Pre-eclampsia
Pre-eclampsia is a disorder of pregnancy characterized by the onset of high blood pressure and often a significant amount of protein in the urine.[1][8] When it arises, the condition begins after 20 weeks of pregnancy.[2][3] In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances.[2][3] Pre-eclampsia increases the risk of poor outcomes for both the mother and the baby.[3] If left untreated, it may result in seizures at which point it is known as eclampsia.[2]
| Pre-eclampsia | |
|---|---|
| Other names | Preeclampsia toxaemia (PET) |
 | |
| A micrograph showing hypertrophic decidual vasculopathy, a finding seen in gestational hypertension and pre-eclampsia. H&E stain. | |
| Specialty | Obstetrics |
| Symptoms | High blood pressure, protein in the urine[1] |
| Complications | Red blood cell breakdown, low blood platelet count, impaired liver function, kidney problems, swelling, shortness of breath due to fluid in the lungs, eclampsia[2][3] |
| Usual onset | After 20 weeks of pregnancy[2] |
| Risk factors | Obesity, prior hypertension, older age, diabetes mellitus[2][4] |
| Diagnostic method | BP > 140 mmHg systolic or 90 mmHg diastolic at two separate times[3] |
| Prevention | Aspirin, calcium supplementation, treatment of prior hypertension[4][5] |
| Treatment | Delivery, medications[4] |
| Medication | Labetalol, methyldopa, magnesium sulfate[4][6] |
| Frequency | 2–8% of pregnancies[4] |
| Deaths | 46,900 hypertensive disorders in pregnancy (2015)[7] |
Risk factors for pre-eclampsia include obesity, prior hypertension, older age, and diabetes mellitus.[2][4] It is also more frequent in a woman's first pregnancy and if she is carrying twins.[2] The underlying mechanism involves abnormal formation of blood vessels in the placenta amongst other factors.[2] Most cases are diagnosed before delivery. Rarely, pre-eclampsia may begin in the period after delivery.[3] While historically both high blood pressure and protein in the urine were required to make the diagnosis, some definitions also include those with hypertension and any associated organ dysfunction.[3][9] Blood pressure is defined as high when it is greater than 140 mmHg systolic or 90 mmHg diastolic at two separate times, more than four hours apart in a woman after twenty weeks of pregnancy.[3] Pre-eclampsia is routinely screened for during prenatal care.[10][11]
Recommendations for prevention include: aspirin in those at high risk, calcium supplementation in areas with low intake, and treatment of prior hypertension with medications.[4][5] In those with pre-eclampsia delivery of the baby and placenta is an effective treatment.[4] When delivery becomes recommended depends on how severe the pre-eclampsia and how far along in pregnancy a woman is.[4] Blood pressure medication, such as labetalol and methyldopa, may be used to improve the mother's condition before delivery.[6] Magnesium sulfate may be used to prevent eclampsia in those with severe disease.[4] Bedrest and salt intake have not been found to be useful for either treatment or prevention.[3][4]
Pre-eclampsia affects 2–8% of pregnancies worldwide.[4] Hypertensive disorders of pregnancy (which include pre-eclampsia) are one of the most common causes of death due to pregnancy.[6] They resulted in 46,900 deaths in 2015.[7] Pre-eclampsia usually occurs after 32 weeks; however, if it occurs earlier it is associated with worse outcomes.[6] Women who have had pre-eclampsia are at increased risk of heart disease and stroke later in life.[10]
The word "eclampsia" is from the Greek term for lightning.[12] The first known description of the condition was by Hippocrates in the 5th century BC.[12]
Signs and symptoms
Oedema (especially in the hands and face) was originally considered an important sign for a diagnosis of pre-eclampsia. However, because oedema is a common occurrence in pregnancy, its utility as a distinguishing factor in pre-eclampsia is not high. Pitting edema (unusual swelling, particularly of the hands, feet, or face, notable by leaving an indentation when pressed on) can be significant, and should be reported to a health care provider.
In general, none of the signs of pre-eclampsia are specific, and even convulsions in pregnancy are more likely to have causes other than eclampsia in modern practice. Further, a symptom such as epigastric pain may be misinterpreted as heartburn. Common features of pre-eclampsia which are screened for during pre-natal visits include elevated blood pressure and excess protein in the urine.[13] Diagnosis depends on finding a coincidence of several pre-eclamptic features, the final proof being their regression after delivery.
Causes
There is no definitive known cause of pre-eclampsia, though it is likely related to a number of factors. Some of these factors include:[2][10]
- Abnormal placentation (formation and development of the placenta)
- Immunologic factors
- Prior or existing maternal pathology—pre-eclampsia is seen more at a higher incidence in individuals with pre-existing hypertension, obesity, or antiphospholipid antibody syndrome or those with a history of pre-eclampsia
- Dietary factors, e.g. calcium supplementation in areas where dietary calcium intake is low has been shown to reduce the risk of pre-eclampsia[4]
- Environmental factors, e.g. air pollution[14]
Those with long term high blood pressure have a risk 7 to 8 times higher than those without.[15]
Physiologically, research has linked pre-eclampsia to the following physiologic changes: alterations in the interaction between the maternal immune response and the placenta, placental injury, endothelial cell injury, altered vascular reactivity, oxidative stress, imbalance among vasoactive substances, decreased intravascular volume, and disseminated intravascular coagulation.[10][16]
While the exact cause of pre-eclampsia remains unclear, there is strong evidence that a major cause predisposing a susceptible woman to pre-eclampsia is an abnormally implanted placenta.[2][10] This abnormally implanted placenta may result in poor uterine and placental perfusion, yielding a state of hypoxia and increased oxidative stress and the release of anti-angiogenic proteins along with inflammatory mediators into the maternal plasma.[10] A major consequence of this sequence of events is generalized endothelial dysfunction.[1] The abnormal implantation may stem from the maternal immune system's response to the placenta, specifically a lack of established immunological tolerance in pregnancy. Endothelial dysfunction results in hypertension and many of the other symptoms and complications associated with pre-eclampsia.[2] Those with pre-eclampsia may have a lower risk of breast cancer.[17]
Abnormal chromosome 19 microRNA cluster (C19MC) impairs extravillus trophoblast cell invasion to the spiral arteries, causing high resistance, low blood flow, and low nutrient supply to the fetus.[18][19][20]
Risk factors
Known risk factors for pre-eclampsia include:[6][21]
- Having never previously given birth
- Diabetes mellitus[22]
- Kidney disease
- Chronic hypertension[22]
- Prior history of pre-eclampsia[22]
- Family history of pre-eclampsia
- Advanced maternal age (>35 years)
- Obesity[22]
- Antiphospholipid antibody syndrome[22]
- Multiple gestation[22]
- Having donated a kidney[23]
- Having sub-clinical hypothyroidism or thyroid antibodies[24][25]
- Placental abnormalities such as placental ischemia
Pathogenesis
