Cholecystitis
Cholecystitis is inflammation of the gallbladder.[8] Symptoms include right upper abdominal pain, nausea, vomiting, and occasionally fever.[1] Often gallbladder attacks (biliary colic) precede acute cholecystitis.[1] The pain lasts longer in cholecystitis than in a typical gallbladder attack.[1] Without appropriate treatment, recurrent episodes of cholecystitis are common.[1] Complications of acute cholecystitis include gallstone pancreatitis, common bile duct stones, or inflammation of the common bile duct.[1][8]
| Cholecystitis | |
|---|---|
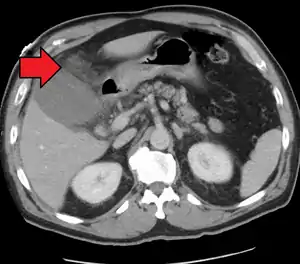 | |
| Acute cholecystitis as seen on CT. Note the fat stranding around the enlarged gallbladder. | |
| Specialty | General surgery, gastroenterology |
| Symptoms | Right upper abdominal pain, nausea, vomiting, fever[1] |
| Duration | Short term or long term[2] |
| Causes | Gallstones, severe illness[1][3] |
| Risk factors | Birth control pills, pregnancy, family history, obesity, diabetes, liver disease, rapid weight loss[4] |
| Diagnostic method | Abdominal ultrasound[5] |
| Differential diagnosis | Hepatitis, peptic ulcer disease, pancreatitis, pneumonia, angina[6] |
| Treatment | Gallbladder removal surgery, gallbladder drainage[7][5] |
| Prognosis | Generally good with treatment[4] |
More than 90% of the time acute cholecystitis is from blockage of the cystic duct by a gallstone.[1] Risk factors for gallstones include birth control pills, pregnancy, a family history of gallstones, obesity, diabetes, liver disease, or rapid weight loss.[4] Occasionally, acute cholecystitis occurs as a result of vasculitis or chemotherapy, or during recovery from major trauma or burns.[9] Cholecystitis is suspected based on symptoms and laboratory testing.[5] Abdominal ultrasound is then typically used to confirm the diagnosis.[5]
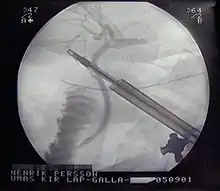
Treatment is usually with laparoscopic gallbladder removal, within 24 hours if possible.[7][10] Taking pictures of the bile ducts during the surgery is recommended.[7] The routine use of antibiotics is controversial.[5][11] They are recommended if surgery cannot occur in a timely manner or if the case is complicated.[5] Stones in the common bile duct can be removed before surgery by endoscopic retrograde cholangiopancreatography (ERCP) or during surgery.[7] Complications from surgery are rare.[4] In people unable to have surgery, gallbladder drainage may be tried.[5]
About 10–15% of adults in the developed world have gallstones.[5] Women more commonly have stones than men and they occur more commonly after age 40.[4] Certain ethnic groups are more often affected; for example, 48% of American Indians have gallstones.[4] Of all people with stones, 1–4% have biliary colic each year.[5] If untreated, about 20% of people with biliary colic develop acute cholecystitis.[5] Once the gallbladder is removed outcomes are generally good.[4] Without treatment, chronic cholecystitis may occur.[2] The word is from Greek, cholecyst- meaning "gallbladder" and -itis meaning "inflammation".[12]
Signs and symptoms

Most people with gallstones do not have symptoms.[1] However, when a gallstone temporarily lodges in the cystic duct, they experience biliary colic.[1] Biliary colic is abdominal pain in the right upper quadrant or epigastric region. It is episodic, occurring after eating greasy or fatty foods, and leads to nausea and/or vomiting.[13] People who suffer from cholecystitis most commonly have symptoms of biliary colic before developing cholecystitis. The pain becomes more severe and constant in cholecystitis. Nausea is common and vomiting occurs in 75% of people with cholecystitis.[14] In addition to abdominal pain, right shoulder pain can be present.[13]
