Mental health
Mental health, defined by the World Health Organization (WHO), is “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community”.[1] According to the WHO, mental health includes "subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others".[2] From the perspectives of positive psychology or of holism, mental health may include an individual's ability to enjoy life and to create a balance between life activities and efforts to achieve psychological resilience.[3] Cultural differences, subjective assessments, and competing professional theories all affect how one defines "mental health".[2][4]
| Part of a series on |
| Public health |
|---|
|
Distinguishing mental health from mental illness
According to the U.K. Surgeon Journal (1999), mental health is the successful performance of the mental function resulting in productive activities, fulfilling relationships with other people, and providing the ability to adapt to change and cope with adversity. The term mental illness refers collectively to all diagnosable mental disorders—health conditions characterized by alterations in thinking, mood, or behavior associated with distress or impaired functioning.[5][6] Mental health has long been defined as the absence of psychopathologies, such as depression and anxiety. The absence of mental illness, however, is a minimal outcome from a psychological perspective on lifespan development.[7] Corey M Keyes has created a two continua model of mental illness and health which holds that both are related, but distinct dimensions: one continuum indicates the presence or absence of mental health, the other the presence or absence of mental illness.[7] For example, people with optimal mental health can also have a mental illness, and people who have no mental illness can also have poor mental health.[8] Indeed, the World Health Organization distinguishes mental health from mental illness: "{mental health}... a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity".[9]
Marie Jahoda described six major, fundamental categories that can be used to categorize mentally healthy individuals. These include a positive attitude towards the self, personal growth, integration, autonomy, a true perception of reality, and environmental mastery, which include adaptability and healthy interpersonal relationships.[10]
Mental health problems may arise due to stress, loneliness, depression, anxiety, relationship problems, death of a loved one, suicidal thoughts, grief, addiction, ADHD, self-harm, various mood disorders, or other mental illnesses of varying degrees, as well as learning disabilities.[11][12] Therapists, psychiatrists, psychologists, social workers, nurse practitioners, or family physicians can help manage mental illness with treatments such as therapy, counseling, or medication.
History
Early history
In the mid-19th century, William Sweetser was the first to coin the term mental hygiene, which can be seen as the precursor to contemporary approaches to work on promoting positive mental health.[13][14] Isaac Ray, the fourth president[15] of the American Psychiatric Association and one of its founders, further defined mental hygiene as "the art of preserving the mind against all incidents and influences calculated to deteriorate its qualities, impair its energies, or derange its movements".[14]
In American history, mentally ill patients were thought to be religiously punished. This response persisted through the 1700s, along with inhumane confinement and stigmatization of such individuals.[16] Dorothea Dix (1802–1887) was an important figure in the development of the "mental hygiene" movement. Dix was a school teacher who endeavored to help people with mental disorders and to expose the sub-standard conditions into which they were put.[17] This became known as the "mental hygiene movement".[17] Before this movement, it was not uncommon that people affected by mental illness would be considerably neglected, often left alone in deplorable conditions without sufficient clothing.[17] From 1840-1880, she won over the support of the federal government to set up over 30 state psychiatric hospitals; however, they were understaffed, under-resourced, and were accused of violating human rights.[16]
Emil Kraepelin in 1896 developed the taxonomy of mental disorders which has dominated the field for nearly 80 years. Later, the proposed disease model of abnormality was subjected to analysis and considered normality to be relative to the physical, geographical and cultural aspects of the defining group.[18]
At the beginning of the 20th century, Clifford Beers founded "Mental Health America – National Committee for Mental Hygiene", after publication of his accounts as a patient in several lunatic asylums, A Mind That Found Itself, in 1908[19][20][21] and opened the first outpatient mental health clinic in the United States.[22]
The mental hygiene movement, similar to the social hygiene movement, had at times been associated with advocating eugenics and sterilisation of those considered too mentally deficient to be assisted into productive work and contented family life.[23][24] In the post-WWII years, references to mental hygiene were gradually replaced by the term 'mental health' due to its positive aspect that evolves from the treatment of illness to preventive and promotive areas of healthcare.[25]
Deinstitutionalization and transinstitutionalization
When state hospitals were accused of violating human rights, advocates pushed for deinstitutionalization: the replacement of federal mental hospitals for community mental health services. The closure of state-provisioned psychiatric hospitals was enforced by the Community Mental Health Centers Act in 1963 that laid out terms in which only patients who posed an imminent danger to others or themselves could be admitted into state facilities.[26] This was seen as an improvement from previous conditions, however, there remains a debate on the conditions of these community resources.
It has been proven that this transition was beneficial for many patients: there was an increase in overall satisfaction, a better quality of life, more friendships between patients, and not too costly. This proved to be true only in the circumstance that treatment facilities that had enough funding for staff and equipment as well as proper management.[27] However, this idea is a polarizing issue. Critics of deinstitutionalization argue that poor living conditions prevailed, patients were lonely, and they did not acquire proper medical care in these treatment homes.[28] Additionally, patients that were moved from state psychiatric care to nursing and residential homes had deficits in crucial aspects of their treatment. Some cases result in the shift of care from health workers to patients’ families, where they do not have the proper funding or medical expertise to give proper care.[28] On the other hand, patients that are treated in community mental health centers lack sufficient cancer testing, vaccinations, or otherwise regular medical check-ups.[28]
Other critics of state deinstitutionalization argue that this was simply a transition to “transinstitutionalization”, or the idea that prisons and state-provisioned hospitals are interdependent. In other words, patients become inmates. This draws on the Penrose Hypothesis of 1939, which theorized that there was an inverse relationship between prisons’ population size and the number of psychiatric hospital beds.[29] This means that populations that require psychiatric mental care will transition between institutions, which in this case, includes state psychiatric hospitals and criminal justice systems. Thus, a decrease in available psychiatric hospital beds occurred at the same time as an increase in inmates.[29] Although some are skeptical that this is due to other external factors, others will reason this conclusion to a lack of empathy for the mentally ill. There is no argument in the social stigmatization of those with mental illnesses, they have been widely marginalized and discriminated against in society.[16] In this source, researchers analyze how most compensation prisoners (detainees who are unable or unwilling to pay a fine for petty crimes) are unemployed, homeless, and with an extraordinarily high degree of mental illnesses and substance abuse.[29] Compensation prisoners then lose prospective job opportunities, face social marginalization, and lack access to resocialization programs, which ultimately facilitate reoffending.[29] The research sheds light on how the mentally ill — and in this case, the poor— are further punished for certain circumstances that are beyond their control, and that this is a vicious cycle that repeats itself. Thus, prisons embody another state-provisioned mental hospital.
Families of patients, advocates, and mental health professionals still call for the increase in more well-structured community facilities and treatment programs with a higher quality of long-term inpatient resources and care. With this more structured environment, the United States will continue with more access to mental health care and an increase in the overall treatment of the mentally ill.
However, there is still a lack of studies for MHCs( mental Health conditions) to raise awareness, knowledge development, and attitude of seeking medical treatment for MHCs in Bangladesh. People in rural areas often seek treatment from the traditional healers and these MHCs sometimes considered as a spiritual matters.[30]
Epidemiology
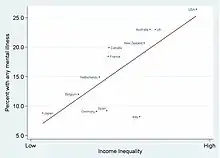
Mental illnesses are more common than cancer, diabetes, or heart disease. Over 26 percent of all Americans over the age of 18 meet the criteria for having a mental illness.[31] Evidence suggests that 450 million people worldwide have some mental illness. Major depression ranks fourth among the top 10 leading causes of disease worldwide. By 2029, mental illness is predicted to become the leading cause of disease worldwide. Women are more likely to have a mental illness than men. One million people commit suicide every year and 10 to 20 million attempt it.[32] A World Health Organization (WHO) report estimates the global cost of mental illness at nearly $2.5 trillion (two-thirds in indirect costs) in 2010, with a projected increase to over $6 trillion by 2030.[33]
Evidence from the WHO suggests that nearly half of the world's population is affected by mental illness with an impact on their self-esteem, relationships and ability to function in everyday life.[34] An individual's emotional health can impact their physical health. Poor mental health can lead to problems such as the ability to make adequate decisions and substance abuse.[35]
Good mental health can improve life quality whereas poor mental health can worsen it. According to Richards, Campania, & Muse-Burke, "There is growing evidence that is showing emotional abilities are associated with pro-social behaviors such as stress management and physical health."[35] Their research also concluded that people who lack emotional expression are inclined to anti-social behaviors (e.g., drug and alcohol abuse, physical fights, vandalism), which reflects ones mental health and suppressed emotions.[35] Adults and children who face mental illness may experience social stigma, which can exacerbate the issues.[36]
Global Prevalence
Mental health can be seen as an unstable continuum, where an individual's mental health may have many different possible values.[37] Mental wellness is generally viewed as a positive attribute, even if the person does not have any diagnosed mental health condition. This definition of mental health highlights emotional well-being, the capacity to live a full and creative life, and the flexibility to deal with life's inevitable challenges. Some discussions are formulated in terms of contentment or happiness.[38] Many therapeutic systems and self-help books offer methods and philosophies espousing strategies and techniques vaunted as effective for further improving the mental wellness. Positive psychology is increasingly prominent in mental health.