Although much research into mechanism of pre-eclampsia has taken place, its exact pathogenesis remains uncertain. Pre-eclampsia is thought to result from an abnormal placenta, the removal of which ends the disease in most cases.[2] During normal pregnancy, the placenta vascularizes to allow for the exchange of water, gases, and solutes, including nutrients and wastes, between maternal and fetal circulations.[16] Abnormal development of the placenta leads to poor placental perfusion. The placenta of women with pre-eclampsia is abnormal and characterized by poor trophoblastic invasion.[16] It is thought that this results in oxidative stress, hypoxia, and the release of factors that promote endothelial dysfunction, inflammation, and other possible reactions.[1][16][26]
The clinical manifestations of pre-eclampsia are associated with general endothelial dysfunction, including vasoconstriction and end-organ ischemia.[16] Implicit in this generalized endothelial dysfunction may be an imbalance of angiogenic and anti-angiogenic factors.[2] Both circulating and placental levels of soluble fms-like tyrosine kinase-1 (sFlt-1) are higher in women with pre-eclampsia than in women with normal pregnancy.[16] sFlt-1 is an anti-angiogenic protein that antagonizes vascular endothelial growth factor (VEGF) and placental growth factor (PIGF), both of which are proangiogenic factors.[10] Soluble endoglin (sEng) has also been shown to be elevated in women with pre-eclampsia and has anti-angiogenic properties, much like sFlt-1 does.[16]
Both sFlt-1 and sEng are upregulated in all pregnant women to some extent, supporting the idea that hypertensive disease in pregnancy is a normal pregnancy adaptation gone awry. As natural killer cells are intimately involved in placentation and placentation involves a degree of maternal immune tolerance for a foreign placenta, it is not surprising that the maternal immune system might respond more negatively to the arrival of some placentae under certain circumstances, such as a placenta which is more invasive than normal. Initial maternal rejection of the placental cytotrophoblasts may be the cause of the inadequately remodeled spiral arteries in those cases of pre-eclampsia associated with shallow implantation, leading to downstream hypoxia and the appearance of maternal symptoms in response to upregulated sFlt-1 and sEng.
Oxidative stress may also play an important part in the pathogenesis of pre-eclampsia. The main source of reactive oxygen species (ROS) is the enzyme xanthine oxidase (XO) and this enzyme mainly occurs in the liver. One hypothesis is that the increased purine catabolism from placental hypoxia results in increased ROS production in the maternal liver and release into the maternal circulation that causes endothelial cell damage.[27]
Abnormalities in the maternal immune system and insufficiency of gestational immune tolerance seem to play major roles in pre-eclampsia. One of the main differences found in pre-eclampsia is a shift toward Th1 responses and the production of IFN-γ. The origin of IFN-γ is not clearly identified and could be the natural killer cells of the uterus, the placental dendritic cells modulating responses of T helper cells, alterations in synthesis of or response to regulatory molecules, or changes in the function of regulatory T cells in pregnancy.[28] Aberrant immune responses promoting pre-eclampsia may also be due to an altered fetal allorecognition or to inflammatory triggers.[28] It has been documented that fetal cells such as fetal erythroblasts as well as cell-free fetal DNA are increased in the maternal circulation in women who develop pre-eclampsia. These findings have given rise to the hypothesis that pre-eclampsia is a disease process by which a placental lesion such as hypoxia allows increased fetal material into the maternal circulation, that in turn leads to an immune response and endothelial damage, and that ultimately results in pre-eclampsia and eclampsia.
One hypothesis for vulnerability to pre-eclampsia is the maternal-fetal conflict between the maternal organism and fetus.[29] After the first trimester trophoblasts enter the spiral arteries of the mother to alter the spiral arteries and thereby gain more access to maternal nutrients.[29] Occasionally there is impaired trophoblast invasion that results in inadequate alterations to the uterine spiral arteries.[29] It is hypothesized that the developing embryo releases biochemical signals that result in the woman developing hypertension and pre-eclampsia so that the fetus can benefit from a greater amount of maternal circulation of nutrients due to increased blood flow to the impaired placenta.[29] This results in a conflict between maternal and fetal fitness and survival because the fetus is invested in only its survival and fitness while the mother is invested in this and subsequent pregnancies.[29]
Another evolutionary hypothesis for vulnerability to pre-eclampsia is the idea of ensuring pair-bonding between the mother and father and paternal investment in the fetus.[30] Researchers posit that pre-eclampsia is an adaptation for the mother to terminate investment in a fetus that might have an unavailable father, as determined by repeated semen exposure of the father to the mother.[30] Various studies have shown that women who frequently had exposure to partners' semen before conception had a reduced risk of pre-eclampsia.[30] Also, subsequent pregnancies by the same father had a reduced risk of pre-eclampsia while subsequent pregnancies by a different father had a higher risk of developing pre-eclampsia.[30]
In normal early embryonic development, the outer epithelial layer contains cytotrophoblast cells, a stem cell type found in the trophoblast that later differentiates into the fetal placenta. These cells differentiate into many placental cells types, including extravillous trophoblast cells. Extravillous trophoblast cells are an invasive cell type which remodel the maternal spiral arteries by replacing the maternal epithelium and smooth muscle lining the spiral arteries causing artery dilation. This prevents maternal vasoconstriction in the spiral arteries and allows for continued blood and nutrient supply to the growing fetus with low resistance and high blood flow.[18]
In pre-eclampsia, abnormal expression of chromosome 19 microRNA cluster (C19MC) in placental cell lines reduces extravillus trophoblast migration.[19][20] Specific microRNAs in this cluster which might cause abnormal spiral artery invasion include miR-520h, miR-520b, and 520c-3p. This impairs extravillus trophoblast cells invasion to the maternal spiral arteries, causing high resistance and low blood flow and low nutrient supply to the fetus.[18] There is tentative evidence that vitamin supplementation can decrease the risk.[31]
Diagnosis
| Pre-eclampsia laboratory values | |
|---|---|
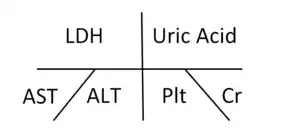 Shorthand for laboratory values commonly used in pre-eclampsia. LDH=Lactate dehydrogenase, Uric acid=Uric acid, AST=Aspartate aminotransferase, ALT=Alanine aminotransferase, Plt=Platelets, Cr=Creatinine. | |
| Reference range | LDH: 105–333 IU/L Uric Acid: 2.4–6.0 mg/dL AST: 5–40 U/L ALT: 7–56 U/L Plt: 140–450 x 109/L Cr: 0.6–1.2 mg/dL |
| MeSH | D007770 |
| LOINC | Codes for pre-eclampsia |
Testing for pre-eclampsia is recommended throughout pregnancy via measuring a woman's blood pressure.[11]
Diagnostic criteria
Pre-eclampsia is diagnosed when a pregnant woman develops:[33]
- Blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic on two separate readings taken at least four to six hours apart after 20 weeks' gestation in an individual with previously normal blood pressure.