On physical examination, fever is common.[14] A gallbladder with cholecystitis is almost always tender to touch.[13] Because of the inflammation, its size can be felt from the outside of the body in 25–50% of people with cholecystitis.[13] Pain with deep inspiration leading to termination of the breath while pressing on the right upper quadrant of the abdomen usually causes pain (Murphy's sign).[15] Yellowing of the skin (jaundice) may occur but is often mild. Severe jaundice suggests another cause of symptoms such as choledocholithiasis.[14] People who are old, have diabetes, chronic illness, or who are immunocompromised may have vague symptoms that may not include fever or localized tenderness.[16]
Complications
A number of complications may occur from cholecystitis if not detected early or properly treated. Signs of complications include high fever, shock and jaundice. Complications include the following:[13]
- Gangrene
- Gallbladder rupture
- Empyema
- Fistula formation and gallstone ileus
- Rokitansky-Aschoff sinuses
Gangrene and gallbladder rupture
Cholecystitis causes the gallbladder to become distended and firm. Distension can lead to decreased blood flow to the gallbladder, causing tissue death and eventually gangrene.[13] Once tissue has died, the gallbladder is at greatly increased risk of rupture (perforation). Rupture can also occur in cases of chronic cholecystitis.[13] Rupture is a rare but serious complication that leads to abscess formation or peritonitis.[14] Massive rupture of the gallbladder has a mortality rate of 30%.[13]
Empyema
Untreated cholecystitis can lead to worsened inflammation and infected bile that can lead to a collection of pus surrounding the gallbladder, also known as empyema.[13] The symptoms of empyema are similar to uncomplicated cholecystitis but greater severity: high fever, severe abdominal pain, more severely elevated white blood count.[13]
Fistula formation and gallstone ileus
The inflammation of cholecystitis can lead to adhesions between the gallbladder and other parts of the gastrointestinal tract, most commonly the duodenum.[13] These adhesions can lead to the formation of direct connections between the gallbladder and gastrointestinal tract, called fistulas.[13] With these direct connections, gallstones can pass from the gallbladder to the intestines. Gallstones can get trapped in the gastrointestinal tract, most commonly at the connection between the small and large intestines (ileocecal valve). When a gallstone gets trapped, it can lead to an intestinal obstruction, called gallstone ileus, leading to abdominal pain, vomiting, constipation, and abdominal distension.[13]
Causes
Cholecystitis occurs when the gallbladder becomes inflamed.[13] Gallstones are the most common cause of gallbladder inflammation but it can also occur due to blockage from a tumor or scarring of the bile duct.[13][17] The greatest risk factor for cholecystitis is gallstones.[17] Risk factors for gallstones include female sex, increasing age, pregnancy, oral contraceptives, obesity, diabetes mellitus, ethnicity (Native North American), rapid weight loss.[13]
Acute calculous cholecystitis
Gallstones blocking the flow of bile account for 90% of cases of cholecystitis (acute calculous cholecystitis).[1][14] Blockage of bile flow leads to thickening and buildup of bile causing an enlarged, red, and tense gallbladder.[1] The gallbladder is initially sterile but often becomes infected by bacteria, predominantly E. coli, Klebsiella, Streptococcus, and Clostridium species.[13] Inflammation can spread to the outer covering of the gallbladder and surrounding structures such as the diaphragm, causing referred right shoulder pain.[13]
Acalculous cholecystitis