A holistic model of mental health generally includes concepts based upon anthropological, educational, psychological, religious, and sociological perspectives. There are also models as theoretical perspectives from personality, social, clinical, health and developmental psychology.[39][40]
The tripartite model of mental well-being[37][41] views mental well-being as encompassing three components of emotional well-being, social well-being, and psychological well-being. Emotional well-being is defined as having high levels of positive emotions, whereas social and psychological well-being are defined as the presence of psychological and social skills and abilities that contribute to optimal functioning in daily life. The model has received empirical support across cultures.[41][42][43] The Mental Health Continuum-Short Form (MHC-SF) is the most widely used scale to measure the tripartite model of mental well-being.[44][45][46]
Children and young adults
According to 2020 data, mental illnesses have a stagnant incidence among adults but are increasing among the youth, categorized as 12 to 17-year-olds.[47] Approximately 13% of youth in the United States reported suffering from at least one major depressive episode in 2019-20, with the greatest increase (18%) in Oregon.[47] Only 28% receive consistent treatment and 70% are left untreated.[47] In lower-income communities, it is more common to forego treatment as a result of financial resources. Being left untreated also leads to unhealthy coping mechanisms such as substance abuse, which in turn causes its own host of mental health issues.
Mental health and stability is a very important factor in a person's everyday life. The human brain develops many skills at an early age including social skills, behavioral skills, and one's way of thinking. Learning how to interact with others and how to focus on certain subjects are essential lessons to learn at a young age. This starts from the time we can talk all the way to when we are so old that we can barely walk. However, there are people in society who have difficulties with these skills and behave differently. A mental illness consists of a wide range of conditions that affects a person's mood, thinking, and behavior.[48] About 26% of people in the United States, ages 18 and older, have been diagnosed with some kind of mental disorder. However, not much is said about children with mental illnesses even though many develop one, even as early as age three.
The most common mental illnesses in children include, but are not limited to anxiety disorder, as well as depression in older children and teens. Having a mental illness at a younger age is different from having one in adulthood. Children's brains are still developing and will continue to develop until around the age of twenty-five.[49] When a mental illness is thrown into the mix, it becomes significantly harder for a child to acquire the necessary skills and habits that people use throughout the day. For example, behavioral skills don't develop as fast as motor or sensory skills do.[49] So when a child has an anxiety disorder, they begin to lack proper social interaction and associate many ordinary things with intense fear.[50] This can be scary for the child because they don't necessarily understand why they act and think the way that they do. Many researchers say that parents should keep an eye on their child if they have any reason to believe that something is slightly off.[49] If the children are evaluated earlier, they become more acquainted to their disorder and treating it becomes part of their daily routine.[49] This is opposed to adults who might not recover as quickly because it is more difficult for them to adopt when already being accustomed to a certain direction of life.
Mental illness affects not only the person themselves but the people around them. Friends and family also play an important role in the child's mental health stability and treatment.[51] If the child is young, parents are the ones who evaluate their child and decide whether or not they need some form of help.[52] Friends are a support system for the child and family as a whole. Living with a mental disorder is never easy, so it's always important to have people around to make the days a little easier. However, there are negative factors that come with the social aspect of mental illness as well. Parents are sometimes held responsible for their child's illness.[52] People also say that the parents raised their children in a certain way or they acquired their behavior from them. Family and friends are sometimes so ashamed of the idea of being close to someone with a disorder that the child feels isolated and thinks that they have to hide their illness from others.[52] When in reality, hiding it from people prevents the child from getting the right amount of social interaction and treatment to thrive in today's society.
Stigmas are also a well-known factor in mental illness. A stigma is defined as “a mark of disgrace associated with a particular circumstance, quality, or person.” Stigmas are used especially when it comes to mentally disabled people. People have this assumption that everyone with a mental problem, no matter how mild or severe, is automatically considered destructive or a criminal person. Thanks to the media, this idea has been planted in our brains from a young age.[53] Watching movies about teens with depression or children with Autism makes us think that all of the people that have a mental illness are like the ones on TV. In reality, the media displays an exaggerated version of most illnesses. Unfortunately, not many people know that, so they continue to belittle those with disorders. In a recent study, a majority of young people associate mental illness with extreme sadness or violent tendencies .[54] Now that children are becoming more and more open to technology and the media itself, future generations will then continue to pair mental illness with negative thoughts. The media should be explaining that many people with psychiatric disorders like ADHD and Anxiety, can live an ordinary life with the correct treatment and should not be punished for something they cannot help. Along with social stigmas, individuals with a mental illness can develop a self-stigma. A self-stigma is when the affected individual does not come forward about their feelings in fear of being judged. These self-stigmas can deter the individual from seeking help and treatment.[55]
Sueki, (2013) carried out a study titled “The effect of suicide-related internet use on users’ mental health: A longitudinal Study”. This study investigated the effects of suicide-related internet use on user's suicidal thoughts, predisposition to depression and anxiety, and loneliness. The study consisted of 850 internet users; the data was obtained by carrying out a questionnaire amongst the participants. This study found that browsing websites related to suicide, and methods used to commit suicide, harmed suicidal thoughts and increased depression and anxiety tendencies. The study concluded that as suicide-related internet use adversely affected the mental health of certain age groups it may be prudent to reduce or control their exposure to these websites. These findings certainly suggest that the internet can indeed have a profoundly negative impact on our mental health.[56]
Psychiatrist Thomas Szasz compared that 50 years ago children were either categorized as good or bad, and today "all children are good, but some are mentally healthy and others are mentally ill". Social control and forced identity creation is the cause of many mental health problems among today's children.[57] A behavior or misbehavior might not be an illness but exercise of their free will and today's immediacy in drug administration for every problem along with the legal over-guarding and regard of a child's status as a dependent shakes their personal self and invades their internal growth.
The homeless population
Mental illness is not only prevalent among children and young adults but also the homeless. Mental illness is thought to be extremely prevalent among homeless populations, though access to proper diagnoses is limited. In an article written by Lisa Godman and her colleagues, they reference Smith’s research on the prevalence of PTSD among homeless people. His research stated, "Homelessness itself is a risk factor for emotional disorder."[58] What this quote is saying is that being homeless itself can cause the emotional disorder. Without looking for other reasons for emotional disorder and really looking at the simple fact that an individual is homeless can cause the emotional disorder. Godman’s article stated "Recently, Smith ( 1991) investigated the prevalence of PTSD among a sample of 300 randomly selected homeless single women and mothers in St. Louis, Missouri. Using the Diagnostic Interview Schedule (DIS; Robins, 1981; Robins & Helzer, 1984), she found that 53% of the respondents could be diagnosed as exhibiting full-blown cases of PTSD." As the source explains, the conclusion that was drawn from Smith’s investigation after studying 300 homeless individuals is that 53% of those people were eligible to be diagnosed with PTSD. She continues and states: "In addition, data from clinical observations, self-reports, and empirical studies suggest that at least two commonly reported symptoms of psychological trauma, social disaffiliation and learned helplessness are highly prevalent among homeless individuals and families."[59] Other data were able to prove that PTSD and learned helplessness were two symptoms that were very much present among homeless individuals and families. The question would be how are these people being helped. This is evident that mental health among the homeless is an issue existing but barely touched.[60] In another article by Stephen W. Hwang and Rochelle E Garner, they talk about the ways that the homeless are getting actually getting help. It states "For homeless people with mental illness, case management linked to other services was effective in improving psychiatric symptoms, and assertive case management was effective in decreasing psychiatric hospitalizations and increasing outpatient contacts. For homeless people with substance abuse problems, case management resulted in greater decreases in substance use than did usual care."[61] The question would be how are these people being helped. As the source explained, case management provided by services helped improve psychiatric symptoms. It also caused a decrease in substance use than usual media care.[62]
Immigrants and refugees
The Rohingya from Myanmar are a large group of stateless people who experienced war, deprivation of social rights, and other cultural and political instability and they are currently residing in the southeastern part of Bangladesh as refugees. There are very little research has been done on their mental health status due to war, daily environmental stressors due to continuous displacement, historical trauma, and life in the refugee camp.[63]
A cross-sectional study was conducted among 148 Rohingya adults in the refugee camp in Bangladesh and the result indicated that people are suffering from post-traumatic stress disorder (PTSD), depression, somatic impairment, and other associated functional impairment as well. this study revealed that all these MHCs developed due to the high level of daily environmental stressors in the camp, also due to lack of food, lack of freedom of movement.[63]
Cultural and religious considerations
Mental health is a socially constructed and socially defined concept; that is, different societies, groups, cultures, institutions, and professions have very different ways of conceptualizing its nature and causes, determining what is mentally healthy, and deciding what interventions, if any, are appropriate.[64] Thus, different professionals will have different cultural, class, political and religious backgrounds, which will impact the methodology applied during treatment. In the context of deaf mental health care, it is necessary for professionals to have cultural competency of deaf and hard of hearing people and to understand how to properly rely on trained, qualified, and certified interpreters when working with culturally Deaf clients.