- In a woman with essential hypertension beginning before 20 weeks' gestational age, the diagnostic criteria are an increase in systolic blood pressure (SBP) of ≥30 mmHg or an increase in diastolic blood pressure (DBP) of ≥15 mmHg.
- Proteinuria ≥ 0.3 grams (300 mg) or more of protein in a 24-hour urine sample or a SPOT urinary protein to creatinine ratio ≥0.3 or a urine dipstick reading of 1+ or greater (dipstick reading should only be used if other quantitative methods are not available).[3]
Suspicion for pre-eclampsia should be maintained in any pregnancy complicated by elevated blood pressure, even in the absence of proteinuria. Ten percent of individuals with other signs and symptoms of pre-eclampsia and 20% of individuals diagnosed with eclampsia show no evidence of proteinuria.[16] In the absence of proteinuria, the presence of new-onset hypertension (elevated blood pressure) and the new onset of one or more of the following is suggestive of the diagnosis of pre-eclampsia:[3][6]
- Evidence of kidney dysfunction (oliguria, elevated creatinine levels)
- Impaired liver function (noted by liver function tests)
- Thrombocytopenia (platelet count <100,000/microliter)
- Pulmonary edema
- Ankle edema (pitting type)
- Cerebral or visual disturbances
Pre-eclampsia is a progressive disorder and these signs of organ dysfunction are indicative of severe pre-eclampsia. A systolic blood pressure ≥160 or diastolic blood pressure ≥110 and/or proteinuria >5g in a 24-hour period is also indicative of severe pre-eclampsia.[6] Clinically, individuals with severe pre-eclampsia may also present epigastric/right upper quadrant abdominal pain, headaches, and vomiting.[6] Severe pre-eclampsia is a significant risk factor for intrauterine fetal death.
A rise in baseline blood pressure (BP) of 30 mmHg systolic or 15 mmHg diastolic, while not meeting the absolute criteria of 140/90, is important to note but is not considered diagnostic.
Predictive tests
There have been many assessments of tests aimed at predicting pre-eclampsia, though no single biomarker is likely to be sufficiently predictive of the disorder.[10] Predictive tests that have been assessed include those related to placental perfusion, vascular resistance, kidney dysfunction, endothelial dysfunction, and oxidative stress. Examples of notable tests include:
- Doppler ultrasonography of the uterine arteries to investigate for signs of inadequate placental perfusion. This test has a high negative predictive value among those individuals with a history of prior pre-eclampsia.[16]
- Elevations in serum uric acid (hyperuricemia) is used by some to "define" pre-eclampsia,[21] though it has been found to be a poor predictor of the disorder.[16] Elevated levels in the blood (hyperuricemia) are likely due to reduced uric acid clearance secondary to impaired kidney function.
- Angiogenic proteins such as vascular endothelial growth factor (VEGF) and placental growth factor (PIGF) and anti-angiogenic proteins such as soluble fms-like tyrosine kinase-1 (sFlt-1) have shown promise for potential clinical use in diagnosing pre-eclampsia, though evidence is sufficient to recommend a clinical use for these markers.[21]
A recent study, ASPRE, known to be the largest multi-country prospective trial, has reported a significant performance in identifying pregnant women at high risk of pre-eclampsia yet during the first trimester of pregnancy. Utilizing a combination of maternal history, mean arterial blood pressure, intra-uterine Doppler and PlGF measurement, the study has shown a capacity to identify more than 75% of the women that will develop pre-eclampsia, allowing early intervention to prevent development of later symptoms.[34] This approach is now officially recommended by the International Federation of Gynecologists & Obstetricians (FIGO) [35]
- Recent studies have shown that looking for podocytes (specialized cells of the kidney) in the urine has the potential to aid in the prediction of pre-eclampsia. Studies have demonstrated that finding podocytes in the urine may serve as an early marker of and diagnostic test for pre-eclampsia.[36][37][38]
Differential diagnosis
Pre-eclampsia can mimic and be confused with many other diseases, including chronic hypertension, chronic renal disease, primary seizure disorders, gallbladder and pancreatic disease, immune or thrombotic thrombocytopenic purpura, antiphospholipid syndrome and hemolytic-uremic syndrome. It must be considered a possibility in any pregnant woman beyond 20 weeks of gestation. It is particularly difficult to diagnose when pre-existing conditions such as hypertension are present.[39] Women with acute fatty liver of pregnancy may also present with elevated blood pressure and protein in the urine, but differ by the extent of liver damage. Other disorders that can cause high blood pressure include thyrotoxicosis, pheochromocytoma, and drug misuse.[6]
Prevention
Preventive measures against pre-eclampsia have been heavily studied. Because the pathogenesis of pre-eclampsia is not completely understood, prevention remains a complex issue. Below are some of the currently accepted recommendations.
