Progressive supranuclear palsy
Progressive supranuclear palsy (PSP) is a late-onset degenerative disease involving the gradual deterioration and death of specific volumes of the brain.[1][2] The condition leads to symptoms including loss of balance, slowing of movement, difficulty moving the eyes, and dementia.[1] PSP may be mistaken for other neurodegenerative diseases such as Parkinson's and Alzheimer's. The cause of the condition is uncertain, but involves accumulation of tau protein within the brain. Medications such as levodopa and amantadine may be useful in some cases.[1]
| Progressive supranuclear palsy | |
|---|---|
| Other names | Steele–Richardson–Olszewski syndrome, frontotemporal dementia with parkinsonism |
| Specialty | Neurology |
| Symptoms | Impaired balance, slowed movements, difficulty moving eyes, dementia |
| Usual onset | 60–70 years |
| Causes | Unknown |
| Differential diagnosis | Parkinson's disease, corticobasal degeneration, FTDP-17, Alzheimer's disease |
| Treatment | Medication, physical therapy, occupational therapy |
| Medication | Levodopa, amantadine |
| Prognosis | 7–10 years after diagnosis. |
| Frequency | 6 per 100,000 |
PSP affects about six people per 100,000.[1] The first symptoms typically occur in persons aged 60–70 years. Males are slightly more likely to be affected than females.[1] No association has been found between PSP and any particular race, location, or occupation.[1]
Signs and symptoms
The initial symptoms in two-thirds of cases are loss of balance, lunging forward when mobilizing, fast walking, bumping into objects or people, and falls.[3] Dementia symptoms are also initially seen in about one in five cases.[4]
Other common early symptoms are changes in personality, general slowing of movement, and visual symptoms. The most common behavioural symptoms in patients with PSP include apathy, disinhibition, anxiety, and dysphoria.[4]
Later symptoms and signs are dementia (typically including loss of inhibition and ability to organize information), slurring of speech, difficulty swallowing, and difficulty moving the eyes, particularly in the vertical direction. The latter accounts for some of the falls experienced by these patients, as they find it difficult to look up or down.[5]
Some of the other signs are poor eyelid function, contracture of the facial muscles, a backward tilt of the head with stiffening of the neck muscles, sleep disruption, urinary incontinence, and constipation.[5]
The visual symptoms are of particular importance in the diagnosis of this disorder. Patients typically complain of difficulty reading due to the inability to look down well. Notably, the ophthalmoparesis experienced by these patients mainly concerns voluntary eye movement and the inability to make vertical saccades, which is often worse with downward saccades. Patients tend to have difficulty looking down (a downgaze palsy) followed by the addition of an upgaze palsy. This vertical gaze paresis will correct when the examiner passively rolls the patient's head up and down as part of a test for the oculocephalic reflex. Involuntary eye movement, as elicited by Bell's phenomenon, for instance, may be closer to normal. On close inspection, eye movements called "square-wave jerks" may be visible when the patient fixes at distance. These are fine movements, that can be mistaken for nystagmus, except that they are saccadic in nature, with no smooth phase. Although healthy individuals also make square-wave jerk movements, PSP patients make slower square-wave jerk movements, with smaller vertical components.[6] Assessment of these square-wave jerks and diminished vertical saccades is especially useful for diagnosing progressive supranuclear palsy, because these movements set PSP patients apart from other parkinsonian patients.[6] Difficulties with convergence (convergence insufficiency), where the eyes come closer together while focusing on something near, like the pages of a book, is typical. Because the eyes have trouble coming together to focus at short distances, the patient may complain of diplopia (double vision) when reading.[5]
A characteristic facial appearance known as “procerus sign”, with a wide-eye stare, furrowing of forehead with a frowning expression and deepening of other facial creases is diagnostic of PSP.[7]
Cardinal manifestations:
- Supranuclear ophthalmoplegia
- Neck dystonia
- Parkinsonism
- Pseudobulbar palsy
- Behavioral and cognitive impairment
- Imbalance and walking difficulty
- Frequent falls
Cause
The cause of PSP is unknown. Fewer than 1% of those with PSP have a family member with the same disorder. A variant in the gene for tau protein called the H1 haplotype, located on chromosome 17 (rs1800547), has been linked to PSP.[8] Nearly all people with PSP received a copy of that variant from each parent, but this is true of about two-thirds of the general population. Therefore, the H1 haplotype appears to be necessary but not sufficient to cause PSP. Other genes, as well as environmental toxins, are being investigated as other possible contributors to the cause of PSP.