Research has shown that there is stigma attached to mental illness.[65] Due to such stigma, individuals may resist 'labeling' and may be driven to respond to mental health diagnoses with denialism.[66] Family caregivers of individuals with mental disorders may also suffer discrimination or face stigma.[67]
Addressing and eliminating the social stigma and perceived stigma attached to mental illness has been recognized as crucial to education and awareness surrounding mental health issues. In the United Kingdom, the Royal College of Psychiatrists organized the campaign Changing Minds (1998–2003) to help reduce stigma,[68] while in the United States, efforts by entities such as the Born This Way Foundation and The Manic Monologues specifically focus on removing the stigma surrounding mental illness.[69][70] The National Alliance on Mental Illness is a U.S. institution founded in 1979 to represent and advocate for those struggling with mental health issues. NAMI helps to educate about mental illnesses and health issues, while also working to eliminate stigma[71] attached to these disorders.
Many mental health professionals are beginning to, or already understand, the importance of competency in religious diversity and spirituality. They are also partaking in cultural training to better understand which interventions work best for these different groups of people. The American Psychological Association explicitly states that religion must be respected. Education in spiritual and religious matters is also required by the American Psychiatric Association,[72] however, far less attention is paid to the damage that more rigid, fundamentalist faiths commonly practiced in the United States can cause.[73] This theme has been widely politicized in 2018 such as with the creation of the Religious Liberty Task Force in July of that year.[74] Also, many providers and practitioners in the United States are only beginning to realize that the institution of mental healthcare lacks knowledge and competence of many non-Western cultures, leaving providers in the United States ill-equipped to treat patients from different cultures.[75]
Mental health and occupations
Mental health in social work
Social work in mental health, also called psychiatric social work, is a process where an individual in a setting is helped to attain freedom from overlapping internal and external problems (social and economic situations, family and other relationships, the physical and organizational environment, psychiatric symptoms, etc.). It aims for harmony, quality of life, self-actualization and personal adaptation across all systems. Psychiatric social workers are mental health professionals that can assist patients and their family members in coping with both mental health issues and various economic or social problems caused by mental illness or psychiatric dysfunctions and to attain improved mental health and well-being. They are vital members of the treatment teams in Departments of Psychiatry and Behavioral Sciences in hospitals. They are employed in both outpatient and inpatient settings of a hospital, nursing homes, state and local governments, substance abuse clinics, correctional facilities, health care services...etc.[76]
In the United States, social workers provide most of the mental health services. According to government sources, 60 percent of mental health professionals are clinically trained social workers, 10 percent are psychiatrists, 23 percent are psychologists, and 5 percent are psychiatric nurses.[77]
Mental health social workers in Japan have professional knowledge of health and welfare and skills essential for person's well-being. Their social work training enables them as a professional to carry out Consultation assistance for mental disabilities and their social reintegration; Consultation regarding the rehabilitation of the victims; Advice and guidance for post-discharge residence and re-employment after hospitalized care, for major life events in regular life, money and self-management and other relevant matters to equip them to adapt in daily life. Social workers provide individual home visits for mentally ill and do welfare services available, with specialized training a range of procedural services are coordinated for home, workplace and school. In an administrative relationship, Psychiatric social workers provides consultation, leadership, conflict management and work direction. Psychiatric social workers who provides assessment and psychosocial interventions function as a clinician, counselor and municipal staff of the health centers.[78]
Factors affecting mental health
Economic factors
Unemployment has been shown to hurt an individual's emotional well-being, self-esteem, and more broadly their mental health. Increasing unemployment has been shown to have a significant impact on mental health, predominantly depressive disorders.[79] This is an important consideration when reviewing the triggers for mental health disorders in any population survey.[80]
Emotional mental disorders are a leading cause of disabilities worldwide. Investigating the degree and severity of untreated emotional mental disorders throughout the world is a top priority of the World Mental Health (WMH) survey initiative,[81] which was created in 1998 by the World Health Organization (WHO).[82] "Neuropsychiatric disorders are the leading causes of disability worldwide, accounting for 37% of all healthy life years lost through disease.These disorders are most destructive to low and middle-income countries due to their inability to provide their citizens with proper aid. Despite modern treatment and rehabilitation for emotional mental health disorders, "even economically advantaged societies have competing priorities and budgetary constraints".
The World Mental Health survey initiative has suggested a plan for countries to redesign their mental health care systems to best allocate resources. "A first step is documentation of services being used and the extent and nature of unmet treatment needs. A second step could be to do a cross-national comparison of service use and unmet needs in countries with different mental health care systems. Such comparisons can help to uncover optimum financing, national policies, and delivery systems for mental health care."
Knowledge of how to provide effective emotional mental health care has become imperative worldwide. Unfortunately, most countries have insufficient data to guide decisions, absent or competing visions for resources, and near-constant pressures to cut insurance and entitlements. WMH surveys were done in Africa (Nigeria, South Africa), the Americas (Colombia, Mexico, United States), Asia and the Pacific (Japan, New Zealand, Beijing and Shanghai in the People's Republic of China), Europe (Belgium, France, Germany, Italy, Netherlands, Spain, Ukraine), and the middle east (Israel, Lebanon). Countries were classified with World Bank criteria as low-income (Nigeria), lower-middle-income (China, Colombia, South Africa, Ukraine), higher middle-income (Lebanon, Mexico), and high-income.
The coordinated surveys on emotional mental health disorders, their severity, and treatments were implemented in the aforementioned countries. These surveys assessed the frequency, types, and adequacy of mental health service use in 17 countries in which WMH surveys are complete. The WMH also examined unmet needs for treatment in strata defined by the seriousness of mental disorders. Their research showed that "the number of respondents using any 12-month mental health service was generally lower in developing than in developed countries, and the proportion receiving services tended to correspond to countries' percentages of gross domestic product spent on health care". "High levels of unmet need worldwide are not surprising, since WHO Project ATLAS' findings of much lower mental health expenditures than was suggested by the magnitude of burdens from mental illnesses. Generally, unmet needs in low-income and middle-income countries might be attributable to these nations spending reduced amounts (usually <1%) of already diminished health budgets on mental health care, and they rely heavily on out-of-pocket spending by citizens who are ill-equipped for it".
Stress
The Centre for Addiction and Mental Health discuss how a certain amount of stress is a normal part of daily life. Small doses of stress help people meet deadlines, be prepared for presentations, be productive and arrive on time for important events. However, long-term stress can become harmful. When stress becomes overwhelming and prolonged, the risks for mental health problems and medical problems increase."[83]
Mental health protection and promotion
"The terms mental health promotion and prevention have often been confused. Promotion is defined as intervening to optimize positive mental health by addressing determinants of positive mental health (i.e. protective factors) before a specific mental health problem has been identified, with the ultimate goal of improving the positive mental health of the population. Mental health prevention is defined as intervening to minimize mental health problems (i.e. risk factors) by addressing determinants of mental health problems before a specific mental health problem has been identified in the individual, group, or population of focus with the ultimate goal of reducing the number of future mental health problems in the population."[84][85]
In order to improve your emotional mental health, the root of the issue has to be resolved. "Prevention emphasizes the avoidance of risk factors; promotion aims to enhance an individual's ability to achieve a positive sense of self-esteem, mastery, well-being, and social inclusion."[86] Mental health promotion attempts to increase protective factors and healthy behaviors that can help prevent the onset of a diagnosable mental disorder and reduce risk factors that can lead to the development of a mental disorder.[84] It is very important to improve your emotional mental health by surrounding yourself with positive relationships. We as humans feed off companionships and interactions with other people. Another way to improve your emotional mental health is by participating in activities that can allow you to relax and take time for yourself. Yoga is a great example of an activity that calms your entire body and nerves. According to a study on well-being by Richards, Campania, and Muse-Burke, "mindfulness is considered to be a purposeful state, it may be that those who practice it belief in its importance and value being mindful, so that valuing of self-care activities may influence the intentional component of mindfulness."[35]
Mental health is conventionally defined as a hybrid of absence of a mental disorder and the presence of well-being. Focus is increasing on preventing mental disorders. Prevention is beginning to appear in mental health strategies, including the 2004 WHO report "Prevention of Mental Disorders", the 2008 EU "Pact for Mental Health" and the 2011 US National Prevention Strategy.[87][88] Some commentators have argued that a pragmatic and practical approach to mental disorder prevention at work would be to treat it the same way as physical injury prevention.[89]
Prevention of a disorder at a young age may significantly decrease the chances that a child will suffer from a disorder later in life, and shall be the most efficient and effective measure from a public health perspective.[90] Prevention may require the regular consultation of a physician for at least twice a year to detect any signs that reveal any mental health concerns. Similar to mandated health screenings, bills across the U.S. are being introduced to require mental health screenings for students attending public schools. Supporters of these bills hope to diagnose mental illnesses such as anxiety and depression to prevent self-harm and any harm induced on other students.
