Limbic encephalitis
Limbic encephalitis is a form of encephalitis, a disease characterized by inflammation of the brain.[1] Limbic encephalitis is caused by autoimmunity: an abnormal state where the body produces antibodies against itself. Some cases are associated with cancer and some are not.[1] Although the disease is known as "limbic" encephalitis, it is seldom limited to the limbic system and post-mortem studies usually show involvement of other parts of the brain.[2][3][4] The disease was first described by Brierley and others in 1960 as a series of three cases. The link to cancer was first noted in 1968[3] and confirmed by later investigators.[5]
| Limbic encephalitis | |
|---|---|
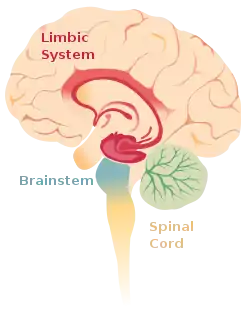 | |
| The limbic system within the brain. | |
| Specialty | Neurology |
The majority of cases of limbic encephalitis are associated with a tumor (diagnosed or undiagnosed). In cases caused by tumor, recovery can only occur following complete removal of the tumor, which is not always possible. Limbic encephalitis is classified according to the auto-antibody that causes the disease. The most common types are:
- Anti-Hu, which is associated with small-cell carcinoma of the lungs.
- Anti-Ma2, associated with germ-cell tumours of the testis.
- Anti-NMDAR, associated with tumors of the ovaries, commonly teratomas.
Since 1999, following the publication of a case report of a 15-year-old teenager of Indian descent from South Africa who developed subacute memory loss subsequent to herpes simplex type 1 encephalitis,[6] similar cases of non-paraneoplastic LE have been described, as has its association with auto-antibodies and response to steroid.[7][8] Limbic encephalitis associated with voltage-gated potassium channel antibodies (VGKC-Abs)[9] may frequently be non-paraneoplastic.[10] A recent study of 15 cases of limbic encephalitis found raised VGKC-Abs associated with non-paraneoplastic disorders and remission following immunosuppressive treatment.[11]
Classification
Limbic encephalitis is broadly grouped into two types: paraneoplastic limbic encephalitis and non-paraneoplastic limbic encephalitis.
- Paraneoplastic limbic encephalitis (PNLE) is caused by cancer or tumor, and may be treated by removal of the tumor.
- Non-paraneoplastic limbic encephalitis (NPLE) is not associated with cancer. More common than PNLE, it is caused by an infection, auto-immune disorder, or other condition that may never be identified.[12]
Symptoms and signs
Symptoms develop over days or weeks. The subacute development of short-term memory deficits is considered the hallmark of this disease,[1] but this symptom is often overlooked, because it is overshadowed by other more obvious symptoms such as headache, irritability, sleep disturbance, delusions, hallucinations, agitation, seizures and psychosis, or because the other symptoms mean the patient has to be sedated, and it is not possible to test memory in a sedated patient.
Cause
Limbic encephalitis is associated with an autoimmune reaction.[1] In non-paraneoplastic limbic encephalitis, this is typically due to infection (commonly herpes simplex virus) or as a systemic autoimmune disorder.[13] Limbic encephalitis associated with cancer or tumors is called paraneoplastic limbic encephalitis.
Diagnosis
The diagnosis of limbic encephalitis is extremely difficult and it is usual for the diagnosis to be delayed for weeks. The key diagnostic test (detection of specific auto-antibodies in cerebrospinal fluid) is not routinely offered by most immunology laboratories. Some of the rarer auto-antibodies (e.g., NMDAR) have no commercially available assay and can only be measured by a very small number of research laboratories worldwide, further delaying diagnosis by weeks or months. Most patients with limbic encephalitis are initially diagnosed with herpes simplex encephalitis, because the two syndromes cannot be distinguished clinically.[1] HHV-6 (human herpes virus 6) encephalitis is also clinically indistinguishable from limbic encephalitis.[1]
There are two sets of diagnostic criteria used. The oldest are those proposed by Gultekin et al. in 2000.[14]
| Gultekin criteria |
|---|
| EITHER, Pathological demonstration of limbic encephalitis |
OR, All four of:
|
A revised set of criteria were proposed by Graus and Saiz in 2005.[15]
| Graus and Saiz criteria |
|---|
All four of
|
The main distinction between the two sets of criteria is whether or not the detection of a paraneoplastic antibody is needed for diagnosis.
Antibodies against intracellular neuronal antigens
The main antibodies within this group are those against Hu, Ma2, CV2, amphiphysin and Ri. The syndrome of anti-Ma2 encephalitis may be clinically mistaken for Whipple's disease.[16]
Antibodies against cell membrane antigens
The main antibodies within this group are those against anti-N-methyl-D-aspartate receptors (NMDAR) and the voltage-gated potassium channel-complex (VGKC-complex). Anti-NMDAR encephalitis is strongly associated with benign tumours of the ovary (usually teratomas or dermoid cysts). Anti-VGKC-complex encephalitis is most often not associated with tumours.