Additionally, the H2 haplotype, combined with vascular dysfunction, seems to be a factor of progressive supranuclear palsy.[9]
Besides tauopathy, mitochondrial dysfunction seems to be a factor involved in PSP. Especially, mitochondrial complex I inhibitors (such as acetogenins and quinolines contained in Annonaceae, as well as rotenoids) are implicated in PSP-like brain injuries.[10]
Pathophysiology
The affected brain cells are both neurons and glial cells. The neurons display neurofibrillary tangles (NFTs), which are clumps of tau protein, a normal part of a brain cell's internal structural skeleton. These tangles are often different from those seen in Alzheimer's disease, but may be structurally similar when they occur in the cerebral cortex.[11] Their chemical composition is usually different, however, and is similar to that of tangles seen in corticobasal degeneration.[12] Tufts of tau protein in astrocytes, or tufted astrocytes, are also considered diagnostic. Unlike globose NFTs, they may be more widespread in the cortex.[13] Lewy bodies are seen in some cases, but whether this is a variant or an independent co-existing process is not clear, and in some cases, PSP can coexist with corticobasal degeneration, Parkinson's, and/or Alzheimer's disease, particularly with older patients.[14][15][16][17][18]
The principal areas of the brain affected are the:
- basal ganglia, particularly the subthalamic nucleus, substantia nigra, and globus pallidus
- brainstem, particularly the portion of the midbrain where "supranuclear" eye movement resides, as well as dopaminergic nuclei.
- cerebral cortex, particularly that of the frontal lobes and the limbic system (similarly to frontotemporal degeneration)
- dentate nucleus of the cerebellum
- spinal cord, particularly the area where some control of the bladder and bowel resides
Some consider PSP, corticobasal degeneration, and frontotemporal dementia to be variations of the same disease.[19][20] Others consider them separate diseases.[21][22][23] PSP has been shown occasionally to co-exist with Pick's disease.[24]
Diagnosis
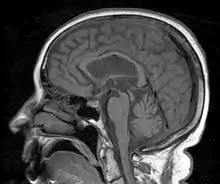
MRI is often done to diagnose PSP. MRI may show atrophy in the midbrain with preservation of the pons giving a "hummingbird" sign appearance and Mickey Mouse sign.[26]
Types
Based on the pathological findings in confirmed cases of PSP, it is divided into the following categories:
- classical Richardson syndrome (PSP-RS)
- PSP-parkinsonism (PSP-P) and PSP-pure akinesia with gait freezing (PSP-PAGF)
- frontal PSP, PSP-corticobasal syndrome (PSP-CBS), PSP-behavioural variant of frontotemporal dementia (PSP-bvFTD) and PSP-progressive non-fluent aphasia (PSP-PNFA)[27]
- PSP-C
- PSP induced by Annonaceae[28]
Richardson syndrome is characterized by the typical features of PSP. In PSP-P features of Parkinson’s Disease overlap with the clinical presentation of PSP and follows a more benign course. In both PSP-P and PSP- PAGF distribution of abnormal tau is relatively restricted to the brain stem. Frontal PSP initially presents with behavioral and cognitive symptoms, with or without ophthalmoparesis and then evolve into typical PSP.[7] The phenotypes of PSP-P and PSP-PAGF are sometimes referred as the ‘brain stem’ variants of PSP, as opposed to the ‘cortical’ variants which present with predominant cortical features including PSP-CBS, PSP-bvFTD, and PSP-PNFA.[29] Cerebellar ataxia as the predominant early presenting feature is increasingly recognized as a very rare subtype of PSP (PSP-C) which is associated with severe neuronal loss with gliosis and higher densities of coiled bodies in the cerebellar dentate nucleus.[30]
Differential diagnosis
PSP is frequently misdiagnosed as Parkinson's disease because they both involve slowed movements and gait difficulty, with PSP being one of a collection of diseases referred to as Parkinson plus syndromes. Both Parkinson's and PSP have an onset in late middle age and involve slowing and rigidity of movement. However, several distinguishing features exist. Tremor is very common with Parkinson's, but rare with PSP. Speech and swallowing difficulties are more common and severe with PSP and the abnormal eye movements of PSP are essentially absent with PD.[31] A poor response to levodopa along with symmetrical onset can also help differentiate PSP from PD.[32] Patients with the Richardson variant of PSP tend to have an upright posture or arched back, as opposed to the stooped-forward posture of other Parkinsonian disorders, although PSP-Parkinsonism (see below) can demonstrate a stooped posture.[33] Early falls are also more common with PSP, especially with Richardson syndrome.[34]
PSP can also be misdiagnosed as Alzheimer's disease because of the behavioral changes.[35]
Chronic traumatic encephalopathy shows many similarities with PSP.