Diet
Supplementation with a balanced protein and energy diet does not appear to reduce the risk of pre-eclampsia.[40] Further, there is no evidence that changing salt intake has an effect.[41]
Supplementation with antioxidants such as vitamin C, D and E has no effect on pre-eclampsia incidence;[42][43] therefore, supplementation with vitamins C, E, and D is not recommended for reducing the risk of pre-eclampsia.[43]
Calcium supplementation of at least 1 gram per day is recommended during pregnancy as it prevents pre-eclampsia where dietary calcium intake is low, especially for those at high risk.[43][44] Higher selenium level is associated with lower incidence of pre-eclampsia.[45][46] Higher cadmium level is associated with higher incidence of pre-eclampsia.[46]
Aspirin
Taking aspirin is associated with a 1 to 5% reduction in pre-eclampsia and a 1 to 5% reduction in premature births in women at high risk.[47] The World Health Organization recommends low-dose aspirin for the prevention of pre-eclampsia in women at high risk and recommends it be started before 20 weeks of pregnancy.[43] The United States Preventive Services Task Force recommends a low-dose regimen for women at high risk beginning in the 12th week.[48] Benefits are less if started after 16 weeks.[49]
The more recent study ASPRE, beside its performance in identifying suspected women to develop pre-eclampsia, has also been able to demonstrate a strong drop in the rate of early pre-eclampsia (-82%) and preterm pre-eclampsia (-62%). Such efficacy of aspirin has been reached due to high performing screening to identify at high risk women, adjusted prophylaxis dosage (150mg/day), timing of the intake (bedtime) and must start before week 16 of pregnancy.[50]
Physical activity
There is insufficient evidence to recommend either exercise[51] or strict bedrest[52] as preventive measures of pre-eclampsia.
Smoking cessation
In low-risk pregnancies, the association between cigarette smoking and a reduced risk of pre-eclampsia has been consistent and reproducible across epidemiologic studies. High-risk pregnancies (those with pregestational diabetes, chronic hypertension, history of pre-eclampsia in a previous pregnancy, or multifetal gestation) showed no significant protective effect. The reason for this discrepancy is not definitively known; research supports speculation that the underlying pathology increases the risk of pre-eclampsia to such a degree that any measurable reduction of risk due to smoking is masked.[53] However, the damaging effects of smoking on overall health and pregnancy outcomes outweighs the benefits in decreasing the incidence of pre-eclampsia.[10] It is recommended that smoking be stopped prior to, during and after pregnancy.[54]
Immune modulation
Some studies have suggested the importance of a woman's gestational immunological tolerance to her baby's father, as the baby and father share genetics. There is tentative evidence that ongoing exposure either by vaginal or oral sex to the same semen that resulted in the pregnancy decreases the risk of pre-eclampsia.[55] As one early study described, "although pre-eclampsia is a disease of first pregnancies, the protective effect of multiparity is lost with change of partner".[56] The study also concluded that although women with changing partners are strongly advised to use condoms to prevent sexually transmitted diseases, "a certain period of sperm exposure within a stable relation, when pregnancy is aimed for, is associated with protection against pre-eclampsia".[56]
Several other studies have since investigated the decreased incidence of pre-eclampsia in women who had received blood transfusions from their partner, those with long preceding histories of sex without barrier contraceptives, and in women who had been regularly performing oral sex.[57]
Having already noted the importance of a woman's immunological tolerance to her baby's paternal genes, several Dutch reproductive biologists decided to take their research a step further. Consistent with the fact that human immune systems tolerate things better when they enter the body via the mouth, the Dutch researchers conducted a series of studies that confirmed a surprisingly strong correlation between a diminished incidence of pre-eclampsia and a woman's practice of oral sex, and noted that the protective effects were strongest if she swallowed her partner's semen.[57][58] A team from the University of Adelaide has also investigated to see if men who have fathered pregnancies which have ended in miscarriage or pre-eclampsia had low seminal levels of critical immune modulating factors such as TGF-beta. The team has found that certain men, dubbed "dangerous males", are several times more likely to father pregnancies that would end in either pre-eclampsia or miscarriage.[55] Among other things, most of the "dangerous males" seemed to lack sufficient levels of the seminal immune factors necessary to induce immunological tolerance in their partners.[59]
As the theory of immune intolerance as a cause of pre-eclampsia has become accepted, women who with repeated pre-eclampsia, miscarriages, or in vitro fertilization failures could potentially be administered key immune factors such as TGF-beta along with the father's foreign proteins, possibly either orally, as a sublingual spray, or as a vaginal gel to be applied onto the vaginal wall before intercourse.[55]
Treatment
The definitive treatment for pre-eclampsia is the delivery of the baby and placenta. The timing of delivery should balance the desire for optimal outcomes for the baby while reducing risks for the mother.[10] The severity of disease and the maturity of the baby are primary considerations.[60] These considerations are situation-specific and management will vary with situation, location, and institution. Treatment can range from expectant management to expedited delivery by induction of labor or Caesarean section, in addition to medications. Important in management is the assessment of the mother's organ systems, management of severe hypertension, and prevention and treatment of eclamptic seizures.[10] Separate interventions directed at the baby may also be necessary. Bed rest has not been found to be useful and is thus not routinely recommended.[61]
Blood pressure
The World Health Organization recommends that women with severe hypertension during pregnancy should receive treatment with anti-hypertensive agents.[4] Severe hypertension is generally considered systolic BP of at least 160 or diastolic BP of at least 110.[3] Evidence does not support the use of one anti-hypertensive over another.[10] The choice of which agent to use should be based on the prescribing clinician's experience with a particular agent, its cost, and its availability.[4] Diuretics are not recommended for prevention of pre-eclampsia and its complications.[4] Labetalol, hydralazine and nifedipine are commonly used antihypertensive agents for hypertension in pregnancy.[6] ACE inhibitors and angiotensin receptor blockers are contraindicated as they affect fetal development.[33]
The goal of treatment of severe hypertension in pregnancy is to prevent cardiovascular, kidney, and cerebrovascular complications.[3] The target blood pressure has been proposed to be 140–160 mmHg systolic and 90–105 mmHg diastolic, although values are variable.[62]
