Status epilepticus
Status epilepticus (SE) is a single seizure lasting more than five minutes or two or more seizures within a five-minute period without the person returning to normal between them.[1] Previous definitions used a 30-minute time limit.[2] The seizures can be of the tonic–clonic type, with a regular pattern of contraction and extension of the arms and legs, or of types that do not involve contractions, such as absence seizures or complex partial seizures.[1] Status epilepticus is a life-threatening medical emergency, particularly if treatment is delayed.[1]
| Status epilepticus | |
|---|---|
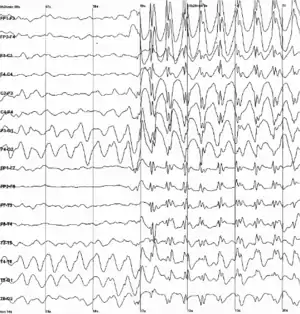 | |
| Generalized 3 Hz spike-and-wave discharges on an electroencephalogram | |
| Specialty | Emergency medicine, neurology |
| Symptoms | Regular pattern of contraction and extension of the arms and legs, movement of one part of the body, unresponsive[1] |
| Duration | > 5 minutes[1] |
| Risk factors | Epilepsy, underlying problem with the brain[2] |
| Diagnostic method | Blood sugar, imaging of the head, blood tests, electroencephalogram[1] |
| Differential diagnosis | Psychogenic nonepileptic seizures, movement disorders, meningitis, delirium[1] |
| Treatment | Benzodiazepines, phenytoin[1] |
| Prognosis | ~20% thirty day risk of death[1] |
| Frequency | 40 per 100,000 people per year[2] |
Status epilepticus may occur in those with a history of epilepsy as well as those with an underlying problem of the brain.[2] These underlying brain problems may include trauma, infections, or strokes among others.[2] Diagnosis often involves checking the blood sugar, imaging of the head, a number of blood tests, and an electroencephalogram.[1] Psychogenic nonepileptic seizures may present similarly.[1] Other conditions that may also appear to be SE include low blood sugar, movement disorders, meningitis, and delirium among others.[1] It can also appear when tuberculosis meningitis becomes very severe.
Benzodiazepines are the preferred initial treatment after which typically phenytoin is given.[1] Possible benzodiazepines include intravenous lorazepam as well as intramuscular injections of midazolam.[3] A number of other medications may be used if these are not effective such as valproic acid, phenobarbital, propofol, or ketamine.[1] Intubation may be required to help maintain the person's airway.[1] Between 10 and 30% of people who have status epilepticus die within 30 days.[1] The underlying cause, the person's age, and the length of the seizure are important factors in the outcome.[2] Status epilepticus occurs in up to 40 per 100,000 people per year.[2] It makes up about 1% of people who visit the emergency department.[1]
Signs and symptoms
Status epilepticus can be divided into two categories: convulsive and nonconvulsive (NCSE).[1]
Convulsive
Convulsive status epilepticus presents with a regular pattern of contraction and extension of the arms and legs.[1]
Epilepsia partialis continua is a variant involving hour-, day-, or even week-long jerking. It is a consequence of vascular disease, tumors, or encephalitis, and is drug-resistant.
Generalized myoclonus is commonly seen in comatose people following CPR and is seen by some as an indication of catastrophic damage to the neocortex.[4]
Refractory status epilepticus is defined as status epilepticus that continues despite treatment with benzodiazepines and one antiepileptic drug.[5]
Super-refractory status epilepticus is defined as status epilepticus that continues or recurs 24 hours or more after the onset of anaesthetic therapy, including those cases where status epilepticus recurs on the reduction or withdrawal of anesthesia.[6]
Nonconvulsive
Nonconvulsive status epilepticus is a relatively long duration change in a person's level of consciousness without large scale bending and extension of the limbs due to seizure activity.[7] It is of two main types with either prolonged complex partial seizures or absence seizures.[7] Up to a quarter of cases of SE are nonconvulsive.[7]
In the case of complex partial status epilepticus, the seizure is confined to a small area of the brain, normally the temporal lobe. Absence status epilepticus is marked by a generalized seizure affecting the whole brain. An EEG is needed to differentiate between the two conditions. This results in episodes characterized by a long-lasting stupor, staring, and unresponsiveness.