In acalculous cholecystitis, no stone is in the biliary ducts.[13] It accounts for 5–10% of all cases of cholecystitis and is associated with high morbidity and mortality rates.[13] Acalculous cholecystitis is typically seen in people who are hospitalized and critically ill.[13] Males are more likely to develop acute cholecystitis following surgery in the absence of trauma.[14][18] It is associated with many causes including vasculitis, chemotherapy, major trauma or burns.[9]
The presentation of acalculous cholecystitis is similar to calculous cholecystitis.[19][13] Patients are more likely to have yellowing of the skin (jaundice) than in calculous cholecystitis.[20] Ultrasonography or computed tomography often shows an immobile, enlarged gallbladder.[13] Treatment involves immediate antibiotics and cholecystectomy within 24–72 hours.[20]
Chronic cholecystitis
Chronic cholecystitis occurs after repeated episodes of acute cholecystitis and is almost always due to gallstones.[13] Chronic cholecystitis may be asymptomatic, may present as a more severe case of acute cholecystitis, or may lead to a number of complications such as gangrene, perforation, or fistula formation.[13][14]
Xanthogranulomatous cholecystitis (XGC) is a rare form of chronic cholecystitis which mimics gallbladder cancer although it is not cancerous.[21][22] It was first reported in the medical literature in 1976 by McCoy and colleagues.[21][23]
Mechanism
Blockage of the cystic duct by a gallstone causes a buildup of bile in the gallbladder and increased pressure within the gallbladder. Concentrated bile, pressure, and sometimes bacterial infection irritate and damage the gallbladder wall, causing inflammation and swelling of the gallbladder.[1] Inflammation and swelling of the gallbladder can reduce normal blood flow to areas of the gallbladder, which can lead to cell death due to inadequate oxygen.[13]
Diagnosis
The diagnosis of cholecystitis is suggested by the history (abdominal pain, nausea, vomiting, fever) and physical examinations in addition to laboratory and ultrasonographic testing. Boas's sign, which is pain in the area below the right scapula, can be a symptom of acute cholecystitis.[24]
Blood tests
In someone suspected of having cholecystitis, blood tests are performed for markers of inflammation (e.g. complete blood count, C-reactive protein), as well as bilirubin levels in order to assess for bile duct blockage.[14] Complete blood count typically shows an increased white blood count (12,000–15,000/mcL).[14] C-reactive protein is usually elevated although not commonly measured in the United States.[1] Bilirubin levels are often mildly elevated (1–4 mg/dL).[14] If bilirubin levels are more significantly elevated, alternate or additional diagnoses should be considered such as gallstone blocking the common bile duct (common bile duct stone).[1] Less commonly, blood aminotransferases are elevated.[13] The degree of elevation of these laboratory values may depend on the degree of inflammation of the gallbladder.
Imaging
Right upper quadrant abdominal ultrasound is most commonly used to diagnose cholecystitis.[1][25][26] Ultrasound findings suggestive of acute cholecystitis include gallstones, pericholecystic fluid (fluid surrounding the gallbladder), gallbladder wall thickening (wall thickness over 3 mm),[27] dilation of the bile duct, and sonographic Murphy's sign.[13] Given its higher sensitivity, hepatic iminodiacetic acid (HIDA) scan can be used if ultrasound is not diagnostic.[13][14] CT scan may also be used if complications such as perforation or gangrene are suspected.[14]
 Abdominal ultrasonography showing gallstones, wall thickening and fluid around the gall bladder
Abdominal ultrasonography showing gallstones, wall thickening and fluid around the gall bladder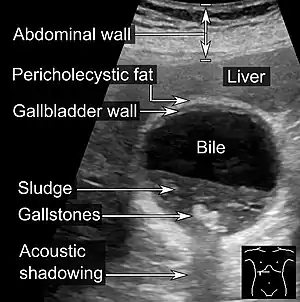 Gallstones and biliary sludge, but the gallbladder wall is not clearly thickened, with no edema in the pericholecystic fat, thus not cholecystitis.