Prevention of eclampsia
The intrapartum and postpartum administration of magnesium sulfate is recommended in severe pre-eclampsia for the prevention of eclampsia.[4][10] Further, magnesium sulfate is recommended for the treatment of eclampsia over other anticonvulsants.[4] Magnesium sulfate acts by interacting with NMDA receptors.[33]
Epidemiology
Pre-eclampsia affects approximately 2–8% of all pregnancies worldwide.[1][2][63] The incidence of pre-eclampsia has risen in the U.S. since the 1990s, possibly as a result of increased prevalence of predisposing disorders, such as chronic hypertension, diabetes, and obesity.[10]
Pre-eclampsia is one of the leading causes of maternal and perinatal morbidity and mortality worldwide.[1] Nearly one-tenth of all maternal deaths in Africa and Asia and one-quarter in Latin America are associated with hypertensive diseases in pregnancy, a category that encompasses pre-eclampsia.[4]
Pre-eclampsia is much more common in women who are pregnant for the first time.[64] Women who have previously been diagnosed with pre-eclampsia are also more likely to experience pre-eclampsia in subsequent pregnancies.[6] Pre-eclampsia is also more common in women who have pre-existing hypertension, obesity, diabetes, autoimmune diseases such as lupus, various inherited thrombophilias such as Factor V Leiden, renal disease, multiple gestation (twins or multiple birth), and advanced maternal age.[6] Women who live at high altitude are also more likely to experience pre-eclampsia.[65][66] Pre-eclampsia is also more common in some ethnic groups (e.g. African-Americans, Sub-Saharan Africans, Latin Americans, African Caribbeans, and Filipinos).[10][67] Change of paternity in a subsequent pregnancy has been implicated as affecting risk, except in those with a family history of hypertensive pregnancy.[68]
Eclampsia is a major complication of pre-eclampsia. Eclampsia affects 0.56 per 1,000 pregnant women in developed countries and almost 10 to 30 times as many women in low-income countries as in developed countries.[6]
Complications
Complications of pre-eclampsia can affect both the mother and the fetus. Acutely, pre-eclampsia can be complicated by eclampsia, the development of HELLP syndrome, hemorrhagic or ischemic stroke, liver damage and dysfunction, acute kidney injury, and acute respiratory distress syndrome (ARDS).[6][16]
Pre-eclampsia is also associated with increased frequency of Caesarean section, preterm delivery, and placental abruption. Furthermore, an elevation in blood pressure can occur in some individuals in the first week postpartum attributable to volume expansion and fluid mobilization.[16] Fetal complications include fetal growth restriction and potential fetal or perinatal death.[16]
Long-term, an individual with pre-eclampsia is at increased risk for recurrence of pre-eclampsia in subsequent pregnancies.
Eclampsia
Eclampsia is the development of new convulsions in a pre-eclamptic patient that may not be attributed to other causes. It is a sign that the underlying pre-eclamptic condition is severe and is associated with high rates of perinatal and maternal morbidity and mortality.[4] Warning symptoms for eclampsia in an individual with current pre-eclampsia may include headaches, visual disturbances, and right upper quadrant or epigastric abdominal pain, with a headache being the most consistent symptom.[10][21] Magnesium sulfate is used to prevent convulsions in cases of severe pre-eclampsia.
HELLP Syndrome
HELLP syndrome is defined as hemolysis (microangiopathic), elevated liver enzymes (liver dysfunction), and low platelets (thrombocytopenia). This condition may occur in 10–20% of patients with severe pre-eclampsia and eclampsia[10] and is associated with increased maternal and fetal morbidity and mortality. In 50% of instances, HELLP syndrome develops preterm, while 20% of cases develop in late gestation and 30% during the post-partum period.[6]
Long term
There is also an increased risk for cardiovascular complications, including hypertension and ischemic heart disease, and kidney disease.[16] Other risks include stroke and venous thromboembolism.[69][70] It seems pre-eclampsia does not increase the risk of cancer.[69]
Lowered blood supply to the fetus in pre-eclampsia causes lowered nutrient supply, which could result in intrauterine growth restriction (IUGR) and low birth weight.[18] The fetal origins hypothesis states that fetal undernutrition is linked with coronary heart disease later in adult life due to disproportionate growth.[71]
Because pre-eclampsia leads to a mismatch between the maternal energy supply and fetal energy demands, pre-eclampsia can lead to IUGR in the developing fetus.[72] Infants suffering from IUGR are prone to suffer from poor neuronal development and in increased risk for adult disease according to the Barker hypothesis. Associated adult diseases of the fetus due to IUGR include, but are not limited to, coronary artery disease (CAD), type 2 diabetes mellitus (T2DM), cancer, osteoporosis, and various psychiatric illnesses.[73]
The risk of pre-eclampsia and development of placental dysfunction has also been shown to be recurrent cross-generationally on the maternal side and most likely on the paternal side. Fetuses born to mothers who were born small for gestational age (SGA) were 50% more likely to develop pre-eclampsia while fetuses born to both SGA parents were three-fold more likely to develop pre-eclampsia in future pregnancies.[74]
History
The word "eclampsia" is from the Greek term for lightning.[12] The first known description of the condition was by Hippocrates in the 5th century BC.[12]
An outdated medical term for pre-eclampsia is toxemia of pregnancy, a term that originated in the mistaken belief that the condition was caused by toxins.[75]
References
- Eiland E, Nzerue C, Faulkner M (2012). "Preeclampsia 2012". Journal of Pregnancy. 2012: 586578. doi:10.1155/2012/586578. PMC 3403177. PMID 22848831.
- Al-Jameil N, Aziz Khan F, Fareed Khan M, Tabassum H (February 2014). "A brief overview of preeclampsia". Journal of Clinical Medicine Research. 6 (1): 1–7. doi:10.4021/jocmr1682w. PMC 3881982. PMID 24400024.
- American College of Obstetricians Gynecologists; Task Force on Hypertension in Pregnancy (November 2013). "Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy" (PDF). Obstetrics and Gynecology. 122 (5): 1122–31. doi:10.1097/01.AOG.0000437382.03963.88. PMC 1126958. PMID 24150027. Archived (PDF) from the original on 2016-01-06. Retrieved 2015-02-17.
- WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia (PDF). 2011. ISBN 978-92-4-154833-5. Archived (PDF) from the original on 2015-05-13.
- Henderson JT, Whitlock EP, O'Connor E, Senger CA, Thompson JH, Rowland MG (May 2014). "Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 160 (10): 695–703. doi:10.7326/M13-2844. PMID 24711050. S2CID 33835367.
- Arulkumaran N, Lightstone L (December 2013). "Severe pre-eclampsia and hypertensive crises". Best Practice & Research. Clinical Obstetrics & Gynaecology. 27 (6): 877–84. doi:10.1016/j.bpobgyn.2013.07.003. PMID 23962474.
- Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Hypertension in pregnancy. ACOG. 2013. p. 2. ISBN 9781934984284. Archived from the original on 2016-11-18. Retrieved 2016-11-17.