Current management
Supportive therapies
No cure for PSP is known, and management is primarily supportive. PSP cases are often split into two subgroups, PSP-Richardson, the classic type, and PSP-Parkinsonism, where a short-term response to levodopa can be obtained.[36] Dyskinesia is an occasional but rare complication of treatment.[37] Amantadine is also sometimes helpful.[38] After a few years the Parkinsonian variant tends to take on Richardson features.[39] Other variants have been described.[40][41][42][43] Botox can be used to treat neck dystonia and blepharospasm, but this can aggravate dysphagia.[44]
Two studies have suggested that rivastigmine may help with cognitive aspects, but the authors of both studies have suggested a larger sampling be used.[45][46] There is some evidence that the hypnotic zolpidem may improve motor function and eye movements, but only from small-scale studies.[47][48]
Rehabilitation
Patients with PSP usually seek or are referred to occupational therapy, speech-language pathology for motor speech changes typically a spastic-ataxic dysarthria, and physical therapy for balance and gait problems with reports of frequent falls.[49] Evidence-based approaches to rehabilitation in PSP are lacking and, currently, the majority of research on the subject consists of case reports involving only a small number of patients.
Case reports of rehabilitation programs for patients with PSP generally include limb-coordination activities, tilt-board balancing, gait training, strength training with progressive resistive exercises, and isokinetic exercises and stretching of the neck muscles.[49] While some case reports suggest that physiotherapy can offer improvements in balance and gait of patients with PSP, the results cannot be generalized across all PSP patients, as each case report only followed one or two patients.[49] The observations made from these case studies can be useful, however, in helping to guide future research concerning the effectiveness of balance and gait training programs in the management of PSP.
Individuals with PSP are often referred to occupational therapists to help manage their condition and to help enhance their independence. This may include being taught to use mobility aids.[50][51] Due to their tendency to fall backwards, the use of a walker, particularly one that can be weighted in the front, is recommended over a cane.[50] The use of an appropriate mobility aid helps to decrease the individual’s risk of falls and makes them safer to ambulate independently in the community.[51] Due to their balance problems and irregular movements, individuals need to spend time learning how to safely transfer in their homes and in the community.[50] This may include rising from and sitting in chairs safely.[51]
Due to the progressive nature of this disease, all individuals eventually lose their ability to walk and will need to progress to using a wheelchair.[50] Severe dysphagia often follows, and at this point death is often a matter of months.[36]
Experimental treatments
Drugs targeting the tau protein offer a promising avenue for therapeutic intervention. The growth factor davunetide was recently trialed in patients to prevent hyperphosphorylated, insoluble forms of tau, however it was unable to show efficacy possibly due insufficient CNS penetration.[52] Antisense therapy has shown efficacy in several other human neurodegenerative disorders and has recently been shown to substantially extend lifespan in animals with PSP.[53] Biogen and Ionis Pharmaceuticals currently are investigating a tau-lowering antisense therapy for Alzheimer's disease and frontotemporal dementia which could also have applicability to PSP.[54]
Prognosis
No effective treatment or cure has been found for PSP, although some of the symptoms can respond to nonspecific measures. The poor prognosis is predominantly attributed to the serious impact this condition has on the quality of life.[3] The average age at symptoms onset is 63 and survival from onset averages seven years with a wide variance.[55] Pneumonia is a frequent cause of death.[56]
History
In 1877, Charcot described a 40-year-old woman who had rigid-akinetic parkinsonism, neck dystonia, dysarthria, and eye-movement problems. Chavany and others reported the clinical and pathologic features of a 50-year-old man with a rigid and akinetic form of parkinsonism with postural instability, neck dystonia, dysarthria, and staring gaze in 1951. Progressive supranuclear palsy was first described as a distinct disorder by neurologists John Steele, John Richardson, and Jerzy Olszewski in 1963.[1][57][58][59] They recognized the same clinical syndrome in 8 patients and described the autopsy findings in 6 of them in 1963.