Gallstones and biliary sludge, but the gallbladder wall is not clearly thickened, with no edema in the pericholecystic fat, thus not cholecystitis. Acute cholecystitis as seen on ultrasound. The closed arrow points to gallbladder wall thickening. Open arrow points to stones in the GB
Acute cholecystitis as seen on ultrasound. The closed arrow points to gallbladder wall thickening. Open arrow points to stones in the GB Acute cholecystitis with gallbladder wall thickening, a large gallstone, and a large gallbladder
Acute cholecystitis with gallbladder wall thickening, a large gallstone, and a large gallbladder
Histopathology
Histopathology is indicated if preoperative imaging and/or gross examination gives a suspicion of gallbladder cancer.[29]
 Gross examination of gallbladder carcinoma, with a prominent nodule.
Gross examination of gallbladder carcinoma, with a prominent nodule.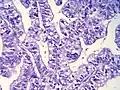 Histopathology of gallbladder carcinoma, with marked nuclear pleomorphism.
Histopathology of gallbladder carcinoma, with marked nuclear pleomorphism.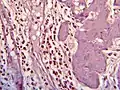 Histopathology of eosinophilic cholecystitis
Histopathology of eosinophilic cholecystitis Gross examination of gallbladder cholesterolosis, with yellow streaks of cholesterol deposition.
Gross examination of gallbladder cholesterolosis, with yellow streaks of cholesterol deposition.
Differential diagnosis
Many other diagnoses can have similar symptoms as cholecystitis. Additionally the symptoms of chronic cholecystitis are commonly vague and can be mistaken for other diseases. These alternative diagnoses include but are not limited to:[14]
- Perforated peptic ulcer
- Acute pancreatitis
- Liver abscess
- Pneumonia
- Myocardial ischemia
- Hiatal hernia
- Biliary colic
- Choledocholithiasis
- Cholangitis
- Appendicitis
- Colitis
- Acute peptic ulcer exacerbation
- Amoebic liver abscess
- Acute intestinal obstruction
- Kidney stone
- Biliary ascariasis[30]
Treatment
Surgery
For most people with acute cholecystitis, the treatment of choice is surgical removal of the gallbladder, laparoscopic cholecystectomy.[31] Laparoscopic cholecystectomy is performed using several small incisions located at various points across the abdomen. Several studies have demonstrated the superiority of laparoscopic cholecystectomy when compared to open cholecystectomy (using a large incision in the right upper abdomen under the rib cage). People undergoing laparoscopic surgery report less incisional pain postoperatively as well as having fewer long term complications and less disability following the surgery.[32][33] Additionally, laparoscopic surgery is associated with a lower rate of surgical site infection.[34]
During the days prior to laparoscopic surgery, studies showed that outcomes were better following early removal of the gallbladder, preferably within the first week.[35] Early laparoscopic cholecystectomy (within 7 days of visiting a doctor with symptoms) as compared to delayed treatment (more than 6 weeks) may result in shorter hospital stays and a decreased risk of requiring an emergency procedure.[36] There is no difference in terms of negative outcomes including bile duct injury or conversion to open cholecystectomy.[36] For early cholecystectomy, the most common reason for conversion to open surgery is inflammation that hides Calot's triangle. For delayed surgery, the most common reason was fibrotic adhesions.[36]
Other

Supportive measures may be instituted prior to surgery. These measures include fluid resuscitation. Intravenous opioids can be used for pain control.
Antibiotics are often not needed.[38] If used they should target enteric organisms (e.g. Enterobacteriaceae), such as E. coli and Bacteroides. This may consist of a broad spectrum antibiotic; such as piperacillin-tazobactam, ampicillin-sulbactam, ticarcillin-clavulanate (Timentin), a third generation cephalosporin (e.g.ceftriaxone) or a quinolone antibiotic (such as ciprofloxacin) and anaerobic bacteria coverage, such as metronidazole. For penicillin allergic people, aztreonam or a quinolone with metronidazole may be used.