- Lambert G, Brichant JF, Hartstein G, Bonhomme V, Dewandre PY (2014). "Preeclampsia: an update". Acta Anaesthesiologica Belgica. 65 (4): 137–49. PMID 25622379.
- Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R (August 2010). "Pre-eclampsia". Lancet. 376 (9741): 631–44. doi:10.1016/S0140-6736(10)60279-6. PMID 20598363. S2CID 208792631.
- Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. (April 2017). "Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement". JAMA. 317 (16): 1661–1667. doi:10.1001/jama.2017.3439. PMID 28444286. S2CID 205091250.
- Mohler ER (2006). Advanced Therapy in Hypertension and Vascular Disease. PMPH-USA. pp. 407–408. ISBN 9781550093186. Archived from the original on 2015-10-05.
- "Pre-eclampsia". Mayo Clinic. Retrieved 21 January 2021.
- Wu J, Ren C, Delfino RJ, Chung J, Wilhelm M, Ritz B (November 2009). "Association between local traffic-generated air pollution and preeclampsia and preterm delivery in the south coast air basin of California" (PDF). Environmental Health Perspectives. 117 (11): 1773–9. doi:10.1289/ehp.0800334. PMC 2801174. PMID 20049131. Archived from the original (PDF) on 2009-07-19. Retrieved 2009-07-05.
- Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC (April 2014). "Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis". BMJ. 348: g2301. doi:10.1136/bmj.g2301. PMC 3988319. PMID 24735917.
- Mustafa R, Ahmed S, Gupta A, Venuto RC (2012). "A comprehensive review of hypertension in pregnancy". Journal of Pregnancy. 2012: 105918. doi:10.1155/2012/105918. PMC 3366228. PMID 22685661.
- Innes KE, Byers TE (November 1999). "Preeclampsia and breast cancer risk". Epidemiology. 10 (6): 722–32. doi:10.1097/00001648-199911000-00013. JSTOR 3703514. PMID 10535787.
- Chen DB, Wang W (May 2013). "Human placental microRNAs and preeclampsia". Biology of Reproduction. 88 (5): 130. doi:10.1095/biolreprod.113.107805. PMC 4013914. PMID 23575145.
- Ouyang Y, Mouillet JF, Coyne CB, Sadovsky Y (February 2014). "Review: placenta-specific microRNAs in exosomes - good things come in nano-packages". Placenta. 35 Suppl: S69-73. doi:10.1016/j.placenta.2013.11.002. PMC 3944048. PMID 24280233.
- Xie L, Mouillet JF, Chu T, Parks WT, Sadovsky E, Knöfler M, Sadovsky Y (December 2014). "C19MC microRNAs regulate the migration of human trophoblasts". Endocrinology. 155 (12): 4975–85. doi:10.1210/en.2014-1501. PMC 4239420. PMID 25211593.
- Cunningham FG, Leveno KJ, Bloom S, Gilstrap L, eds. (2010). Williams obstetrics (23rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-149701-5.
- Bartsch E, Medcalf KE, Park AL, Ray JG (April 2016). "Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies". BMJ. 353: i1753. doi:10.1136/bmj.i1753. PMC 4837230. PMID 27094586.
- Garg AX, Nevis IF, McArthur E, Sontrop JM, Koval JJ, Lam NN, et al. (January 2015). "Gestational hypertension and preeclampsia in living kidney donors". The New England Journal of Medicine. 372 (2): 124–33. doi:10.1056/NEJMoa1408932. PMC 4362716. PMID 25397608.
- van den Boogaard E, Vissenberg R, Land JA, van Wely M, van der Post JA, Goddijn M, Bisschop PH (2011). "Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: a systematic review". Human Reproduction Update (Review). 17 (5): 605–19. doi:10.1093/humupd/dmr024. PMID 21622978.
- Vissenberg R, van den Boogaard E, van Wely M, van der Post JA, Fliers E, Bisschop PH, Goddijn M (July 2012). "Treatment of thyroid disorders before conception and in early pregnancy: a systematic review". Human Reproduction Update (Review). 18 (4): 360–73. doi:10.1093/humupd/dms007. PMID 22431565. Archived from the original on 2016-01-06. Retrieved 2014-12-16.
- Drife JO, Magowan B (2004). Clinical obstetrics and gynecology. Edinburgh, New York: Saunders. pp. 367–70. ISBN 978-0-7020-1775-9.
- McMaster-Fay RA (2008). "Pre-eclampsia: a disease of oxidative stress resulting from the catabolism of DNA (primarily fetal) to uric acid by xanthine oxidase in the maternal liver; a hypothesis". Bioscience Hypotheses. 1: 35–43. doi:10.1016/j.bihy.2008.01.002.
- Laresgoiti-Servitje E, Gómez-López N, Olson DM (April 2010). "An immunological insight into the origins of pre-eclampsia". Human Reproduction Update. 16 (5): 510–24. doi:10.1093/humupd/dmq007. PMID 20388637. Archived from the original on 2020-10-04. Retrieved 2010-08-10.
- Redman CW, Sargent IL (June 2005). "Latest advances in understanding preeclampsia". Science. 308 (5728): 1592–4. Bibcode:2005Sci...308.1592R. doi:10.1126/science.1111726. PMID 15947178. S2CID 21889468.
- Davis JA, Gallup GG (2006). "Preeclampsia and other pregnancy complications as an adaptive response to unfamiliar semen)". In Platek SM, Shackelford TK (eds.). Female Infidelity and Paternal Uncertainty. Evolutionary Perspectives on Male Anti-Cuckoldry Tactics. Cambridge University Press. pp. 191–204. doi:10.1017/CBO9780511617812.010. ISBN 9780511617812.
- Fu ZM, Ma ZZ, Liu GJ, Wang LL, Guo Y (January 2018). "Vitamins supplementation affects the onset of preeclampsia". Journal of the Formosan Medical Association = Taiwan Yi Zhi. 117 (1): 6–13. doi:10.1016/j.jfma.2017.08.005. PMID 28877853.
- Matthiesen L, Berg G, Ernerudh J, Ekerfelt C, Jonsson Y, Sharma S (2005). "Immunology of preeclampsia". Chemical Immunology and Allergy. 89: 49–61. doi:10.1159/000087912. ISBN 978-3-8055-7970-4. PMID 16129952.
- Longo DL (2012). Harrison's principles of internal medicine. New York: McGraw-Hill. pp. 55–61. ISBN 978-0-07-174889-6.