Progressive supranuclear palsy was not a “new” disease in 1963, as 22 well-documented case reports had been identified in the neurologic literature between 1877 and 1963.[60] The unique frontal lobe cognitive changes of progressive supranuclear palsy (apathy, loss of spontaneity, slowing of thought processes, and loss of executive functions) were first described by Albert and colleagues in 1974.[61]
Societies
There are several organizations around the world that support PSP patients and the research into PSP and related diseases, such as corticobasal degeneration (CBD) and multiple system atrophy (MSA).
- Canada: PSP Society of Canada, a federally registered non-profit organization which serves patients and families dealing with PSP, CBD and MSA, set up in 2017 through the help of CurePSP in the USA[62]
- France: Association PSP France, a nonprofit patient association set up in 1996 through the help of PSPA in the UK. It also gives support to French speaking patients in Quebec, Morocco, Algeria, Belgium and Lebanon[63]
- UK: PSPA, a national charity for information, patient support and research of PSP and CBD, set up in 1995[64]
- Ireland: PSPAI, a body which aims to get PSP better known[65]
- US: CurePSP, a nonprofit organization for promoting awareness, care and research of PSP, CBD, MSA "and other prime of life neurodegenerative diseases"[66]
In popular culture
In the 2020 American musical comedy-drama television series, Zoey's Extraordinary Playlist, the title character's father (Mitch Clarke, played by Peter Gallagher) has PSP and dies in the final episode of the first season.[67]
American singer Linda Ronstadt was diagnosed with PSP in 2019, subsequent to an initial diagnosis of Parkinson's disease in 2014.[68]
See also
- Lytico-bodig disease (Parkinsonism-Dementia Complex of Guam)
- Annonacin
References
- Golbe LI (April 2014). "Progressive supranuclear palsy". Seminars in Neurology. 34 (2): 151–9. doi:10.1055/s-0034-1381736. PMID 24963674.
- "ICD-11 - Mortality and Morbidity Statistics". icd.who.int.
- Daroff RB, Fenichel GM,Jankovic J,Mazziotta JC (2012). Bradley's neurology in clinical practice (Sixth ed.). Philadelphia: Elsevier Saunders. p. 1778. ISBN 978-1-4377-0434-1.CS1 maint: multiple names: authors list (link)
- Finger EC (April 2016). "Frontotemporal Dementias". Continuum. 22 (2 Dementia): 464–89. doi:10.1212/CON.0000000000000300. PMC 5390934. PMID 27042904.
- "Symptoms - Progressive supranuclear palsy". NHS. NHS. Retrieved 19 January 2021.
- Alexander RG, Macknik SL, Martinez-Conde S (2018). "Microsaccade Characteristics in Neurological and Ophthalmic Disease". Frontiers in Neurology. 9 (144): 144. doi:10.3389/fneur.2018.00144. PMC 5859063. PMID 29593642.
- Daroff RB,Jankovic J,Mazziotta JC,Pomeroy SL (2016). Bradley's neurology in clinical practice (Seventh). Two. Philadelphia: Elsevier. p. 1439. ISBN 978-0-323-28783-8.CS1 maint: multiple names: authors list (link)
- Online Mendelian Inheritance in Man (OMIM): 601104
- Josephs, K. A.; Ishizawa, T.; Tsuboi, Y.; Cookson, N.; Dickson, D. W. (2002). "A clinicopathological study of vascular progressive supranuclear palsy: A multi-infarct disorder presenting as progressive supranuclear palsy". Archives of Neurology. 59 (10): 1597–601. doi:10.1001/archneur.59.10.1597. PMID 12374498.