In cases of severe inflammation, shock, or if the person has higher risk for general anesthesia (required for cholecystectomy), an interventional radiologist may insert a percutaneous drainage catheter into the gallbladder (percutaneous cholecystostomy tube) and treat the person with antibiotics until the acute inflammation resolves. A cholecystectomy may then be warranted if the person's condition improves.
Homeopathic approaches to treating cholecystitis have not been validated by evidence and should not be used in place of surgery.
Epidemiology
Cholecystitis accounts for 3–10% of cases of abdominal pain worldwide.[39] Cholecystitis caused an estimated 651,829 emergency department visits and 389,180 hospital admissions in the US in 2012.[40] The 2012 US mortality rate was 0.7 per 100,000 people.[40] The frequency of cholecystitis is highest in people age 50–69 years old.[39]
References
- Strasberg, SM (26 June 2008). "Clinical practice. Acute calculous cholecystitis". The New England Journal of Medicine. 358 (26): 2804–11. doi:10.1056/nejmcp0800929. PMID 18579815.
- Feldman, Mark (2010). Sleisenger & Fordtran's Gastrointestinal and liver disease pathophysiology, diagnosis, management (9 ed.). [S.l.]: MD Consult. p. 1065. ISBN 9781437727678. Archived from the original on 2017-09-08.
- Levy, Angela D.; Mortele, Koenraad J.; Yeh, Benjamin M. (2015). Gastrointestinal Imaging. Oxford University Press. p. 456. ISBN 9780199392148. Archived from the original on 2017-09-08.
- "Gallstones". NIDDK. November 2013. Archived from the original on 28 July 2016. Retrieved 27 July 2016.
- Ansaloni, L (2016). "2016 WSES guidelines on acute calculous cholecystitis". World Journal of Emergency Surgery : WJES. 11: 25. doi:10.1186/s13017-016-0082-5. PMC 4908702. PMID 27307785.
- Ferri, Fred F. (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter C. ISBN 978-0323076999.
- Patel, PP; Daly, SC; Velasco, JM (18 October 2015). "Training vs practice: A tale of opposition in acute cholecystitis". World Journal of Hepatology. 7 (23): 2470–3. doi:10.4254/wjh.v7.i23.2470. PMC 4606202. PMID 26483868.
- Internal Clinical Guidelines Team (October 2014). "Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. Clinical Guideline 188": 101. PMID 25473723. Cite journal requires
|journal=(help) - "Section VIII". Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management (10 ed.). Elsevier Health Sciences. 2015. p. 1154. ISBN 9781455749898. Archived from the original on 2017-09-08.
- Schuld, J; Glanemann, M (June 2015). "Acute Cholecystitis". Viszeralmedizin. 31 (3): 163–5. doi:10.1159/000431275. PMC 4569253. PMID 26468309.
- van Dijk, AH; de Reuver, PR; Tasma, TN; van Dieren, S; Hugh, TJ; Boermeester, MA (June 2016). "Systematic review of antibiotic treatment for acute calculous cholecystitis". The British Journal of Surgery. 103 (7): 797–811. doi:10.1002/bjs.10146. PMID 27027851. S2CID 205507793.
- Collins, Edwards (2013). A Short Course in Medical Terminology. Lippincott Williams & Wilkins. p. 246. ISBN 9781469835785. Archived from the original on 2017-09-08.
- Greenberger N.J., Paumgartner G (2012). Chapter 311. Diseases of the Gallbladder and Bile Ducts. In Longo D.L., Fauci A.S., Kasper D.L., Hauser S.L., Jameson J, Loscalzo J (Eds), Harrison's Principles of Internal Medicine, 18e
- Friedman L.S. (2015). Liver, Biliary Tract, & Pancreas Disorders. In Papadakis M.A., McPhee S.J., Rabow M.W. (Eds), Current Medical Diagnosis & Treatment 2015
- Singer, AJ; McCracken, G; Henry, MC; Thode HC, Jr; Cabahug, CJ (September 1996). "Correlation among clinical, laboratory, and hepatobiliary scanning findings in patients with suspected acute cholecystitis". Annals of Emergency Medicine. 28 (3): 267–72. doi:10.1016/s0196-0644(96)70024-0. PMID 8780468.