Additionally, social media is becoming a resource for prevention. In 2004, the Mental Health Services Act[91] began to fund marketing initiatives to educate the public on mental health. This California-based project is working to combat the negative perception with mental health and reduce the stigma associated with it. While social media can benefit mental health, it can also lead to deterioration if not managed properly.[92] Limiting social media intake is beneficial .[93]
Care navigation
Mental health care navigation helps to guide patients and families through the fragmented, often confusing mental health industries. Care navigators work closely with patients and families through discussion and collaboration to provide information on best therapies as well as referrals to practitioners and facilities specializing in particular forms of emotional improvement. The difference between therapy and care navigation is that the care navigation process provides information and directs patients to therapy rather than providing therapy. Still, care navigators may offer diagnosis and treatment planning. Though many care navigators are also trained therapists and doctors. Care navigation is the link between the patient and the below therapies. A clear recognition that mental health requires medical intervention was demonstrated in a study by Kessler et al. of the prevalence and treatment of mental disorders from 1990 to 2003 in the United States. Despite the prevalence of mental health disorders remaining unchanged during this period, the number of patients seeking treatment for mental disorders increased threefold.[94]
Pharmacotherapy
Pharmacotherapy is a therapy that uses pharmaceutical drugs. Pharmacotherapy is used in the treatment of mental illness through the use of antidepressants, benzodiazepines, and the use of elements such as lithium.
Physical activity
For some people, physical exercise can improve mental as well as physical health. Playing sports, walking, cycling, or doing any form of physical activity trigger the production of various hormones, sometimes including endorphins, which can elevate a person's mood.[95]
Studies have shown that in some cases, physical activity can have the same impact as antidepressants when treating depression and anxiety.[96]
Moreover, cessation of physical exercise may have adverse effects on some mental health conditions, such as depression and anxiety. This could lead to many different negative outcomes such as obesity, skewed body image, lower levels of certain hormones, and many more health risks associated with mental illnesses.[97]
Activity therapies
Activity therapies also called recreation therapy and occupational therapy, promote healing through active engagement. Making crafts can be a part of occupational therapy. Walks can be a part of recreation therapy. In recent years colouring has been recognised as an activity that has been proven to significantly lower the levels of depressive symptoms and anxiety in many studies.[98]
Expressive therapies
Expressive therapies or creative arts therapies are a form of psychotherapy that involves the arts or art-making. These therapies include art therapy, music therapy, drama therapy, dance therapy, and poetry therapy. It has been proven that Music therapy is an effective way of helping people who suffer from a mental health disorder.[99] Dramatherapy is approved by NICE for the treatment of psychosis.[100]
Psychotherapy
Psychotherapy is the general term for the scientific based treatment of mental health issues based on modern medicine. It includes a number of schools, such as gestalt therapy, psychoanalysis, cognitive behavioral therapy, psychedelic therapy, transpersonal psychology/psychotherapy, and dialectical behavioral therapy. Group therapy involves any type of therapy that takes place in a setting involving multiple people. It can include psychodynamic groups, expressive therapy groups, support groups (including the Twelve-step program), problem-solving and psychoeducation groups.
Self-compassion
According to Neff, self-compassion consists of three main positive components and their negative counterparts: Self-Kindness versus Self-Judgement, Common Humanity versus Isolation and Mindfulness versus Over-Identification.[101] Furthermore, there is evidence from a study by Shin & Lin suggesting specific components of self-compassion can predict specific dimensions of positive mental health (emotional, social, & psychological well-being).[102]
Social-Emotional Learning
The Callaborative for academic, social, emotional learning (CASEL) addresses five broad and interrelated areas of competence and highlights examples for each: self-awareness, self-management, social awareness, relationship skills, and responsible decision-making.[103] A meta-analysis was done by Alexendru Boncu, Iuliana Costeau, & Mihaela Minulescu (2017) looking at Social-emotional learning (SEL) studies and the effects on emotional and behaviour outcomes. They found a small but significant effect size (across the studies looked into) for externalized problems and social-emotional skills.[104]
Meditation
The practice of mindfulness meditation has several mental health benefits, such as bringing about reductions in depression, anxiety and stress.[105][106][107][108] Mindfulness meditation may also be effective in treating substance use disorders.[109][110] Further, mindfulness meditation appears to bring about favorable structural changes in the brain.[111][112][113]
The Heartfulness meditation program has proven to show significant improvements in the state of mind of health-care professionals.[114] A study posted on the US National Library of Medicine showed that these professionals of varied stress levels were able to improve their conditions after this meditation program was conducted. They benefited in aspects of burnouts and emotional wellness.
People with anxiety disorders participated in a stress-reduction program conducted by researchers from the Mental Health Service Line at the W.G. Hefner Veterans Affairs Medical Center in Salisbury, North Carolina. The participants practiced mindfulness meditation. After the study was over, it was concluded that the "mindfulness meditation training program can effectively reduce symptoms of anxiety and panic and can help maintain these reductions in patients with generalized anxiety disorder, panic disorder, or panic disorder with agoraphobia."[115]
Mental fitness
Mental fitness is a mental health movement that encourages people to intentionally regulate and maintain their emotional wellbeing through friendship, regular human contact, and activities that include meditation, calming exercises, aerobic exercise, mindfulness, having a routine and maintaining adequate sleep. Mental fitness is intended to build resilience against every-day mental health challenges to prevent an escalation of anxiety, depression and suicidal ideation, and help them cope with the escalation of those feelings if they occur.[116]
Spiritual counseling
Spiritual counsellors meet with people in need to offer comfort and support and to help them gain a better understanding of their issues and develop a problem-solving relation with spirituality. These types of counselors deliver care based on spiritual, psychological and theological principles.[117]
Mental health laws and public health policies
There are many factors that influence mental health including:
- Mental illness, disability, and suicide are ultimately the result of a combination of biology, environment, and access to and utilization of mental health treatment.
- Public health policies can influence access and utilization, which subsequently may improve mental health and help to progress the negative consequences of depression and its associated disability.
