus and method for measuring blood pressure
- Chandrasekhar A, Kim CS, Naji M, Natarajan K, Hahn JO, Mukkamala R (March 2018). "Smartphone-based blood pressure monitoring via the oscillometric finger-pressing method". Science Translational Medicine. 10 (431): eaap8674. doi:10.1126/scitranslmed.aap8674. PMC 6039119. PMID 29515001.
- Solà, Josep; Delgado-Gonzalo, Ricard (2019). The Handbook of Cuffless Blood Pressure Monitoring. Springer International Publishing. ISBN 978-3-030-24701-0.
- Sola J, Bertschi M, Krauss J (September 2018). "Measuring Pressure: Introducing oBPM, the Optical Revolution for Blood Pressure Monitoring". IEEE Pulse. 9 (5): 31–33. doi:10.1109/MPUL.2018.2856960. PMID 30273141. S2CID 52893219.
- Prothero JW (2015-10-22). The design of mammals : a scaling approach. Cambridge. ISBN 9781107110472. OCLC 907295832.
- Gross DR (2009). Animal models in cardiovascular research (3rd ed.). Dordrecht: Springer. p. 5. ISBN 9780387959627. OCLC 432709394.
- Brown S, Atkins C, Bagley R, Carr A, Cowgill L, Davidson M, Egner B, Elliott J, Henik R, Labato M, Littman M, Polzin D, Ross L, Snyder P, Stepien R (2007). "Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats". Journal of Veterinary Internal Medicine. 21 (3): 542–58. doi:10.1111/j.1939-1676.2007.tb03005.x. PMID 17552466.
- Lerman LO, Chade AR, Sica V, Napoli C (September 2005). "Animal models of hypertension: an overview". The Journal of Laboratory and Clinical Medicine. 146 (3): 160–73. doi:10.1016/j.lab.2005.05.005. PMID 16131455.
- Acierno, Mark J.; Brown, Scott; Coleman, Amanda E.; Jepson, Rosanne E.; Papich, Mark; Stepien, Rebecca L.; Syme, Harriet M. (2018). "ACVIM consensus statement: Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats". Journal of Veterinary Internal Medicine. 32 (6): 1803–1822. doi:10.1111/jvim.15331. ISSN 0891-6640. PMC 6271319. PMID 30353952.
Further reading
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ (2005). Subcommittee of Professional Public Education of the American Heart Association Council on High Blood Pressure Research. "Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research". Hypertension. 45 (5): 142–61. doi:10.1161/01.HYP.0000150859.47929.8e. PMID 15611362.
External links
| Wikimedia Commons has media related to Blood pressure. |