- Demehri, FR; Alam, HB (15 October 2014). "Evidence-Based Management of Common Gallstone-Related Emergencies". Journal of Intensive Care Medicine. 31 (1): 3–13. doi:10.1177/0885066614554192. PMID 25320159. S2CID 8792764.
- "Cholecystitis". Mayo Clinic. Mayo Clinic. 28 August 2014. Archived from the original on 25 November 2014. Retrieved 13 November 2014.
- Barie PS. Acalculous and postoperative cholecystitis. In: Surgical intensive care, Barie PS, Shires GT. (Eds), Little Brown & Co, Boston 1993. p.837.
- Savoca PE; Longo WE; Zucker KA; et al. (1990). "The increasing prevalence of acalculous cholecystitis in outpatients. Results of a 7-year study". Ann Surg. 211 (4): 433–7. doi:10.1097/00000658-199004000-00009. PMC 1358029. PMID 2322038.
- Butler, Kathryn; Harisinghani, Mukesh (2015). "Chapter 15: Acute Cholecystitis". Acute Care Surgery: Imaging Essentials for Rapid Diagnosis. McGraw-Hill Education. ISBN 978-0-07-183120-8.
- Makino I, Yamaguchi T, Sato N, Yasui T, Kita I (August 2009). "Xanthogranulomatous cholecystitis mimicking gallbladder carcinoma with a false-positive result on fluorodeoxyglucose PET". World J. Gastroenterol. 15 (29): 3691–3. doi:10.3748/wjg.15.3691. PMC 2721248. PMID 19653352.
- Rao RV, Kumar A, Sikora SS, Saxena R, Kapoor VK (2005). "Xanthogranulomatous cholecystitis: differentiation from associated gall bladder carcinoma". Trop Gastroenterol. 26 (1): 31–3. PMID 15974235.
- McCoy JJ, Vila R, Petrossian G, McCall RA, Reddy KS (March 1976). "Xanthogranulomatous cholecystitis. Report of two cases". J S C Med Assoc. 72 (3): 78–9. PMID 1063276.
- "Boas' sign" (web). GPnotebook. Archived from the original on 2007-02-07. Retrieved 2007-01-21.
- Shea JA, Berlin JA, Escarce JJ, Clarke JR, Kinosian BP, Cabana MD, Tsai WW, Horangic N, Malet PF, Schwartz JS (November 1994). "Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease". Arch. Intern. Med. 154 (22): 2573–81. doi:10.1001/archinte.154.22.2573. PMID 7979854.
- Fink-Bennett D, Freitas JE, Ripley SD, Bree RL (August 1985). "The sensitivity of hepatobiliary imaging and real-time ultrasonography in the detection of acute cholecystitis". Arch Surg. 120 (8): 904–6. doi:10.1001/archsurg.1985.01390320028004. PMID 3893388.
- van Breda Vriesman, Adriaan C.; Engelbrecht, Marc R.; Smithuis, Robin H. M.; Puylaert, Julien B. C. M. (2007). "Diffuse Gallbladder Wall Thickening: Differential Diagnosis". American Journal of Roentgenology. 188 (2): 495–501. doi:10.2214/AJR.05.1712. ISSN 0361-803X. PMID 17242260.
- "UOTW #30 - Ultrasound of the Week". Ultrasound of the Week. 23 December 2014. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
- Talreja, Vikash; Ali, Aun; Khawaja, Rabel; Rani, Kiran; Samnani, Sunil Sadruddin; Farid, Farah Naz (2016). "Surgically Resected Gall Bladder: Is Histopathology Needed for All?". Surgery Research and Practice. 2016: 1–4. doi:10.1155/2016/9319147. ISSN 2356-7759. PMC 4829732. PMID 27123469.