- Rolnik, D. L.; Wright, D.; Poon LCY; Syngelaki, A.; O'Gorman, N.; De Paco Matallana, C.; Akolekar, R.; Cicero, S.; Janga, D.; Singh, M.; Molina, F. S.; Persico, N.; Jani, J. C.; Plasencia, W.; Papaioannou, G.; Tenenbaum-Gavish, K.; Nicolaides, K. H. (2017). "ASPRE trial: Performance of screening for preterm pre-eclampsia". Ultrasound in Obstetrics & Gynecology. 50 (4): 492–495. doi:10.1002/uog.18816. PMID 28741785. S2CID 24728853.
- Poon, Liona C.; Shennan, Andrew; Hyett, Jonathan A.; Kapur, Anil; Hadar, Eran; Divakar, Hema; McAuliffe, Fionnuala; Silva Costa, Fabricio; Dadelszen, Peter; McIntyre, Harold David; Kihara, Anne B.; Di Renzo, Gian Carlo; Romero, Roberto; d'Alton, Mary; Berghella, Vincenzo; Nicolaides, Kypros H.; Hod, Moshe; Hanson, Mark; Ma, Ronald; Purandare, CN; Fuchtner, Carlos; Visser, Gerard; Morris, Jessica; Gooden, Rachel (2019). "The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre‐eclampsia: A pragmatic guide for first‐trimester screening and prevention". International Journal of Gynecology & Obstetrics. 145: 1–33. doi:10.1002/ijgo.12802. PMC 6944283. PMID 31111484.
- Craici IM, Wagner SJ, Bailey KR, Fitz-Gibbon PD, Wood-Wentz CM, Turner ST, et al. (June 2013). "Podocyturia predates proteinuria and clinical features of preeclampsia: longitudinal prospective study". Hypertension. 61 (6): 1289–96. doi:10.1161/HYPERTENSIONAHA.113.01115. PMC 3713793. PMID 23529165.
- "Pre-eclampsia predicted using test during pregnancy". BBC News. 2011-11-12. Archived from the original on 2011-11-18. Retrieved 2011-11-22.
- Brown CM, Garovic VD (October 2011). "Mechanisms and management of hypertension in pregnant women". Current Hypertension Reports. 13 (5): 338–46. doi:10.1007/s11906-011-0214-y. PMC 3746761. PMID 21656283.
- "Pre-eclampsia-Eclampsia". Diagnosis and management of pre-eclampsia and eclampsia. Armenian Medical Network. 2003. Retrieved 2005-11-23.
- Ota E, Hori H, Mori R, Tobe-Gai R, Farrar D (June 2015). "Antenatal dietary education and supplementation to increase energy and protein intake". The Cochrane Database of Systematic Reviews (6): CD000032. doi:10.1002/14651858.CD000032.pub3. PMID 26031211.
- Duley L, Henderson-Smart D, Meher S (October 2005). "Altered dietary salt for preventing pre-eclampsia, and its complications". The Cochrane Database of Systematic Reviews (4): CD005548. doi:10.1002/14651858.CD005548. PMID 16235411.
- Rumbold AR, Crowther CA, Haslam RR, Dekker GA, Robinson JS (April 2006). "Vitamins C and E and the risks of preeclampsia and perinatal complications" (PDF). The New England Journal of Medicine. 354 (17): 1796–806. doi:10.1056/NEJMoa054186. hdl:2440/23161. PMID 16641396.
- WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. 2011. ISBN 978-92-4-154833-5.
- Hofmeyr GJ, Lawrie TA, Atallah ÁN, Torloni MR (October 2018). "Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems". The Cochrane Database of Systematic Reviews. 10: CD001059. doi:10.1002/14651858.CD001059.pub5. PMC 6517256. PMID 30277579.
- Rayman MP, Bode P, Redman CW (November 2003). "Low selenium status is associated with the occurrence of the pregnancy disease preeclampsia in women from the United Kingdom" (PDF). American Journal of Obstetrics and Gynecology. 189 (5): 1343–9. doi:10.1067/S0002-9378(03)00723-3. PMID 14634566. Archived (PDF) from the original on 2018-07-20. Retrieved 2019-06-30.
- Liu T, Zhang M, Guallar E, Wang G, Hong X, Wang X, Mueller NT (August 2019). "Trace Minerals, Heavy Metals, and Preeclampsia: Findings from the Boston Birth Cohort". Journal of the American Heart Association. 8 (16): e012436. doi:10.1161/JAHA.119.012436. PMC 6759885. PMID 31426704.
- Duley, L; Meher, S; Hunter, KE; Seidler, AL; Askie, LM (30 October 2019). "Antiplatelet agents for preventing pre-eclampsia and its complications". The Cochrane Database of Systematic Reviews. 2019 (10). doi:10.1002/14651858.CD004659.pub3. PMC 6820858. PMID 31684684.
- "Low-Dose Aspirin Use for the Prevention of Morbidity and Mortality From Preeclampsia". United States Preventive Services Task Force. Sep 2014. Archived from the original on 17 September 2014. Retrieved 17 Sep 2014.
- Roberge S, Nicolaides K, Demers S, Hyett J, Chaillet N, Bujold E (February 2017). "The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis". American Journal of Obstetrics and Gynecology. 216 (2): 110–120.e6. doi:10.1016/j.ajog.2016.09.076. PMID 27640943. S2CID 3079979.
- Rolnik, D. L.; Wright, D.; Poon LCY; Syngelaki, A.; O'Gorman, N.; De Paco Matallana, C.; Akolekar, R.; Cicero, S.; Janga, D.; Singh, M.; Molina, F. S.; Persico, N.; Jani, J. C.; Plasencia, W.; Papaioannou, G.; Tenenbaum-Gavish, K.; Nicolaides, K. H. (2017). "ASPRE trial: Performance of screening for preterm pre-eclampsia". Ultrasound in Obstetrics & Gynecology. 50 (4): 492–495. doi:10.1002/uog.18816. PMID 28741785. S2CID 24728853.
- Meher S, Duley L (April 2006). Meher S (ed.). "Exercise or other physical activity for preventing pre-eclampsia and its complications". The Cochrane Database of Systematic Reviews (2): CD005942. doi:10.1002/14651858.CD005942. PMID 16625645.