Patients with NMDAR encephalitis are frequently young women who present with fever, headache and fatigue. This is often misdiagnosed as influenza, but progresses to severe behavioural and personality disturbance, delusions, paranoia and hallucinations.[17] Patients may therefore initially be admitted to a psychiatric ward for acute psychosis or schizophrenia. The disease then progresses to catatonia, seizures and loss of consciousness. The next stage is hypoventilation (inadequate breathing) requiring intubation, orofacial dyskinesia and autonomic instability (dramatic fluctuations in blood pressure, temperature and heart rate).[18]
Cerebrospinal fluid (CSF)
Examination of cerebrospinal fluid (CSF) shows elevated numbers of lymphocytes (but usually < 100 cells/μl); elevated CSF protein (but usually <1.5 g/l), normal glucose, elevated IgG index and oligoclonal bands. Patients with antibodies to voltage-gated potassium channels may have a completely normal CSF examination.[19][20][21]
Neuroimaging
Brain MRI is the mainstay of initial investigation pointing to limbic lobe pathology revealing increased T2 signal involving one or both temporal lobes in most cases.[22][14]
Serial MRI in LE starts as an acute disease with uni- or bilateral swollen temporomesial structures that are hyperintense on fluid attenuation inversion recovery and T2-weighted sequences. Swelling and hyperintensity may persist over months to years, but in most cases progressive temporomesial atrophy develops.[23]
PET-CT is not an essential investigation but can help in suspected cases with MRI negative for early diagnosis.[24]
Neuro-electrophysiology
EEG is mostly nonspecific slowing and epileptiform activity arising from temporal lobes.[14]
Treatment
Limbic encephalitis is a rare condition with no randomised-controlled trials to guide treatment. Treatments that have been tried include intravenous immunoglobulin, plasmapheresis, corticosteroids, cyclophosphamide and rituximab.[1]
If an associated tumour is found, then recovery is not possible until the tumour is removed. Unfortunately, this is not always possible, especially if the tumour is malignant and advanced.
History
| Clinical Features | Pathology | Year | Syndromes |
| Subacute onset of episodic memory impairment, disorientation and agitation, commonly associated with seizures, hallucinations, sleep disturbance | Medial temporal lobe inflammation | 1960 | Subacute encephalitis of later adult life mainly affecting the limbic areas[2] |
| 1968 | Limbic Encephalitis association with Carcinoma[25][2] | ||
| 2008 | Paraneoplastic LE with Lung Carcinoma, thymoma,[26] | ||
| 2002 | Non Paraneoplastic LE[6] |
References
- Tüzün E, Dalmau J (2007). "Limbic encephalitis and variants: classification, diagnosis and treatment". The Neurologist. 13 (5).
- Brierley JB, Corsellis JA, Hierons R, et al. (1960). "Subacute encephalitis of later adult life. Mainly affecting the limbic areas". Brain. 83 (3): 357–368. doi:10.1093/brain/83.3.357.
- Corsellis JA, Goldberg GJ, Norton AR (1968). ""Limbic encephalitis" and its association with carcinoma". Brain. 91 (3): 481–496. doi:10.1093/brain/91.3.481. PMID 5723018.
- Bakheit AM, Kennedy PG, Behan PO (1990). "Paraneoplastic limbic encephalitis: clinico-pathological correlations". J Neurol Neurosurg Psychiatry. 53 (12): 1084–1088. doi:10.1136/jnnp.53.12.1084. PMC 488321. PMID 1963440.
- Henson RA, Hoffman HL, Urich H (1965). "Encephalomyelitis with carcinoma". Brain. 88 (3): 449–464. doi:10.1093/brain/88.3.449.
- Mori, Masahiro; Kuwabara, Satoshi; Yoshiyama, Mitsuharu; Kanesaka, Toshihide; Ogata, Tsuyoshi; Hattori, Takamichi (2002-09-15). "Successful immune treatment for non-paraneoplastic limbic encephalitis". Journal of the Neurological Sciences. 201 (1–2): 85–88. doi:10.1016/s0022-510x(02)00188-0. ISSN 0022-510X. PMID 12163199.
- Watanabe, Yasuhiro; Shimizu, Yasutaka; Ooi, Shinji; Tanaka, Keiko; Inuzuka, Takashi; Nakashima, Kenji (2003-05-01). "Steroid-responsive limbic encephalitis". Internal Medicine. 42 (5): 428–432. doi:10.2169/internalmedicine.42.428. ISSN 0918-2918. PMID 12793715.
- Lang, Pierre Olivier; Sellal, François (2008-05-01). "[Non-paraneoplastic limbic encephalitis revealed by anterograde amnesia]". Presse Médicale. 37 (5 Pt 1): 775–782. doi:10.1016/j.lpm.2007.11.013. ISSN 0755-4982. PMID 18261871.