Emotional mental illnesses should be a particular concern in the United States since the U.S. has the highest annual prevalence rates (26 percent) for mental illnesses among a comparison of 14 developing and developed countries.[118] While approximately 80 percent of all people in the United States with a mental disorder eventually receive some form of treatment, on the average persons do not access care until nearly a decade following the development of their illness, and less than one-third of people who seek help receive minimally adequate care.[119] The government offers everyone programs and services, but veterans receive the most help, there is certain eligibility criteria that has to be met.[120]
Policies
The mental health policies in the United States have experienced four major reforms: the American asylum movement led by Dorothea Dix in 1843; the "mental hygiene" movement inspired by Clifford Beers in 1908; the deinstitutionalization started by Action for Mental Health in 1961; and the community support movement called for by The CMCH Act Amendments of 1975.[121]
In 1843, Dorothea Dix submitted a Memorial to the Legislature of Massachusetts, describing the abusive treatment and horrible conditions received by the mentally ill patients in jails, cages, and almshouses. She revealed in her Memorial: "I proceed, gentlemen, briefly to call your attention to the present state of insane persons confined within this Commonwealth, in cages, closets, cellars, stalls, pens! Chained, naked, beaten with rods, and lashed into obedience...."[122] Many asylums were built in that period, with high fences or walls separating the patients from other community members and strict rules regarding the entrance and exit. In those asylums, traditional treatments were well implemented: drugs were not used as a cure for a disease, but a way to reset equilibrium in a person's body, along with other essential elements such as healthy diets, fresh air, middle class culture, and the visits by their neighboring residents. In 1866, a recommendation came to the New York State Legislature to establish a separate asylum for chronic mentally ill patients. Some hospitals placed the chronic patients into separate wings or wards, or different buildings.[123]
In A Mind That Found Itself (1908) Clifford Whittingham Beers described the humiliating treatment he received and the deplorable conditions in the mental hospital.[124] One year later, the National Committee for Mental Hygiene (NCMH) was founded by a small group of reform-minded scholars and scientists – including Beers himself – which marked the beginning of the "mental hygiene" movement. The movement emphasized the importance of childhood prevention. World War I catalyzed this idea with an additional emphasis on the impact of maladjustment, which convinced the hygienists that prevention was the only practical approach to handle mental health issues.[125] However, prevention was not successful, especially for chronic illness; the condemnable conditions in the hospitals were even more prevalent, especially under the pressure of the increasing number of chronically ill and the influence of the depression.[121]
In 1961, the Joint Commission on Mental Health published a report called Action for Mental Health, whose goal was for community clinic care to take on the burden of prevention and early intervention of the mental illness, therefore to leave space in the hospitals for severe and chronic patients. The court started to rule in favor of the patients' will on whether they should be forced to treatment. By 1977, 650 community mental health centers were built to cover 43 percent of the population and serve 1.9 million individuals a year, and the lengths of treatment decreased from 6 months to only 23 days.[126] However, issues still existed. Due to inflation, especially in the 1970s, the community nursing homes received less money to support the care and treatment provided. Fewer than half of the planned centers were created, and new methods did not fully replace the old approaches to carry out its full capacity of treating power.[126] Besides, the community helping system was not fully established to support the patients' housing, vocational opportunities, income supports, and other benefits.[121] Many patients returned to welfare and criminal justice institutions, and more became homeless. The movement of deinstitutionalization was facing great challenges.[127]
After realizing that simply changing the location of mental health care from the state hospitals to nursing houses was insufficient to implement the idea of deinstitutionalization, the National Institute of Mental Health in 1975 created the Community Support Program (CSP) to provide funds for communities to set up a comprehensive mental health service and supports to help the mentally ill patients integrate successfully in the society. The program stressed the importance of other supports in addition to medical care, including housing, living expenses, employment, transportation, and education; and set up new national priority for people with serious mental disorders. In addition, the Congress enacted the Mental Health Systems Act of 1980 to prioritize the service to the mentally ill and emphasize the expansion of services beyond just clinical care alone.[128] Later in the 1980s, under the influence from the Congress and the Supreme Court, many programs started to help the patients regain their benefits. A new Medicaid service was also established to serve people who were diagnosed with a "chronic mental illness." People who were temporally hospitalized were also provided aid and care and a pre-release program was created to enable people to apply for reinstatement prior to discharge.[126] Not until 1990, around 35 years after the start of the deinstitutionalization, did the first state hospital begin to close. The number of hospitals dropped from around 300 by over 40 in the 1990s, and finally a Report on Mental Health showed the efficacy of mental health treatment, giving a range of treatments available for patients to choose.[128]
However, several critics maintain that deinstitutionalization has, from a mental health point of view, been a thoroughgoing failure. The seriously mentally ill are either homeless, or in prison; in either case (especially the latter), they are getting little or no mental health care. This failure is attributed to a number of reasons over which there is some degree of contention, although there is general agreement that community support programs have been ineffective at best, due to a lack of funding.[127]
The 2011 National Prevention Strategy included mental and emotional well-being, with recommendations including better parenting and early intervention programs, which increase the likelihood of prevention programs being included in future US mental health policies.[87] The NIMH is researching only suicide and HIV/AIDS prevention, but the National Prevention Strategy could lead to it focusing more broadly on longitudinal prevention studies.[129]
In 2013, United States Representative Tim Murphy introduced the Helping Families in Mental Health Crisis Act, HR2646. The bipartisan bill went through substantial revision and was reintroduced in 2015 by Murphy and Congresswoman Eddie Bernice Johnson. In November 2015, it passed the Health Subcommittee by an 18–12 vote.
See also
References
- "Mental health: strengthening our response". World Health Organization. August 2014. Retrieved 4 May 2014.
- "The world health report 2001 – Mental Health: New Understanding, New Hope" (PDF). WHO. Retrieved 4 May 2014.
- Snyder, C. R; Lopez, Shane J; Pedrotti, Jennifer Teramoto (2011). Positive psychology: the scientific and practical explorations of human strengths. SAGE. ISBN 978-1-4129-8195-8. OCLC 639574840.
- "Mental Health". medlineplus.gov. Retrieved 2019-11-20.
- National Alliance for the Mentally Ill, 2011
- "Mental Disorders". medlineplus.gov. Retrieved 2019-11-20.
- Westerhof, Gerben J.; Keyes, Corey L. M. (June 2010). "Mental Illness and Mental Health: The Two Continua Model Across the Lifespan". Journal of Adult Development. 17 (2): 110–119. doi:10.1007/s10804-009-9082-y. ISSN 1068-0667. PMC 2866965. PMID 20502508.
- "What is Mental Health and Mental Illness? | Workplace Mental Health Promotion". Workplace Mental Health Promotion.
- "Mental health: strengthening our response". www.who.int. Retrieved 2020-11-11.
- Jahoda, Marie (1958). "Current concepts of positive mental health". New York. doi:10.1037/11258-000. hdl:2027/mdp.39015004395078.
- "Practicing Effective Prevention". Center for the Application of Prevention Technologies. Substance Abuse and Mental Health Services Administration. 11 January 2016. Archived from the original on 5 September 2015. Retrieved 2 May 2014.
- Kitchener, Betty; Jorm, Anthony (2002). Mental Health First Aid Manual (1st ed.). Canberra: Center for Mental Health Research, Australian National University. p. 5. ISBN 978-0-7315-4891-0. OCLC 62228904.
- Shook, John R., ed. (April 2012). "Sweetser, William". Dictionary of Early American Philosophers. Bloomsbury Publishing USA. pp. 1016–1020. ISBN 978-1-4411-7140-5.
- Mandell, Wallace (1995). "Origins of Mental Health, The Realization of an Idea". Johns Hopkins Bloomberg School of Public Health. Baltimore, MD: Johns Hopkins University. Retrieved 9 June 2015.
- "Isaac Ray Award". www.psychiatry.org. American Psychiatric Association. Retrieved 27 October 2017.
- "A Brief History of Mental Illness and the U.S. Mental Health Care System". www.uniteforsight.org. Retrieved 2020-05-11.
- Barlow, D.H., Durand, V.M., Steward, S.H. (2009). Abnormal psychology: An integrative approach (Second Canadian Edition). Toronto: Nelson. p. 16
- Ebert, Andreas; Bär, Karl-Jürgen (2010). "Emil Kraepelin: A pioneer of scientific understanding of psychiatry and psychopharmacology". Indian Journal of Psychiatry. 52 (2): 191–192. doi:10.4103/0019-5545.64591. PMC 2927892. PMID 20838510.
- Amanda Peck (2013),Mental Health America – Origins, Retrieved June 9, 2015, from The Social Welfare History Project.
- Archived 2007-04-09 at the Wayback Machine
- BERTOLOTE, JOSÉ (June 2008). "The roots of the concept of mental health". World Psychiatry. 7 (2): 113–116. doi:10.1002/j.2051-5545.2008.tb00172.x. ISSN 1723-8617. PMC 2408392. PMID 18560478.
- Clifford Beers Clinic. (2006, October 30). About Clifford Beers Clinic. Retrieved June 1, 2007, from CliffordBeers.org
- Social Hygiene in 20th Century Britain Taylor & Francis, Page 80 to 83
- Encyclopedia of Children and Childhood in History and Society: Hygiene Jacqueline S. Wilkie.
- Bertolote, José (June 2008). "The roots of the concept of mental health". World Psychiatry. 7 (2): 113–116. doi:10.1002/j.2051-5545.2008.tb00172.x. PMC 2408392. PMID 18560478.
- "New York Times New York State Poll, June 2008". 2009-12-03. doi:10.3886/icpsr26164.v1. Cite journal requires
|journal=(help) - Knapp, Martin; Beecham, Jennifer; McDaid, David; Matosevic, Tihana; Smith, Monique (December 2010). "The economic consequences of deinstitutionalisation of mental health services: lessons from a systematic review of European experience: Economic consequences of deinstitutionalisation of mental health services". Health & Social Care in the Community. 19 (2): 113–125. doi:10.1111/j.1365-2524.2010.00969.x. PMID 21143545.