- Meher S, Duley L (April 2006). Meher S (ed.). "Rest during pregnancy for preventing pre-eclampsia and its complications in women with normal blood pressure". The Cochrane Database of Systematic Reviews (2): CD005939. doi:10.1002/14651858.CD005939. PMC 6823233. PMID 16625644.
- Jeyabalan A, Powers RW, Durica AR, Harger GF, Roberts JM, Ness RB (August 2008). "Cigarette smoke exposure and angiogenic factors in pregnancy and preeclampsia". American Journal of Hypertension. 21 (8): 943–7. doi:10.1038/ajh.2008.219. PMC 2613772. PMID 18566591.
- Whitworth M, Dowswell T (October 2009). "Routine pre-pregnancy health promotion for improving pregnancy outcomes". The Cochrane Database of Systematic Reviews (4): CD007536. doi:10.1002/14651858.CD007536.pub2. PMC 4164828. PMID 19821424.
- Robertson SA, Bromfield JJ, Tremellen KP (August 2003). "Seminal 'priming' for protection from pre-eclampsia-a unifying hypothesis". Journal of Reproductive Immunology. 59 (2): 253–65. doi:10.1016/S0165-0378(03)00052-4. PMID 12896827.
- Dekker GA, Robillard PY, Hulsey TC (June 1998). "Immune maladaptation in the etiology of preeclampsia: a review of corroborative epidemiologic studies". Obstetrical & Gynecological Survey. 53 (6): 377–82. doi:10.1097/00006254-199806000-00023. PMID 9618714.
- Bonney EA (December 2007). "Preeclampsia: a view through the danger model". Journal of Reproductive Immunology. 76 (1–2): 68–74. doi:10.1016/j.jri.2007.03.006. PMC 2246056. PMID 17482268.
- Mattar R, Soares RV, Daher S (February 2005). "Sexual behavior and recurrent spontaneous abortion". International Journal of Gynaecology and Obstetrics. 88 (2): 154–5. doi:10.1016/j.ijgo.2004.11.006. PMID 15694097. S2CID 37475639.
- Dekker G (2002). "The partner's role in the etiology of preeclampsia". Journal of Reproductive Immunology. 57 (1–2): 203–15. doi:10.1016/S0165-0378(02)00039-6. PMID 12385843.
- Beckmann CR, Ling FW, Smith RP, Barzansky BM, Herbert WN, Laube DW, American Congress of Obstetricians and Gynecologists, eds. (2010). Obstetrics and gynecology (6th ed.). Baltimore, MD: Lippincott Williams & Wilkins. ISBN 978-0781788076.
- McCall CA, Grimes DA, Lyerly AD (June 2013). ""Therapeutic" bed rest in pregnancy: unethical and unsupported by data". Obstetrics and Gynecology. 121 (6): 1305–8. doi:10.1097/aog.0b013e318293f12f. PMID 23812466. S2CID 9069311.
- Hypertensive Disorders in Pregnancy. Version 2.0. Archived 2016-03-06 at the Wayback Machine at Nederlandse Vereniging voor Obstetrie en Gynaecologie. Date of approval: 20-05-2005
- World Health Organization (WHO). World health report 2005: make every mother and child count. Geneva: WHO; 2005, p. 63
- Robbins and Cotran, Pathological Basis of Disease, 7th ed.
- Keyes LE, Armaza JF, Niermeyer S, Vargas E, Young DA, Moore LG (July 2003). "Intrauterine growth restriction, preeclampsia, and intrauterine mortality at high altitude in Bolivia". Pediatric Research. 54 (1): 20–5. doi:10.1203/01.PDR.0000069846.64389.DC. PMID 12700368. S2CID 25586771.
- Moore LG, Shriver M, Bemis L, Hickler B, Wilson M, Brutsaert T, et al. (April 2004). "Maternal adaptation to high-altitude pregnancy: an experiment of nature--a review" (PDF). Placenta. 25 Suppl A: S60-71. doi:10.1016/j.placenta.2004.01.008. PMID 15033310. Archived from the original (PDF) on 2016-08-17. Retrieved 2016-06-14.
- Urquia ML, Glazier RH, Gagnon AJ, Mortensen LH, Nybo Andersen AM, Janevic T, et al. (November 2014). "Disparities in pre-eclampsia and eclampsia among immigrant women giving birth in six industrialised countries". BJOG. 121 (12): 1492–500. doi:10.1111/1471-0528.12758. PMC 4232918. PMID 24758368.
- Hjartardottir S, Leifsson BG, Geirsson RT, Steinthorsdottir V (2004). "Paternity change and the recurrence risk in familial hypertensive disorder in pregnancy". Hypertension in Pregnancy. 23 (2): 219–25. doi:10.1081/PRG-120037889. PMID 15369654. S2CID 8936562.
- Bellamy L, Casas JP, Hingorani AD, Williams DJ (November 2007). "Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis". BMJ. 335 (7627): 974. doi:10.1136/bmj.39335.385301.BE. PMC 2072042. PMID 17975258.
- McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ (November 2008). "Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses". American Heart Journal. 156 (5): 918–30. doi:10.1016/j.ahj.2008.06.042. PMID 19061708.
- Barker DJ (July 1995). "Fetal origins of coronary heart disease". BMJ. 311 (6998): 171–4. doi:10.1136/bmj.311.6998.171. PMC 2550226. PMID 7613432.
- Sharma D, Shastri S, Sharma P (2016). "Intrauterine Growth Restriction: Antenatal and Postnatal Aspects". Clinical Medicine Insights. Pediatrics. 10: 67–83. doi:10.4137/CMPed.S40070. PMC 4946587. PMID 27441006.
- Calkins K, Devaskar SU (July 2011). "Fetal origins of adult disease". Current Problems in Pediatric and Adolescent Health Care. 41 (6): 158–76. doi:10.1016/j.cppeds.2011.01.001. PMC 4608552. PMID 21684471.
- Wikström AK, Svensson T, Kieler H, Cnattingius S (November 2011). "Recurrence of placental dysfunction disorders across generations". American Journal of Obstetrics and Gynecology. 205 (5): 454.e1–8. doi:10.1016/j.ajog.2011.05.009. PMID 21722870.
- "Toxemia of pregnancy | medical disorder". Encyclopedia Britannica. Archived from the original on 2014-03-28. Retrieved 2013-06-28.
External links
- Pre-eclampsia at Curlie
- MedlinePlus entry on high blood pressure in pregnancy
- Mayo Clinic fact sheet on pre-eclampsia
| Classification |
|---|