Causes
Only 25% of people who experience seizures or status epilepticus have epilepsy.[8] The following is a list of possible causes:
- Stroke[8]
- Hemorrhage[8]
- Intoxicants[8] or adverse reactions to drugs
- Insufficient dosage or sudden withdrawal of a medication (especially anticonvulsants)
- Consumption of alcoholic beverages while on an anticonvulsant, or alcohol withdrawal
- Dieting or fasting while on an anticonvulsant
- Starting on a new medication that reduces the effectiveness of the anticonvulsant or changes drug metabolism, decreasing its half-life, leading to decreased blood concentrations
- Developing a resistance to an anticonvulsant already being used
- Gastroenteritis while on an anticonvulsant, where lower levels of anticonvulsant may exist in the bloodstream due to vomiting of gastric contents or reduced absorption due to mucosal edema
- Developing a new, unrelated condition in which seizures are coincidentally also a symptom, but are not controlled by an anticonvulsant already used
- Metabolic disturbances—such as affected kidney and liver[8]
- Sleep deprivation of more than a short duration is often the cause of a (usually, but not always, temporary) loss of seizure control.
Diagnosis
Diagnosis vary, but currently it is defined as one continuous, unremitting seizure lasting longer than five minutes,[9] or recurrent seizures without regaining consciousness between seizures for greater than five minutes.[1] Previous definitions used a 30-minute time limit.[2]
Nonconvulsive status epilepticus is believed to be under-diagnosed.[10]
Treatments

Benzodiazepines are the preferred initial treatment after which typically phenytoin or fosphenytoin is given.[1] First aid guidelines for seizures state that, as a rule, an ambulance should be called for seizures lasting longer than five minutes (or sooner if this is the person's first seizure episode and no precipitating factors are known, or if SE happens to a person with epilepsy whose seizures were previously absent or well controlled for a considerable time period).
Benzodiazepines
When given intravenously, lorazepam appears to be superior to diazepam for stopping seizure activity.[3][11] Intramuscular midazolam appears to be a reasonable option especially in those who are not in hospital.[3]
The benzodiazepine of choice in North America for initial treatment is lorazepam, due to its relatively long duration of action (2–8 hours) when injected, and rapid onset of action, which is thought to be due to its high affinity for GABA receptors and low lipid solubility, which causes it to remain in the vascular compartment. If lorazepam is not available, or intravenous access is not possible, then diazepam should be given.[12]
In several countries outside North America, intravenous clonazepam is regarded as the drug of first choice. For instance, a guideline from the Netherlands recommends clonazepam.[13] Cited advantages of clonazepam include a longer duration of action than diazepam, and a lower propensity for the development of acute tolerance than lorazepam.[14] The use of clonazepam for this indication has not caught on in North America, as it is not available as an intravenous formulation there.[14]
Particularly in children, another popular treatment choice is midazolam, given into the side of the mouth or the nose.[15] Sometimes, the failure of lorazepam alone is considered to be enough to classify a case of SE as resistant to treatment.
Phenytoin and fosphenytoin
Phenytoin was once another first-line therapy,[16] although the prodrug fosphenytoin can be administered three times as fast and with far fewer injection site reactions. If these or any other hydantoin derivatives are used, then cardiac monitoring is necessary if they are administered intravenously. Because the hydantoins take 15–30 minutes to work, a benzodiazepine or barbiturate is often coadministered. Because of diazepam's short duration of action, they were often administered together anyway.
Barbiturates
Before the benzodiazepines were invented, there were the barbiturates, which are still used today if benzodiazepines or the hydantoins are not an option. These are used to induce a barbituric coma. The barbiturate most commonly used for this is phenobarbital. Thiopental or pentobarbital may also be used for that purpose if the seizures have to be stopped immediately or if the person has already been compromised by the underlying illness or toxic/metabolic-induced seizures; however, in those situations, thiopental is the agent of choice.