- Novella, Enric J. (December 2010). "Mental health care and the politics of inclusion: A social systems account of psychiatric deinstitutionalization". Theoretical Medicine and Bioethics. 31 (6): 411–427. doi:10.1007/s11017-010-9155-8. PMID 20711755. S2CID 23328647.
- Schildbach, Sebastian; Schildbach, Carola (25 October 2018). "Criminalization Through Transinstitutionalization: A Critical Review of the Penrose Hypothesis in the Context of Compensation Imprisonment". Frontiers in Psychiatry. 9: 534. doi:10.3389/fpsyt.2018.00534. PMC 6209624. PMID 30410452.
- Uddin, Mohammed Nazim; Bhar, Sunil; Islam, Fakir M Amirul (December 2019). "An assessment of awareness of mental health conditions and its association with socio-demographic characteristics: a cross-sectional study in a rural district in Bangladesh". BMC Health Services Research. 19 (1): 562. doi:10.1186/s12913-019-4385-6. PMC 6692949. PMID 31409332. S2CID 199547608.
- National Institute of Mental Health, 2011
- Sowers, Rowe, & Clay, 2009
- "Who". Mental illness.
- Storrie, Kim; Ahern, Kathy; Tuckett, Anthony (February 2010). "A systematic review: Students with mental health problems-A growing problem". International Journal of Nursing Practice. 16 (1): 1–6. doi:10.1111/j.1440-172X.2009.01813.x. PMID 20158541.
- Richards, KC; Campania, C; Muse-Burke, JL (July 2010). "Self-care and Well-being in Mental Health Professionals: The Mediating Effects of Self-awareness and Mindfulnes". Journal of Mental Health Counseling. 32 (3): 247–264. doi:10.17744/mehc.32.3.0n31v88304423806.
- Heary, Caroline; Hennessy, Eilis; Swords, Lorraine; Corrigan, Patrick (6 July 2017). "Stigma towards Mental Health Problems during Childhood and Adolescence: Theory, Research and Intervention Approaches". Journal of Child and Family Studies. 26 (11): 2949–2959. doi:10.1007/s10826-017-0829-y. S2CID 148951912.
- Keyes, Corey L. M. (2 January 2002). "The mental health continuum: from languishing to flourishing in life". Journal of Health and Social Behavior. 43 (2): 207–222. doi:10.2307/3090197. JSTOR 3090197. PMID 12096700. S2CID 2961978.
- Graham, Michael C. (2014). Facts of Life: ten issues of contentment. Outskirts Press. pp. 6–10. ISBN 978-1-4787-2259-5.
- Witmer, J.M.; Sweeny, T.J. (1992). "A holistic model for wellness and prevention over the lifespan". Journal of Counseling and Development. 71 (2): 140–148. doi:10.1002/j.1556-6676.1992.tb02189.x.
- Hattie, J.A.; Myers, J.E.; Sweeney, T.J. (2004). "A factor structure of wellness: Theory, assessment, analysis and practice". Journal of Counseling and Development. 82 (3): 354–364. doi:10.1002/j.1556-6678.2004.tb00321.x.
- Joshanloo, Mohsen (23 October 2015). "Revisiting the Empirical Distinction Between Hedonic and Eudaimonic Aspects of Well-Being Using Exploratory Structural Equation Modeling". Journal of Happiness Studies. 17 (5): 2023–2036. doi:10.1007/s10902-015-9683-z. S2CID 16022037.
- Bobowik, Magdalena; Basabe, Nekane; Páez, Darío (1 May 2015). "The bright side of migration: Hedonic, psychological, and social well-being in immigrants in Spain". Social Science Research. 51: 189–204. doi:10.1016/j.ssresearch.2014.09.011. PMID 25769861.
- Gallagher, Matthew W.; Lopez, Shane J.; Preacher, Kristopher J. (August 2009). "The Hierarchical Structure of Well-Being". Journal of Personality. 77 (4): 1025–1050. doi:10.1111/j.1467-6494.2009.00573.x. PMC 3865980. PMID 19558444.
- Keyes, Corey L. M.; Wissing, Marié; Potgieter, Johan P.; Temane, Michael; Kruger, Annamarie; van Rooy, Sinette (May 2008). "Evaluation of the mental health continuum–short form (MHC–SF) in setswana-speaking South Africans". Clinical Psychology & Psychotherapy. 15 (3): 181–192. doi:10.1002/cpp.572. PMID 19115439.
- Joshanloo, Mohsen; Lamers, Sanne M.A. (July 2016). "Reinvestigation of the factor structure of the MHC-SF in the Netherlands: Contributions of exploratory structural equation modeling". Personality and Individual Differences. 97: 8–12. doi:10.1016/j.paid.2016.02.089.
- Joshanloo, Mohsen (March 2016). "A New Look at the Factor Structure of the MHC-SF in Iran and the United States Using Exploratory Structural Equation Modeling". Journal of Clinical Psychology. 72 (7): 701–713. doi:10.1002/jclp.22287. PMID 26990960.
- "Mental Health in America - Youth Data". Mental Health America. Retrieved 2020-05-11.
- proof missing
- Lee, Francis S.; Heimer, Hakon; Giedd, Jay N.; Lein, Edward S.; Šestan, Nenad; Weinberger, Daniel R.; Casey, B.J. (31 October 2014). "Adolescent Mental Health—Opportunity and Obligation". Science. 346 (6209): 547–549. Bibcode:2014Sci...346..547L. doi:10.1126/science.1260497. PMC 5069680. PMID 25359951.
- Staikova, Ekaterina; Gomes, Hilary; Tartter, Vivien; McCabe, Allyssa; Halperin, Jeffrey M. (December 2013). "Pragmatic Deficits and Social Impairment in Children with ADHD". Journal of Child Psychology and Psychiatry. 54 (12): 1275–283. doi:10.1111/jcpp.12082. PMC 3648855. PMID 23682627.
- "NIMH » Child and Adolescent Mental Health". www.nimh.nih.gov. Retrieved 2020-04-14.
- Hinshaw, Stephen P. (July 2005). "The Stigmatization of Mental Illness in Children and Parents: Developmental Issues, Family Concerns, and Research Needs". Journal of Child Psychology and Psychiatry. 46 (7): 714–34. doi:10.1111/j.1469-7610.2005.01456.x. PMID 15972067.
- Wahl, Otto F. (June 2003). "Depictions of Mental Illnesses in Children's Media". Journal of Mental Health. 12 (3): 249–58. doi:10.1080/0963823031000118230. S2CID 145537429.
- Fox, C.; Buchanan‐Barrow, E.; Barrett, M. (January 2008). "Children's Understanding of Mental Illness: An Exploratory Study". Child: Care, Health and Development. 34 (1): 10–18. doi:10.1111/j.1365-2214.2007.00783.x. PMID 18171438.
- Feldman, David. "The Tragedy of Mental Illness Stigma". Psychology Today. Psychology Today. Retrieved 16 November 2020.
- Sueki (2013). "The Effect of Suicide-Related Internet Use on Users' Mental Health". Crisis. 34 (5): 348–353. doi:10.1027/0227-5910/a000201. PMID 23685338.
- "from The Los Angeles Times, March 15, 2001". www.szasz.com.
- Goodman, L.; Saxe, L.; Harvey, M. (1991). "Homelessness as psychological trauma. Broadening perspectives". The American Psychologist. 46 (11): 1219–1225. doi:10.1037//0003-066x.46.11.1219. ISSN 0003-066X. PMID 1772159.
- "Interventions to Improve the Health of the HomelessA Systematic Review | Request PDF". ResearchGate. Retrieved 2021-01-29.
- Goodman, Lisa; Saxe, Leonard; Harvey, Mary (November 1991). "Homelessness as psychological trauma. Broadening perspectives". The American Psychologist. 46 (11): 1219–1225. doi:10.1037//0003-066x.46.11.1219. PMID 1772159.
- "Interventions to Improve the Health of the HomelessA Systematic Review | Request PDF". ResearchGate. Retrieved 2021-01-29.
- Hwang, Stephen W.; Tolomiczenko, George; Kouyoumdjian, Fiona G.; Garner, Rochelle E. (1 November 2005). "Interventions to Improve the Health of the Homeless: A Systematic Review". American Journal of Preventive Medicine. 29 (4): 311–311.e75. doi:10.1016/j.amepre.2005.06.017. PMID 16242595.