- Caparros-Lefebvre D, Sergeant N, Lees A, Camuzat A, Daniel S, Lannuzel A, et al. (April 2002). "Guadeloupean parkinsonism: a cluster of progressive supranuclear palsy-like tauopathy". Brain. 125 (Pt 4): 801–11. doi:10.1093/brain/awf086. PMID 11912113.
- Amano N, Iwabuchi K, Yokoi S, Yagishita S, Itoh Y, Saitoh A, et al. (January 1989). "[The reappraisal study of the ultrastructure of Alzheimer's neurofibrillary tangles in three cases of progressive supranuclear palsy]". No to Shinkei = Brain and Nerve (in Japanese). 41 (1): 35–44. PMID 2655673.
- Buée L, Delacourte A (October 1999). "Comparative biochemistry of tau in progressive supranuclear palsy, corticobasal degeneration, FTDP-17 and Pick's disease". Brain Pathology. 9 (4): 681–93. doi:10.1111/j.1750-3639.1999.tb00550.x. PMID 10517507. S2CID 10711305.
- Feany MB, Mattiace LA, Dickson DW (January 1996). "Neuropathologic overlap of progressive supranuclear palsy, Pick's disease and corticobasal degeneration". Journal of Neuropathology and Experimental Neurology. 55 (1): 53–67. doi:10.1097/00005072-199601000-00006. PMID 8558172.
- Uchikado H, DelleDonne A, Ahmed Z, Dickson DW (April 2006). "Lewy bodies in progressive supranuclear palsy represent an independent disease process". Journal of Neuropathology and Experimental Neurology. 65 (4): 387–95. doi:10.1097/01.jnen.0000218449.17073.43. PMID 16691119.
- Keith-Rokosh J, Ang LC (November 2008). "Progressive supranuclear palsy: a review of co-existing neurodegeneration". The Canadian Journal of Neurological Sciences. 35 (5): 602–8. doi:10.1017/S0317167100009392. PMID 19235444.
- Rigby HB, Dugger BN, Hentz JG, Adler CH, Beach TG, Shill HA, et al. (March 2015). "Clinical Features of Patients with Concomitant Parkinson's Disease and Progressive Supranuclear Palsy Pathology". Movement Disorders Clinical Practice. 2 (1): 33–38. doi:10.1002/mdc3.12104. PMC 6183005. PMID 30363831.
- Gearing M, Olson DA, Watts RL, Mirra SS (June 1994). "Progressive supranuclear palsy: neuropathologic and clinical heterogeneity". Neurology. 44 (6): 1015–24. doi:10.1212/wnl.44.6.1015. PMID 8208392. S2CID 20622672.
- Dugger BN, Adler CH, Shill HA, Caviness J, Jacobson S, Driver-Dunckley E, Beach TG, et al. (Arizona Parkinson's Disease Consortium) (May 2014). "Concomitant pathologies among a spectrum of parkinsonian disorders". Parkinsonism & Related Disorders. 20 (5): 525–9. doi:10.1016/j.parkreldis.2014.02.012. PMC 4028418. PMID 24637124.
- Kertesz A, Munoz D (2004). "Relationship between frontotemporal dementia and corticobasal degeneration/progressive supranuclear palsy". Dementia and Geriatric Cognitive Disorders. 17 (4): 282–6. doi:10.1159/000077155. PMID 15178937. S2CID 21017979.
- Katsuse O, Iseki E, Arai T, Akiyama H, Togo T, Uchikado H, et al. (September 2003). "4-repeat tauopathy sharing pathological and biochemical features of corticobasal degeneration and progressive supranuclear palsy". Acta Neuropathologica. 106 (3): 251–60. doi:10.1007/s00401-003-0728-8. PMID 12802605. S2CID 20275104.