- Buckley, C.; Oger, J.; Clover, L.; Tüzün, E.; Carpenter, K.; Jackson, M.; Vincent, A. (2001-07-01). "Potassium channel antibodies in two patients with reversible limbic encephalitis". Annals of Neurology. 50 (1): 73–78. doi:10.1002/ana.1097. ISSN 0364-5134. PMID 11456313.
- Schott, J. M.; Harkness, K.; Barnes, J.; della Rocchetta, A. Incisa; Vincent, A.; Rossor, M. N. (2003-04-12). "Amnesia, cerebral atrophy, and autoimmunity". Lancet. 361 (9365): 1266. doi:10.1016/s0140-6736(03)12983-2. ISSN 0140-6736. PMID 12699955.
- Pozo-Rosich, Patricia; Clover, Linda; Saiz, Albert; Vincent, Angela; Graus, Francesc (2003-10-01). "Voltage-gated potassium channel antibodies in limbic encephalitis". Annals of Neurology. 54 (4): 530–533. doi:10.1002/ana.10713. ISSN 0364-5134. PMID 14520669.
- "Limbic encephalitis". The Encephalitis Society. Retrieved 2017-12-23.
- Anderson, N. E.; Barber, P. A. (September 2008). "Limbic encephalitis - a review". Journal of Clinical Neuroscience. 15 (9): 961–971. doi:10.1016/j.jocn.2007.12.003. ISSN 0967-5868. PMID 18411052.
- Gultekin SH, Rosenfeld MR, Voltz R, et al. (2000). "Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients". Brain. 123 (7): 1481–1494. doi:10.1093/brain/123.7.1481. PMID 10869059.
- Graus F, Saiz A (2005). "Limbic encephalitis: a probably under-recognized syndrome". Neurologia. 20: 24–30.
- Castle J, Sakonju A, Dalmau J, et al. (2006). "Anti-Ma2-associated encephalitis with normal FDG-PET: a case of pseudo-Whipple's disease". Nat Clin Pract Neurol. 2 (10): 566–572. doi:10.1038/ncpneuro0287. PMID 16990830.
- Koide R, Shimizu T, Koike K, et al. (2007). "EFA6A-like antibodies in paraneoplastic encephalitis associated with immature ovarian teratoma: a case report". J Neurooncol. 81 (1): 71–74. doi:10.1007/s11060-006-9200-7. PMID 16807779.
- Dalmau J, Tuzun E, Wu HY, et al. (2007). "Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma". Ann Neurol. 61 (1): 25–36. doi:10.1002/ana.21050. PMC 2430743. PMID 17262855.
- Buckley C, Oger J, Clover L, et al. (2001). "Potassium channel antibodies in two patients with reversible limbic encephalitis". Ann Neurol. 50: 73–78. doi:10.1002/ana.1097. PMID 11456313.
- Vincent A, Buckley C, Schott JM, et al. (2004). "Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis". Brain. 127 (3): 701–712. doi:10.1093/brain/awh077. PMID 14960497.
- Thieben MJ, Lennon VA, Boeve BF, et al. (2004). "Potentially reversible auto-immune limbic encephalitis with neuronal potassium channel antibody". Neurology. 62 (7): 1177–1182. doi:10.1212/01.WNL.0000122648.19196.02.
- Nicholas, D (2003). "Clinical, Magnetic Resonance Imaging, and 7Electroencephalographic Findings in Paraneoplastic Limbic Encephalitis". Mayo Clinic Proceedings. 78 (11): 1363–1368. doi:10.4065/78.11.1363. PMID 14601695.
- Horst, Urbach (2006). "Serial MRI of limbic encephalitis". Neuroradiology. 48 (6): 380–386. doi:10.1007/s00234-006-0069-0. PMID 16586118.
- Cózar Santiago, Maria Del Puig; Sanchez Jurado, Raul; Sanz Llorens, Rut; Aguilar Barrios, Jose Enrique; Ferrer Rebolleda, Jose (2016-02-01). "Limbic Encephalitis Diagnosed With 18F-FDG PET/CT". Clinical Nuclear Medicine. 41 (2): e101–103. doi:10.1097/RLU.0000000000001076. ISSN 1536-0229. PMID 26571448.
- Corsellis, JA (1968). "Limbic encephalitis" and its association with carcinoma". Brain. 91 (3): 481–96. doi:10.1093/brain/91.3.481. PMID 5723018.
- Dalmau, Josep; Gleichman, Amy J.; Hughes, Ethan G.; Rossi, Jeffrey E.; Peng, Xiaoyu; Lai, Meizan; Dessain, Scott K.; Rosenfeld, Myrna R.; Balice-Gordon, Rita (2008-12-01). "Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies". The Lancet. Neurology. 7 (12): 1091–1098. doi:10.1016/S1474-4422(08)70224-2. ISSN 1474-4422. PMC 2607118. PMID 18851928.
External links
| Classification | |
|---|---|
| External resources |