- Riley, Andrew; Varner, Andrea; Ventevogel, Peter; Taimur Hasan, M. M.; Welton-Mitchell, Courtney (June 2017). "Daily stressors, trauma exposure, and mental health among stateless Rohingya refugees in Bangladesh". Transcultural Psychiatry. 54 (3): 304–331. doi:10.1177/1363461517705571. PMID 28540768. S2CID 4915988.
- Weare, Katherine (2000). Promoting Mental, Emotional and Social Health: A Whole School Approach. London: RoutledgeFalmer. p. 12. ISBN 978-0-415-16875-5.
- Office of the Deputy Prime Minister – Social Exclusion Unit: "Factsheet 1: Stigma and Discrimination on Mental Health Grounds". 2004.
- Barker, Phil (2010). Mental Health Ethics: The Human Context. Routledge. p. 146. ISBN 9781136881930.
- Yin, Yi; Zhang, Weijun; Hu, Zhenyu; Jia, Fujun; Li, Yafang; Xu, Huiwen; Zhao, Shuliang; Guo, Jing; Tian, Donghua; Qu, Zhiyong; Courvoisier, Delphine Sophie (26 September 2014). "Experiences of Stigma and Discrimination among Caregivers of Persons with Schizophrenia in China: A Field Survey". PLOS ONE. 9 (9): e108527. Bibcode:2014PLoSO...9j8527Y. doi:10.1371/journal.pone.0108527. PMC 4178170. PMID 25259732.
- Royal College of Psychiatrists: Changing Minds.
- Erin Blakemore (29 April 2019). "A play that hopes to smash the stigma surrounding mental illness". The Washington Post. Retrieved 23 June 2020.
- Rachael Myrow (2 May 2019). "'Manic Monologues' Seeks to Disrupt the Stigma Around Mental Illness". KQED. Retrieved 23 June 2020.
- "NAMI Presents: Cure Stigma". NAMI Presents: Cure Stigma. Retrieved 2018-09-15.
- Richards, PS; Bergin, AE (2000). Handbook of Psychotherapy and Religious Diversity. Washington, DC: American Psychological Association. p. 4. ISBN 978-1-55798-624-5.
- "Religious Trauma Syndrome". Recovering from Religion. Retrieved 2018-12-08.
- Merelli, Annalisa. "Jeff Sessions' new task force puts freedom of religion first". Quartz. Retrieved 2018-12-08.
- "How culture shapes your mind — and your mental illness - The Boston Globe". BostonGlobe.com. Retrieved 2018-12-08.
- Francis, Abraham P. (2014). Social Work in Mental Health: Contexts and Theories for Practice. SAGE Publications India. ISBN 978-93-5150-116-9.
- National Association of Social Workers, 2011
- "精神保健福祉士の受験資格を取得するための養成課程" [Psychiatric Social Worker Training Course]. Japan College of Social Work (in Japanese).
- Extremera, Natalio; Rey, Lourdes (29 September 2016). "Attenuating the Negative Impact of Unemployment: The Interactive Effects of Perceived Emotional Intelligence and Well-Being on Suicide Risk". PLOS ONE. 11 (9): e0163656. Bibcode:2016PLoSO..1163656E. doi:10.1371/journal.pone.0163656. PMC 5042532. PMID 27685996.
- Paul, Karsten (2009). "Unemployment impairs mental health: Meta-analysis". Journal of Vocational Behavior. 74 (3): 264–282. doi:10.1016/j.jvb.2009.01.001.
- "The World Mental Health Survey Initiative". Harvard Medical School. Retrieved 23 January 2016.
- Thornicroft, G (2007). "Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys". The Lancet. 370 (9590): 841–850. doi:10.1016/S0140-6736(07)61414-7. PMC 2847360. PMID 17826169.
- "20131 Stress". CAMH. Retrieved 2020-11-13.
- "Promotion & Prevention | Youth.gov". youth.gov. Retrieved 2020-11-17.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Miles, J., Espiritu, R. C., Horen, N. M., Sebian, J., & Waetzig, E. (2010). Washington, DC: Georgetown University, Center for Children and Human Development, National Technical Assistance Center for Children’s Mental Health
- Power, A (2010). "Transforming the Nation's Health: Next Steps in Mental Health Promotion". American Journal of Public Health. 100 (12): 2343–6. doi:10.2105/AJPH.2010.192138. PMC 2978180. PMID 20966366.
- National Prevention Council (16 June 2011), National Prevention Strategy (PDF), Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General, archived from the original (PDF) on 4 October 2011
- National Research Council; Institute of Medicine (2009). England, Mary Jane; Sim, Leslie J. (eds.). Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: National Academies Press. doi:10.17226/12565. ISBN 978-0-309-12178-1. PMID 25009931.
- "Your Staff's Mental Health Is a Workplace Safety Issue - Humanengineers". Humanengineers. 2017-06-20. Retrieved 2018-01-11.
- Jeronimus BF, Kotov R, Riese H, Ormel J (2016). "Neuroticism's prospective association with mental disorders: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants". Psychological Medicine. 46 (14): 2883–2906. doi:10.1017/S0033291716001653. PMID 27523506.
- Clark, Wayne; Welch, Stephanie N.; Berry, Sandra H.; Collentine, Ann M.; Collins, Rebecca; Lebron, Dorthy; Shearer, Amy L. (May 2013). "California's Historic Effort to Reduce the Stigma of Mental Illness: The Mental Health Services Act". American Journal of Public Health. 103 (5): 786–794. doi:10.2105/AJPH.2013.301225. PMC 3698820. PMID 23488486.
- "SIX WAYS SOCIAL MEDIA NEGATIVELY AFFECTS YOUR MENTAL HEALTH". 2019-10-10. Retrieved 2020-04-20.
- "Here's How to Look After Your Mental Health". 2020-04-20. Retrieved 2020-04-20.
- Kessler, Ronald C.; Demler, Olga; Frank, Richard G.; Olfson, Mark; Pincus, Harold Alan; Walters, Ellen E.; Wang, Philip; Wells, Kenneth B.; Zaslavsky, Alan M. (16 June 2005). "Prevalence and Treatment of Mental Disorders, 1990 to 2003". New England Journal of Medicine. 352 (24): 2515–2523. doi:10.1056/nejmsa043266. PMC 2847367. PMID 15958807.
- Ione Avila-Palencia (2018). "The effects of transport mode use on self-perceived health, mental health, and social contact measures: A cross-sectional and longitudinal study". Environment International. 120: 199–206. doi:10.1016/j.envint.2018.08.002. hdl:10044/1/62973. PMID 30098553.
- Rebar, Amanda L.; Stanton, Robert; Geard, David; Short, Camille; Duncan, Mitch J.; Vandelanotte, Corneel (3 July 2015). "A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations". Health Psychology Review. 9 (3): 366–378. doi:10.1080/17437199.2015.1022901. PMID 25739893. S2CID 24320503.
- Weinstein, Ali A.; Koehmstedt, Christine; Kop, Willem J. (November 2017). "Mental health consequences of exercise withdrawal: A systematic review". General Hospital Psychiatry. 49: 11–18. doi:10.1016/j.genhosppsych.2017.06.001. PMID 28625704.
- Flett J.A.M., Lie C., Riordan B.C., Thompson L.M., Conner T.S., Hayne H. (2017). "Sharpen Your Pencils: Preliminary Evidence that Adult Coloring Reduces Depressive Symptoms and Anxiety". Creativity Research Journal. 29 (4): 409–416. doi:10.1080/10400419.2017.1376505. S2CID 149346431.CS1 maint: multiple names: authors list (link)
- McCafferey, T; Edwards, J; Fannon, D (2009). "Is there a role for music therapy in the recovery approach in mental health?". The Arts in Psychotherapy. 38 (3): 185–189. doi:10.1016/j.aip.2011.04.006. hdl:10344/3362.
- The National Institute for Health and Care Excellence (NICE), Dramatherapy in Early Intervention in Psychosis, March 2019 https://www.nice.org.uk/sharedlearning/dramatherapy-in-early-intervention-in-psychosis
- Pommier, Elizabeth; Neff, Kristin D.; Tóth-Király, István (2020-01-01). "The Development and Validation of the Compassion Scale". Assessment. 27 (1): 21–39. doi:10.1177/1073191119874108. ISSN 1073-1911. PMID 31516024. S2CID 202569236.
- Shin, Na Young; Lim, Young-Jin (December 2019). "Contribution of self-compassion to positive mental health among Korean university students". International Journal of Psychology. 54 (6): 800–806. doi:10.1002/ijop.12527. ISSN 1464-066X. PMID 30206928.