- Hattori M, Hashizume Y, Yoshida M, Iwasaki Y, Hishikawa N, Ueda R, Ojika K (August 2003). "Distribution of astrocytic plaques in the corticobasal degeneration brain and comparison with tuft-shaped astrocytes in the progressive supranuclear palsy brain". Acta Neuropathologica. 106 (2): 143–9. doi:10.1007/s00401-003-0711-4. PMID 12732936. S2CID 25741692.
- Komori T, Arai N, Oda M, Nakayama H, Mori H, Yagishita S, et al. (October 1998). "Astrocytic plaques and tufts of abnormal fibers do not coexist in corticobasal degeneration and progressive supranuclear palsy". Acta Neuropathologica. 96 (4): 401–8. doi:10.1007/s004010050911. PMID 9797005. S2CID 7265831.
- Zhu MW, Wang LN, Li XH, Gui QP (April 2004). "[Glial abnormalities in progressive supranuclear palsy and corticobasal degeneration]" [Glial abnormalities in progressive supranuclear palsy and corticobasal degeneration]. Zhonghua Bing Li Xue Za Zhi = Chinese Journal of Pathology (in Chinese). 33 (2): 125–9. doi:10.3760/j.issn:0529-5807.2004.02.008. PMID 15132848.
- Wang LN, Zhu MW, Feng YQ, Wang JH (June 2006). "Pick's disease with Pick bodies combined with progressive supranuclear palsy without tuft-shaped astrocytes: a clinical, neuroradiologic and pathological study of an autopsied case". Neuropathology. 26 (3): 222–30. doi:10.1111/j.1440-1789.2006.00671.x. PMID 16771179. S2CID 25562683.
- Shukla R, Sinha M, Kumar R, Singh D (April 2009). "'Hummingbird' sign in progressive supranuclear palsy". Annals of Indian Academy of Neurology. 12 (2): 133. doi:10.4103/0972-2327.53087. PMC 2812742. PMID 20142864.
- Sonthalia N, Ray S (September 2012). "The Hummingbird sign: a diagnostic clue for Steele-Richardson-Olszweski syndrome". BMJ Case Reports. 2012: bcr2012006263. doi:10.1136/bcr-2012-006263. PMC 4543120. PMID 22987902.
- Ling H (January 2016). "Clinical Approach to Progressive Supranuclear Palsy". Journal of Movement Disorders. 9 (1): 3–13. doi:10.14802/jmd.15060. PMC 4734991. PMID 26828211.
- https://academic.oup.com/brain/article/125/4/801/260717
- Dickson DW, Ahmed Z, Algom AA, Tsuboi Y, Josephs KA (August 2010). "Neuropathology of variants of progressive supranuclear palsy". Current Opinion in Neurology. 23 (4): 394–400. doi:10.1097/WCO.0b013e32833be924. PMID 20610990.
- Kanazawa M, Tada M, Onodera O, Takahashi H, Nishizawa M, Shimohata T. (2013). "Early clinical features of patients with progressive supranuclear palsy with predominant cerebellar ataxia". Parkinsonism Relat Disord. 19 (12): 1149–1151. doi:10.1016/j.parkreldis.2013.07.019. PMID 23916652.CS1 maint: multiple names: authors list (link)
- "Progressive Supranuclear Palsy Fact Sheet | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. NIH. Retrieved 19 February 2019.
- Litvan I, Campbell G, Mangone CA, Verny M, McKee A, Chaudhuri KR, et al. (January 1997). "Which clinical features differentiate progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome) from related disorders? A clinicopathological study". Brain. 120 ( Pt 1) (Pt 1): 65–74. doi:10.1093/brain/120.1.65. PMID 9055798.
- Moore DP, Puri BK (2012-06-29). Textbook of Clinical Neuropsychiatry and Behavioral Neuroscience. pp. 400–401. ISBN 978-1-4441-6494-7.
- Williams DR, Watt HC, Lees AJ (April 2006). "Predictors of falls and fractures in bradykinetic rigid syndromes: a retrospective study". Journal of Neurology, Neurosurgery, and Psychiatry. 77 (4): 468–73. doi:10.1136/jnnp.2005.074070. PMC 2077491. PMID 16543524.