Carbamazepine and valproate
Valproate is available to be given intravenously, and may be used for status epilepticus. Carbamazepine is not available in an intravenous formulation, and does not play a role in status epilepticus.[16]
Others
If this proves ineffective or if barbiturates cannot be used for some reason, then a general anesthetic such as propofol[17] may be tried; sometimes it is used second after the failure of lorazepam.[18] This would entail putting the person on artificial ventilation. Propofol has been shown to be effective in suppressing the jerks seen in myoclonus status epilepticus.[19]
Ketamine, an NMDA antagonist drug, can be used as a last resort for drug-resistant status epilepticus.[20]
Lidocaine has been used in cases that do not improve with other more typical medications.[21] One concern is that seizures often begin again 30 minutes after it is stopped.[21] Additionally, it is not recommended in those with heart or liver problems.[21]
Prognosis
Between 10 and 30% of people who have status epilepticus die within 30 days.[1] The great majority of these people have an underlying brain condition causing their status seizure such as brain tumor, brain infection, brain trauma, or stroke. However, people with diagnosed epilepsy who have a status seizure also have an increased risk of death if their condition is not stabilized quickly, their medication and sleep regimen adapted and adhered to, and stress and other stimulant (seizure trigger) levels controlled. However, with optimal neurological care, adherence to the medication regimen, and a good prognosis (no other underlying uncontrolled brain or other organic disease), the person—even people who have been diagnosed with epilepsy—in otherwise good health can survive with minimal or no brain damage, and can decrease risk of death and even avoid future seizures.[8]
Epidemiology
In the United States, about 40 cases of SE occur annually per 100,000 people.[2] This includes about 10–20% of all first seizures.
Research
Allopregnanolone is being studied in a clinical trial by the Mayo Clinic to treat super-resistant status epilepticus.[22]
See also
References
- Al-Mufti, F; Claassen, J (Oct 2014). "Neurocritical Care: Status Epilepticus Review". Critical Care Clinics. 30 (4): 751–764. doi:10.1016/j.ccc.2014.06.006. PMID 25257739.
- Trinka, E; Höfler, J; Zerbs, A (September 2012). "Causes of status epilepticus". Epilepsia. 53 Suppl 4: 127–38. doi:10.1111/j.1528-1167.2012.03622.x. PMID 22946730. S2CID 5294771.
- Prasad, M; Krishnan, PR; Sequeira, R; Al-Roomi, K (Sep 10, 2014). "Anticonvulsant therapy for status epilepticus". The Cochrane Database of Systematic Reviews. 9 (9): CD003723. doi:10.1002/14651858.CD003723.pub3. PMC 7154380. PMID 25207925.
- Wijdicks, Eelco F. M.; Parisi, J. E.; Sharbrough, F. W. (February 1994). "Prognostic value of myoclonus status in comatose survivors of cardiac arrest". Annals of Neurology. 35 (2): 239–43. doi:10.1002/ana.410350219. PMID 8109907. S2CID 42680232.
- Rossetti, AO; Lowenstein, DH (October 2011). "Management of refractory status epilepticus in adults: still more questions than answers". The Lancet. Neurology. 10 (10): 922–30. doi:10.1016/s1474-4422(11)70187-9. PMC 3202016. PMID 21939901.
- Shorvon Simon, Ferlisi Monica (2011). "A Critical Review of Available Therapies and a Clinical Treatment Protocol". Brain. 134 (10): 2802–2818. doi:10.1093/brain/awr215. PMID 21914716.
- Chang, AK; Shinnar, S (Feb 2011). "Nonconvulsive status epilepticus". Emergency Medicine Clinics of North America. 29 (1): 65–72. doi:10.1016/j.emc.2010.08.006. PMID 21109103.
- Stasiukyniene, V.; Pilvinis, V.; Reingardiene, D.; Janauskaite, L. (2009). "[Epileptic seizures in critically ill patients]". Medicina. 45 (6): 501–7. doi:10.3390/medicina45060066. PMID 19605972.
- Nair, PP; Kalita, J.; Misra, U. K. (Jul–Sep 2011). "Status epilepticus: why, what, and how". Journal of Postgraduate Medicine. 57 (3): 242–52. doi:10.4103/0022-3859.81807. PMID 21941070.