- "SEL: What Are the Core Competence Areas and Where are they Promoted?". casel.org. Retrieved 2020-11-14.
- Department of Psychology, West University of Timisoara, Romania; Boncu, Alexandru; Costea, Iuliana; Department of Psychology, West University of Timisoara, Romania; Minulescu, Mihaela; National School of Political Studies and Public Administration, Bucharest, Romania (2017-12-31). "A meta-analytic study investigating the efficiency of socio-emotional learning programs on the development of children and adolescents" (PDF). Romanian Journal of Applied Psychology: 35–41. doi:10.24913/rjap.19.2.02.CS1 maint: multiple names: authors list (link)
- Goyal, Madhav; Singh, Sonal; Sibinga, Erica M. S.; Gould, Neda F.; Rowland-Seymour, Anastasia; Sharma, Ritu; Berger, Zackary; Sleicher, Dana; Maron, David D.; Shihab, Hasan M.; Ranasinghe, Padmini D.; Linn, Shauna; Saha, Shonali; Bass, Eric B.; Haythornthwaite, Jennifer A. (1 March 2014). "Meditation Programs for Psychological Stress and Well-being". JAMA Internal Medicine. 174 (3): 357–68. doi:10.1001/jamainternmed.2013.13018. PMC 4142584. PMID 24395196.
- Galla, Brian M.; O'Reilly, Gillian A.; Kitil, M. Jennifer; Smalley, Susan L.; Black, David S. (September 2014). "Community-Based mindfulness program for disease prevention and health promotion: Targeting stress reduction". American Journal of Health Promotion. 30 (1): 36–41. doi:10.4278/ajhp.131107-QUAN-567. PMID 25162319. S2CID 503591.
- Sharma M, Rush SE (Jul 2014). "Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review". J Evid Based Complementary Altern Med. 19 (4): 271–86. doi:10.1177/2156587214543143. PMID 25053754.
- Khoury B, Lecomte T, Fortin G, et al. (Aug 2013). "Mindfulness-based therapy: a comprehensive meta-analysis". Clin Psychol Rev. 33 (6): 763–71. doi:10.1016/j.cpr.2013.05.005. PMID 23796855.
- Chiesa A (Apr 2014). "Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence". Subst Use Misuse. 49 (5): 492–512. doi:10.3109/10826084.2013.770027. PMID 23461667. S2CID 34990668.
- Garland EL (Jan 2014). "Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface". Front Psychiatry. 4 (173): 173. doi:10.3389/fpsyt.2013.00173. PMC 3887509. PMID 24454293.

- Tang YY, Posner MI (Jan 2013). "Special issue on mindfulness neuroscience". Social Cognitive and Affective Neuroscience. 8 (1): 1–3. doi:10.1093/scan/nss104. PMC 3541496. PMID 22956677.
- Posner MI, Tang YY, Lynch G (2014). "Mechanisms of white matter change induced by meditation training". Frontiers in Psychology. 5 (1220): 297–302. doi:10.3389/fpsyg.2014.01220. PMC 4209813. PMID 25386155.

- Holzel BK, Lazar SW, et al. (Nov 2011). "How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective". Perspectives on Psychological Science. 6 (6): 537–559. doi:10.1177/1745691611419671. PMID 26168376. S2CID 2218023.
- Jayaram, Thimmapuram; Robert, Pargament; Kedesha, Sibliss; Rodney, Grim; Rosana, Risques; Erik, Toorens (31 March 2017). "Effect of heartfulness meditation on burnout, emotional wellness, and telomere length in health care professionals". Journal of Community Hospital Internal Medicine Perspectives. 7 (1): 21–27. doi:10.1080/20009666.2016.1270806. PMC 5463663. PMID 28634520.
- Schmidtman, Emily A. (1992). "Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders". American Journal of Psychiatry. 149 (7): 936–943. CiteSeerX 10.1.1.474.4968. doi:10.1176/ajp.149.7.936. PMID 1609875.
- Walkadean, Chad (22 June 2020). "Mental fitness - a gamechanger". Gotcha4Life mental health and suicide prevention.
- Rosmarin, David H.; Pirutinsky, Steven; Auerbach, Randy P.; Björgvinsson, Thröstur; Bigda-Peyton, Joseph; Andersson, Gerhard; Pargament, Kenneth I.; Krumrei, Elizabeth J. (July 2011). "Incorporating spiritual beliefs into a cognitive model of worry". Journal of Clinical Psychology. 67 (7): 691–700. doi:10.1002/jclp.20798. PMID 21480226.
- Demyttenaere, K.; Bruffaerts, R.; Posada-Villa, J.; Gasquet, I.; Kovess, V.; Lepine, J. P.; Angermeyer, M. C.; Bernert, S.; De Girolamo, G.; Morosini, P.; Polidori, G.; Kikkawa, T.; Kawakami, N.; Ono, Y.; Takeshima, T.; Uda, H.; Karam, E. G.; Fayyad, J. A.; Karam, A. N.; Mneimneh, Z. N.; Medina-Mora, M. E.; Borges, G.; Lara, C.; De Graaf, R.; Ormel, J.; Gureje, O.; Shen, Y.; Huang, Y.; Zhang, M.; et al. (2 June 2004). "Prevalence, Severity, and Unmet Need for Treatment of Mental Disorders in the World Health Organization World Mental Health Surveys". JAMA. 291 (21): 2581–90. doi:10.1001/jama.291.21.2581. PMID 15173149.
- Wang, Philip S.; Berglund, Patricia; Olfson, Mark; Pincus, Harold A.; Wells, Kenneth B.; Kessler, Ronald C. (1 June 2005). "Failure and Delay in Initial Treatment Contact After First Onset of Mental Disorders in the National Comorbidity Survey Replication". Archives of General Psychiatry. 62 (6): 603–13. doi:10.1001/archpsyc.62.6.603. PMID 15939838.
- Ogletree, Cordaye; Grimm, Geoffrey; Martin, Laurie; Hansen, Michael; Tanielian, Terri (2016). "Supporting the Mental Health Needs of Veterans in the Metro Detroit Area". Rand Health Quarterly. 6 (1): 15. doi:10.7249/RR1346. ISBN 978-0-8330-9257-1. PMC 5158279. PMID 28083443.
- U.S. Public Health Service (1999). "Overview of Mental Health Services". Mental Health: A Report of the Surgeon General. Archived from the original on 11 February 2012. Retrieved 19 February 2012.
- Dix, D (April 2006). "'I Tell What I Have Seen'—The Reports of Asylum Reformer Dorothea Dix. 1843". American Journal of Public Health. 96 (4): 622–624. doi:10.2105/ajph.96.4.622. PMC 1470564. PMID 16551962.
- Luchins, AS (November 1989). "Moral Treatment in Asylums and General Hospitals in 19th-Century America". The Journal of Psychology. 123 (6): 585–607. doi:10.1080/00223980.1989.10543013. PMID 2691669.
- Beers, Clifford Whittingham (8 April 2004) [1908]. A Mind That Found Itself: An Autobiography. Project Gutenberg.
- Cohen, Sol (1983). "The Mental Hygiene Movement, the Development of Personality and the School: The Medicalization of American Education". History of Education Quarterly. 23 (2): 123–149. doi:10.2307/368156. JSTOR 368156. PMID 11614585.
- Koyanagi, C; Goldman, H (September 1991). "The quiet success of the national plan for the chronically mentally ill". Hospital & Community Psychiatry. 42 (9): 899–905. doi:10.1176/ps.42.9.899. PMID 1743659.
- Torrey, E. Fuller (10 May 2005). "Deinstitutionalization: A Psychiatric "Titanic"". Frontline. WGBH Educational Foundation. Archived from the original on 25 May 2005. Excerpts from Torrey, E. Fuller (1997). Out of the Shadows: Confronting America's Mental Illness Crisis. New York: John Wiley & Sons. ISBN 978-0471161615.
- Koyanagi, Chris (August 2007), Learning From History: Deinstitutionalization of People with Mental Illness As Precursor to Long-Term Care Reform (PDF), Menlo Park, CA: Kaiser Family Foundation, pp. 1–22
- "Prevention of Mental Disorders". National Institute of Mental Health. National Institute of Mental Health. Archived from the original on 5 July 2015. Retrieved 7 August 2015.
Further reading
External links
| Wikiquote has quotations related to: Mental health |
| Library resources about Mental health |
- "Mental health and substance abuse". WHO Regional Office for the Eastern Mediterranean.
- National Institute of Mental Health (United States)
- Health-EU Portal Mental Health in the EU
- Mental Health Department of Health (United Kingdom)