- Elble, Rodger J. "Progressive Supranuclear Palsy". www.rarediseases.org.
- O'Sullivan SS, Massey LA, Williams DR, Silveira-Moriyama L, Kempster PA, Holton JL, et al. (May 2008). "Clinical outcomes of progressive supranuclear palsy and multiple system atrophy". Brain. 131 (Pt 5): 1362–72. doi:10.1093/brain/awn065. PMID 18385183.
- Williams DR, de Silva R, Paviour DC, Pittman A, Watt HC, Kilford L, et al. (June 2005). "Characteristics of two distinct clinical phenotypes in pathologically proven progressive supranuclear palsy: Richardson's syndrome and PSP-parkinsonism". Brain. 128 (Pt 6): 1247–58. doi:10.1093/brain/awh488. PMID 15788542.
- Brooks DJ (March 2002). "Diagnosis and management of atypical parkinsonian syndromes". Journal of Neurology, Neurosurgery, and Psychiatry. 72 Suppl 1: I10–I16. doi:10.1136/jnnp.72.suppl_1.i10 (inactive 2021-01-19). PMC 1765580. PMID 11870198.CS1 maint: DOI inactive as of January 2021 (link)
- "What is progressive supranuclear palsy?". Movementdisorders.org. Retrieved 2017-01-08.
- "Orphanet: Progressive supranuclear palsy". Orpha.net. Retrieved 2017-01-08.
- "What's New in Progressive Supranuclear Palsy?" (PDF). Acnr.org. Retrieved 2017-01-08.
- "Progressive Supranuclear Palsy – NORD (National Organization for Rare Disorders)". Rarediseases.org. Retrieved 2017-01-08.
- Williams DR, Lees AJ (March 2009). "Progressive supranuclear palsy: clinicopathological concepts and diagnostic challenges". The Lancet. Neurology. 8 (3): 270–9. doi:10.1016/S1474-4422(09)70042-0. PMID 19233037. S2CID 1417930.
- Barsottini OG, Felício AC, Aquino CC, Pedroso JL (December 2010). "Progressive supranuclear palsy: new concepts". Arquivos de Neuro-Psiquiatria. 68 (6): 938–46. doi:10.1590/s0004-282x2010000600020. PMID 21243256.
- Nijboer H, Dautzenberg PL (June 2009). "[Progressive supranucleair palsy: acetylcholineeserase-inhibitor a possible therapy?]". Tijdschrift voor Gerontologie en Geriatrie. 40 (3): 133–7. doi:10.1007/BF03079574. PMID 19731749. S2CID 140525754.
- Liepelt I, Gaenslen A, Godau J, Di Santo A, Schweitzer KJ, Gasser T, Berg D (January 2010). "Rivastigmine for the treatment of dementia in patients with progressive supranuclear palsy: Clinical observations as a basis for power calculations and safety analysis". Alzheimer's & Dementia. 6 (1): 70–4. doi:10.1016/j.jalz.2009.04.1231. PMID 20129321. S2CID 33349776.
- Abe K (January 2008). "Zolpidem therapy for movement disorders". Recent Patents on CNS Drug Discovery. 3 (1): 55–60. doi:10.2174/157488908783421519. PMID 18221242.
- Barsottini OG, Felício AC, Aquino CC, Pedroso JL (December 2010). "Progressive supranuclear palsy: new concepts". Arquivos de Neuro-Psiquiatria. 68 (6): 938–46. doi:10.1590/S0004-282X2010000600020. PMID 21243256.
- Zampieri C, Di Fabio RP (June 2006). "Progressive supranuclear palsy: disease profile and rehabilitation strategies". Physical Therapy. 86 (6): 870–80. doi:10.1093/ptj/86.6.870. PMID 16737412.
- van Balken I, Litvan I (May 2006). "Current and future treatments in progressive supranuclear palsy". Current Treatment Options in Neurology. 8 (3): 211–23. doi:10.1007/s11940-006-0012-z. PMID 16569380. S2CID 30537997.
- Golbe LI (November 2001). "Progressive Supranuclear Palsy". Current Treatment Options in Neurology. 3 (6): 473–477. doi:10.1007/s11940-001-0010-0. PMID 11581524. S2CID 36973020.