- Rubin, Diana; Stephan, Ruegg; Stephan, Marsch; Christian, Schindler; Leticia, Grize; Raoul, Sutter (August 24, 2011). "High prevalence of nonconvulsive and subtle status epilepticus in an ICU of a tertiary care center: A three-year observational cohort study". Epilepsy Research. 96 (1): 140–150. doi:10.1016/j.eplepsyres.2011.05.018. PMID 21676592. S2CID 25684463.
- Zhao, ZY; Wang, HY; Wen, B; Yang, ZB; Feng, K; Fan, JC (28 March 2016). "A Comparison of Midazolam, Lorazepam, and Diazepam for the Treatment of Status Epilepticus in Children: A Network Meta-analysis". Journal of Child Neurology. 31 (9): 1093–107. doi:10.1177/0883073816638757. PMID 27021145. S2CID 7677504.
- Pang, Trudy; Lawrence J. Hirsch (July 2005). "Treatment of Convulsive and Nonconvulsive Status Epilepticus". Current Treatment Options in Neurology. 7 (4): 247–259. doi:10.1007/s11940-005-0035-x. PMID 15967088. S2CID 31286223.
- "22.8 Convulsive status epilepticus" (PDF). Acute Boekje (in Dutch) (4th ed.). Van Zuiden Communications B.V. 2009. p. 276. ISBN 978-90-8523-197-4.
- Lawn, Nicholas D; Wijdicks, Eelco FM (2002). "Status epilepticus: A critical review of management options". Neurol J Southeast Asia. 7: 47–59.
- Walker, D. M.; Teach, S. J. (June 2006). "Update on the acute management of status epilepticus in children". Curr Opin Pediatr. 18 (3): 239–44. doi:10.1097/01.mop.0000193306.55635.24. PMID 16721142. S2CID 42391321.
- Beran, RG. (April 2008). "An alternative perspective on the management of status epilepticus". Epilepsy Behav. 12 (3): 349–53. doi:10.1016/j.yebeh.2007.12.013. hdl:10072/22410. PMID 18262847. S2CID 42219786.
- Pourrat, X; J .M. Serekian, D. Antier, J. Grassin (June 9, 2001). "Generalized tonic-clonic status epilepticus: therapeutic strategy". Presse Médicale. 30 (20): 1031–6. PMID 11433696.CS1 maint: multiple names: authors list (link) (French).
- Marik, Paul E.; Joseph Varon (2004). "The management of status epilepticus". Chest. 126 (2): 582–91. doi:10.1378/chest.126.2.582. PMID 15302747. S2CID 29378123.
- Wijdicks, Eelco F. M. (July 2002). "Propofol in myoclonus status epilepticus in comatose patients following cardiac resuscitation". Journal of Neurology, Neurosurgery, and Psychiatry. 73 (1): 94–5. doi:10.1136/jnnp.73.1.94. PMC 1757284. PMID 12082068.
- Gomes, D; Pimentel, J; Bentes, C; Aguiar de Sousa, D; Antunes, AP; Alvarez, A; Silva, ZC (31 October 2018). "Consensus Protocol for the Treatment of Super-Refractory Status Epilepticus". Acta Medica Portuguesa. 31 (10): 598–605. doi:10.20344/amp.9679. PMID 30387431.
- Schmutzhard, E; Pfausler, B (Oct 2011). "Complications of the management of status epilepticus in the intensive care unit". Epilepsia. 52 Suppl 8: 39–41. doi:10.1111/j.1528-1167.2011.03233.x. PMID 21967359. S2CID 205692349.
- "A Study Using SAGE-547 for Super Resistant Status Epilepticus". Archived from the original on 2017-03-08. Retrieved 2017-03-07.
External links
| Classification | |
|---|---|
| External resources |
- Evidence-Based Guideline: Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society
- Thomas, SanjeevV; Cherian, Ajith (2009). "Status epilepticus". Annals of Indian Academy of Neurology. 12 (3): 140–53. doi:10.4103/0972-2327.56312. PMC 2824929. PMID 20174493.