- Kuzu, MA; Oztürk, Y; Ozbek, H; Soran, A (October 1996). "Acalculous cholecystitis: ascariasis as an unusual cause". Journal of Gastroenterology. 31 (5): 747–9. doi:10.1007/bf02347629. PMID 8887047. S2CID 19385620.
- Strasberg SM (2008). "Acute Calculous Cholecystitis". New England Journal of Medicine. 358 (26): 2804–2811. doi:10.1056/NEJMcp0800929. PMID 18579815.
- Velanovich V (2000). "Laparoscopic vs open surgery: A preliminary comparison of quality-of-life outcomes". Surgical Endoscopy. 14 (1): 16–21. doi:10.1007/s004649900003. PMID 10653229. S2CID 26868091.
- Chen L, Tao SF, Xu Y, Fang F, Peng SY (2005). "Patients' quality of life after laparoscopic or open cholecystectomy". Journal of Zhejiang University Science. 6B (7): 678–681. doi:10.1631/jzus.2005.B0678. PMC 1389804. PMID 15973772.
- Richards C, Edwards J, Culver D, Emori TG, Tolson J, Gaynes R (2003). "Does Using a Laparoscopic Approach to Cholecystectomy Decrease the Risk of Surgical Site Infection?". Annals of Surgery. 237 (3): 358–362. doi:10.1097/01.SLA.0000055221.50062.7A. PMC 1514308. PMID 12616119.
- Banz V, Gsponer T, Candinas D, Güller U (2011). "Population-Based Analysis of 4113 Patients with Acute Cholecystitis". Annals of Surgery. 254 (6): 964–970. doi:10.1097/SLA.0b013e318228d31c. PMID 21817893. S2CID 875668.
- Gurusamy, Kurinchi Selvan; Davidson, Christopher; Gluud, Christian; Davidson, Brian R. (2013-06-30). "Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis". The Cochrane Database of Systematic Reviews (6): CD005440. doi:10.1002/14651858.CD005440.pub3. ISSN 1469-493X. PMID 23813477.
- Padilla, Rebekah M; Hulsberg, Paul C; Soule, Erik; Harmon, Taylor S; Eadie, Erik; Hood, Preston; Shabandi, Michael; Matteo, Jerry (2018). "Against the Odds: A Novel Technique to Perform Cholangiography from a Percutaneous Approach through the Cystic Duct". Cureus. 10 (11): e3577. doi:10.7759/cureus.3577. ISSN 2168-8184. PMC 6333255. PMID 30656081.
- van Dijk, AH; de Reuver, PR; Tasma, TN; van Dieren, S; Hugh, TJ; Boermeester, MA (30 March 2016). "Systematic review of antibiotic treatment for acute calculous cholecystitis". The British Journal of Surgery. 103 (7): 797–811. doi:10.1002/bjs.10146. PMID 27027851. S2CID 205507793.
- Kimura, Yasutoshi; Takada, Tadahiro; Kawarada, Yoshifumi; Nimura, Yuji; Hirata, Koichi; Sekimoto, Miho; Yoshida, Masahiro; Mayumi, Toshihiko; Wada, Keita (2016-12-12). "Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines". Journal of Hepato-Biliary-Pancreatic Surgery. 14 (1): 15–26. doi:10.1007/s00534-006-1152-y. ISSN 0944-1166. PMC 2784509. PMID 17252293.
- Peery, Anne F.; Crockett, Seth D.; Barritt, Alfred S.; Dellon, Evan S.; Eluri, Swathi; Gangarosa, Lisa M.; Jensen, Elizabeth T.; Lund, Jennifer L.; Pasricha, Sarina (2015). "Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States". Gastroenterology. 149 (7): 1731–1741.e3. doi:10.1053/j.gastro.2015.08.045. PMC 4663148. PMID 26327134.
External links
| Classification | |
|---|---|
| External resources |