- Boxer, Adam L.; Lang, Anthony E.; Grossman, Murray; Knopman, David S.; Miller, Bruce L.; Schneider, Lon S.; Doody, Rachelle S.; Lees, Andrew; Golbe, Lawrence I.; Williams, David R.; Corvol, Jean-Cristophe (July 2014). "Davunetide in patients with progressive supranuclear palsy: a randomised, double-blind, placebo-controlled phase 2/3 trial". The Lancet. Neurology. 13 (7): 676–685. doi:10.1016/S1474-4422(14)70088-2. ISSN 1474-4465. PMC 4129545. PMID 24873720.
- DeVos, Sarah L.; Miller, Rebecca L.; Schoch, Kathleen M.; Holmes, Brandon B.; Kebodeaux, Carey S.; Wegener, Amy J.; Chen, Guo; Shen, Tao; Tran, Hien; Nichols, Brandon; Zanardi, Tom A. (2017-01-25). "Tau Reduction Prevents Neuronal Loss and Reverses Pathological Tau Deposition and Seeding in Mice with Tauopathy". Science Translational Medicine. 9 (374): eaag0481. doi:10.1126/scitranslmed.aag0481. ISSN 1946-6234. PMC 5792300. PMID 28123067.
- PhD, Joana Carvalho. "Ionis Licensed IONIS-MAPTRx AntisenseTherapy for Alzheimer's to Biogen". Retrieved 2020-12-09.
- https://www.independent.ie/life/health-wellbeing/health-features/i-dont-want-to-believe-i-have-an-incurable-brain-disease-but-i-know-i-have-former-rte-presenter-kieron-wood-38614857.html
- Tomita S, Oeda T, Umemura A, Kohsaka M, Park K, Yamamoto K, et al. (August 13, 2015). "Impact of Aspiration Pneumonia on the Clinical Course of Progressive Supranuclear Palsy: A Retrospective Cohort Study". PLOS ONE. 10 (8): e0135823. Bibcode:2015PLoSO..1035823T. doi:10.1371/journal.pone.0135823. PMC 4536232. PMID 26270456.
- Richardson JC, Steele J, Olszewski J (1963). "Supranuclear Ophthalmoplegia, Pseudobulbar Palsy, Nuchal Dystonia and Dementia. A Clinical Report on Eight Cases of "heterogenous System Degeneration"". Transactions of the American Neurological Association. 88: 25–9. PMID 14272249.
- Steele JC, Richardson JC, Olszewski J (April 1964). "Progressive Supranuclear Palsy". Archives of Neurology. 10 (4): 333–59. doi:10.1001/archneur.1964.00460160003001. PMID 14107684.
- Hershey L,Farlow MR, Lichter D. "Progressive supranuclear palsy: cognitive and behavioral changes".CS1 maint: multiple names: authors list (link)
- Brusa A, Stoehr R, Pramstaller PP (March 2004). "Progressive supranuclear palsy: new disease or variant of postencephalitic parkinsonism?". Movement Disorders. 19 (3): 247–52. doi:10.1002/mds.10699. PMID 15022178. S2CID 41907329.
- Albert ML, Willis A, Feldman RG (1974). "The "subcortical dementias"of progressive supranuclear palsy". Journal of Neurology, Neurosurgery, and Psychiatry. 37 (2): 121–130. doi:10.1136/jnnp.37.2.121. PMC 494589. PMID 4819905.CS1 maint: multiple names: authors list (link)
- PSP Society of Canada, re-linked 2020-01-20
- PSP France - Notre histoire, re-linked 2020-01-20
- PSPA, re-linked 2020-01-20
- CurePSP, re-linked 2020-01-20
- Bentley, Jean (May 3, 2020). "'Zoey's Extraordinary Playlist' Boss on That Devastating Finale and Season 2 Plans". The Hollywood Reporter. Retrieved 2020-05-04.
- Schulman, Michael (September 1, 2019). "Linda Ronstadt Has Found Another Voice". The New Yorker.
| Classification | |
|---|---|
| External resources |